Achilles Tendinopathy
Achilles tendon injuries are a common problem in both active and sedentary individuals of all ages.
Classification
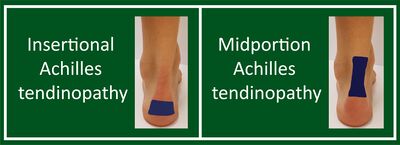
There are two location-based patterns of Achilles tendionpathy
- Mid-portion Achilles tendinopathy - the pain occurs between 2-7cm above the superior aspect of the calcaneum
- Insertional Achilles tendinopathy - the pain occurs within the first 2cm of the insertion point on the calcaneum. There may be a tendinopathy of the Achilles tendon insertion, and associated Haglund deformity and/or an associated retrocalcaneal bursitis.
Clinical Features
In general, history and physical exam features are better at ruling in, rather than ruling out achilles tendinopathy. Self reported morning stiffness is the only feature with a moderate negative likelihood ratio.
| Test | Sens. | Spec. | LR+ | LR- | K |
|---|---|---|---|---|---|
| Palpation (tenderness) | 64% | 81% | 3.15 | 0.48 | |
| Arc Sign | 42% | 88% | 3.24 | 0.68 | |
| Royal London Hospital Test |
54% | 86% | 3.84 | 0.54 | |
| Morning stiffness | 89% | 58% | 2.12 | 0.19 | |
| Palpation thickening | 59% | 90% | 5.9 | 0.46 | |
| Crepitus | 3% | 100% | inf | 0.97 | |
| Stretch on passive dorsiflexion with knee joint in flexion |
13% | 87% | 1.00 | 1.00 | |
| Single legged heel raise | 22% | 93% | 3.14 | 0.95 | |
| Hop test | 43% | 87% | 3.31 | 0.66 | |
| Thompson test (for rupture) |
- Palpation: Palpate midportion and insertion
- Royal London Hospital Test: Pain on palpation disappears on maximal dorsiflexion compared to plantarflexion in achilles tendinopathy
- Arc test: palpate for thickened part/nodule, then have patient move ankle. In achilles tendinopathy the nodule should move, if it does not move then consider paratendonitis. Paratendonitis may show swelling.
- Modified straight leg raise for assessing sural nerve neuropathy: bring ankle into dorsiflexion and inverison, then flex the hip.
- Posterior impingement: passively hyperplantarflex the ankle looking for pain provocation.
- Plantaris tendinopathy: medial pain as the plantaris compresses against the medial achilles tendon
- Accessory/low soleus: can lead to compartment syndrome like symptoms e.g. symptoms settle quickly after the patient stops running
Diagnosis
Diagnosing achilles tendinopathy follows the same overarching assessment principles as other lower limb tendinopathies.
- Localised symptoms at relevant portion (insertion or midportion)
- Proportional pain-load relationship
- Pain onset 24 hours after high and fast load activities
- Every stage perform a couple of repetitions and gauge pain. Start with walking or running to assess the pain, double calf raises on the ground, double calf raises on a step, single leg calf raises, single leg knee bent calf raises, add load if required, add speed to calf raises with knee bent, hopping double leg, hopping single leg, hopping forward, backwards, sideways, jumps for maximal height with single leg.
- Local thickening of the relevant portion.
- Pain on local palpation of the relevant portion.
- Hallmark signs
- Morning stiffness, this is the most sensitive sign.
- Often have pain after arising from sitting.
- Muscle Wasting.
Differential Diagnosis
- Midportion Achilles Tendinopathy
- Insertional Achilles Tendinopathy
- Retrocalcaneal bursitis
- Paratenon inflammation
- Posterior impingement syndrome
- Plantaris Tendinopathy
- Sever Disease (Calcaneal Apophysitis)
- Accessory or low soleus muscle
- Referred Pain (neural structures, lumbar spine), and sural neuropathy
- Achilles tendon rupture
- Achilles enthesopathy due to inflammatory arthropathies
- Osteochondritis dissecans (posterior medial talus)
Imaging
Plain films in insertional Achilles tendinopathy may show calcification or Haglund deformity.
Ultrasound is the preferred imaging modality which has the following typical findings, but may not be correlated with symptoms:
- Tendon thickening (increased AP diameter)
- Altered tendon pattern (altered echogenicity)
- Neovascularisation
MRI is usually not done but can be used if there is a discrepancy between the ultrasound results and the clinical findings, or if an additional specific diagnosis is suspected which can't be detected on ultrasound.
Imaging cannot give information related to response to treatment or prognosis.
Treatment
First Line
Education: that it is a degenerative condition that will take many months to resolve but a significant portion of patients will have long term symptoms. Address psychosocial factors.
Loading advice: temporary avoidance of painful sporting activities. Encourage non-provocative replacement activities for example cycling, walking, swimming, or low-impact aerobic gym activities. The patient should start slowly and build up gradually. They can adjust activities based on pain.
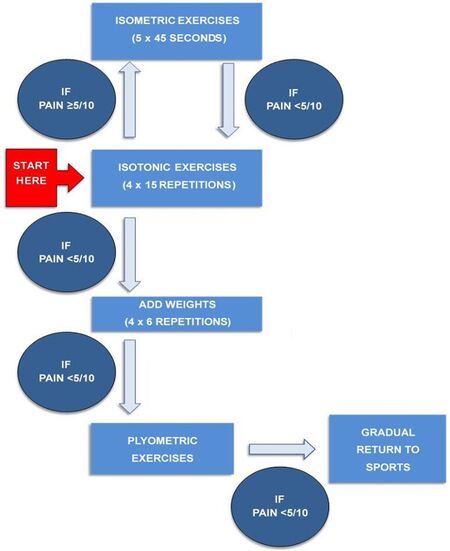
Progressive calf muscle strengthening: Graded loading programme based around calf muscle strengthening for 12 weeks. Insertional Achilles tendinopathy exercises can be done on a flat surface to avoid compressing the anterior surface of the distal Achilles against the posterior calcaneum. Be guided by pain levels, if pain is more than 5/10 go back a level, if it is less than 5/10 progress.
- Isometric exercises (5 x 45 seconds)
- Isotonic exercises (4 x 15 reps)
- Isotonic exercises with added weight (4 x 6 reps)
- Plyometric exercises
- Return to sport
Second Line
If there is no improvement after three months of patient education, structured exercise therapy, and loading advice then discuss other options. However explain that the evidence is very poor.
- Night splint
- Orthotics or heel raise
- Injections (lidocaine, autologous blood, PRP, hyaluronic acid, prolotherapy). Avoid corticosteroid injections.
- Extracorporeal shockwave therapy
- Surgery
Prognosis
The majority of patients recover, But 23-37% have persisting pain for at least 10 years despite treatment.[1]
Resources
See Also
- Tendinopathy
- Dutch multidisciplinary guideline on Achilles tendinopathy (open access)[1]
- Achilles Tendon Differential Diagnosis | Physio Network (physio-network.com)
References
- ↑ 1.0 1.1 1.2 de Vos RJ, van der Vlist AC, Zwerver J, Meuffels DE, Smithuis F, van Ingen R, van der Giesen F, Visser E, Balemans A, Pols M, Veen N, den Ouden M, Weir A. Dutch multidisciplinary guideline on Achilles tendinopathy. Br J Sports Med. 2021 Oct;55(20):1125-1134. doi: 10.1136/bjsports-2020-103867. Epub 2021 Jun 29. PMID: 34187784; PMCID: PMC8479731.