Acute Neck Pain
Acute neck pain is largely a benign condition, however the clinician should not be complacent as a rare number have a sinister cause, and a portion go on to develop chronic pain.
Aetiology
- Main article: Causes and Sources of Neck Pain
The causes of common acute neck pain are largely unknown, however any structure in the cervical spine that is innervated is a potential source of pain. Importantly, cervical spondylosis is not a legitimate cause of neck pain. Serious and identifiable causes of neck pain - infections, fractures, tumours, dissection - are rare, but vigilance is required to detect them. Many review articles and textbooks list things like neurological and rheumatological conditions, but in these conditions there is usually another give away and so they are not generally part of the true differential of isolated acute neck pain.
The major aetiological risk factors for neck pain are educational level, occupation, previous injury, working with machines, and stress at work. Psychological factors are not major risk factors.[1]
Clinical Assessment
- Significant trauma (eg. fall in osteoporotic patient, motor vehicle accident)
- Infective: (eg. fever, meningism, immunosuppression, intravenous drug use, exotic exposure, recent overseas travel)
- Constitutional: (eg. fevers, weight loss, anorexia, past or current history of malignancy)
- Iatrogenic: Recent surgery, catheterisation, venipuncture, manipulation
- Neurological: Symptoms/signs especially of upper motor neuron pathology, vomiting
- Genitourinary/Reproductive: UTI, haematuria, retention, uterine, breast
- Endocrine: Corticosteroids, diabetes, hyperparathyroid
- Gastrointestinal: Dysphagia
- Integumentary: Infections, rashes
- Cardiorespiratory: Cough, haemoptysis, chest pain, shortness of breath, diaphoresis, ripping/tearing sensation (dissection), CVD risk factors, anticoagulants
- Rheumatological: History of rheumatoid arthritis (atlanto-axial disruption)
- Awkward posture (atlantoaxial rotatory subluxation in children)
It is rarely possible to establish a patho-anatomic diagnosis in acute neck pain, and so the diagnostic process is one of exclusion.
The first step is evaluating whether the patient has neurological symptoms or signs. If they do then they should be assessed under a neurological disorders framework rather than an acute neck pain framework as the neurological disorder takes precedence. Neurological disorders include spinal cord injury, myelopathy, and radiculopathy.
With longitudinal care, the practitioner should remain vigilant to new clues that invites revisiting the diagnosis. Vigilance includes revisiting red flag symptoms and noting any new symptoms or signs.
History
The location of pain is important. The clinician should be familiar with the definitions of neck pain. Anterior neck pain is not usually related to disorders of the cervical spine and requires a different framework. The presence of headache invites consideration of whether there is pain referring from the neck to the head, or from the head to the neck. Neck pain can refer to the chest and vice versa. However if the primary disorder lies in the heart or thoracic aorta, then usually the chest pain is worse than the neck pain. Also there may be other associated symptoms such as diaphoresis, distress, cyanosis, or abnormal vital signs.
There may be a well defined area of pain, and this location can be used to make an assessment as to the segmental nociceptive origin. Pain in the upper half of the neck is usually from the upper cervical segments (C2-3 most commonly), and pain in the lower half of the neck is usually from the lower cervical segments (C5-6 most commonly). The approximate segmental location may be able to be determined if there is a localised pattern of pain radiation. The patient should be asked where they feel the pain at its worst. More emphasis should be placed on the "core" or "centroid" location of pain over the total extent of the pain referral boundaries. The information can be correlated to cervical pain maps, for example pain maps in asymptomatic patients, or symptomatic patients. This information can be used to approximate the segment, but not the structure. This is because discs, facet joints, and muscles all have a similar segmental pain referral pattern.
| Segment | Pain Pattern |
|---|---|
| C2-3 | Suboccipital area, may radiate into the occiput or forehead |
| C3-4 | Posterolateral neck, approximately over the course of the levator scapula |
| C4-5 | Angle between neck and top of shoulder girdle |
| C5-6 | Supraspinatus fossa, radiates to the deltoid region |
| C6-7 | Medial border of the scapula |
Arm pain may be due to somatic referred pain or radicular pain. Distinguishing these is not always straight forward.
- Somatic referred pain is deep, aching, and is sometimes felt as an expanding pressure that spreads into the upper limb. It usually only radiates no further distal than the shoulder girdle or upper limb. Distal referral is still possible but this has only been shown in studies of noxious stimulation in normal subjects. There are no neurological signs in somatic referred pain.
- Radicular pain is also felt in the shoulder girdle and proximal upper limb. However it more often extends more distally into the forearm and hand, especially with C6 or C7 involvement. There may be an associated radiculopathy, i.e. paraesthesias, numbness, weakness, and reduced reflexes, in a dermatomal or myotomal distribution.
The duration of illlness should be ascertained. This allows classification into acute or chronic pain and can guide treatment recommendations.
Ask about the circumstances of onset, with particular respect to trauma. A spontaneous onset of pain should lead to more careful enquiry about red flag conditions. With any trauma, ask about whether it was an external force, or an inertial/indirect force. The likelihood of fracture is greater with external forces, and the risk increases the greater the force. Recent surgery, instrumentation, skin penetration, or infection elsewhere in the body may raise the risk of spinal infection. Prolonged neck rotation or extension, or recent spinal manipulation raise the risk of vascular disorders. The mode of onset relates to how quickly the pain came on. Sudden onset of pain may be concerning for serious conditions. Acute inflammation may present as a gradual onset of pain up to a few days with a subsequent rapid worsening or pain. Of note, osteomyelitis has a very slow and quiet pain onset, and the diagnosis is often delayed by many months.
The quality of pain is often dull, aching, or pressure-like, and is suggestive of somatic pain. Any shooting or lancinating pain is indicative of a neurogenic pain origin, however neck pain is rarely neurogenic (contrasted to radicular arm pain). The severity of pain cannot be relied upon, however sudden onset of severe pain may suggest a serious condition. Otherwise the severity is more useful as baseline data to compare to later.
The frequency of pain is not generally helpful; the pain is generally constant, with any periodicity typically relating to aggravating factors. The duration of pain, different to duration of illness, means how long does the pain last for when it starts. Paroxysmal pain is highly suggestive of neurogenic pain, although again neck pain is only rarely neurogenic. The time of onset is most relevant with respect to sleep. Any pain at night may suggest a serious condition.
Precipitating and aggravating factors should be asked about. Any extreme apprehension or caution for certain neck movements raises concern for instability. Avoiding neck rotation can be a symptom of atlanto-axial instability such as with odontoid fractures or with alar ligament tears. Aggravating factors are common, any any lack of such factors can indicate a vascular or vertebral body lesion. Relieving factors may be useful diagnostically when they are absent as it raises suspicion of a sinister condition. Some patients with benign causes of pain may describe their pain in an exaggerated manner. However normally patients with a serious cause of pain look ill and are comparatively silent about their pain.
The systems review evaluates any associated features. Enquire about past history of illness (e.g. cancer, diabetes, HIV, etc), weight loss, fever, night sweats, recent travel, numbness, weakness, headache, vomiting, disturbances in vision/speech/balance, cardiovascular disease risk factors, anticoagulant use, urinary frequency and dysuria, steroid use, dysphagia, pain in other regions, skin rashes, breast or uterine disorders, and respiratory disorders. See red flags box.
Physical Examination
A medical examination of the neck may be required. This may include temperature measurement which is present in 42% of patients with spinal infection, Kernig's sign for meningeal irritation, palpation of the anterior neck for masses and lymphadenopathy, palpation of the common carotid artery for carotidynia, and evaluation of horner's syndrome as a presenting feature of internal carotid artery dissection. A screening neurological examination may be indicated. In the presence of neurological symptoms or significant trauma then a more systematic neurological examination should be performed including assessment for papillooedema.
For the musculoskeletal examination, start with inspection. Evaluate for rashes, pigmentation, deformities, torticollis, and neck posture. The most common postural "fault" is forward head posture, meaning forward displacement of the head in relation to the shoulder. Forward head posture is associated with reduced cervical range of motion, but it is controversial whether it is related to neck pain. One study found an association in adults under 50 years old.[2]
Palpate looking for tenderness. The reliability for muscle tenderness ranges has a wide range depending on the area tested. Reliability for articular pillar tenderness is reasonably good (kappa 0.68, 95% CI 0.49-0.89). The diagnostic validity of articular pillar tenderness as it pertains to pinpointing the painful structure is unknown. However it does distinguish patients with neck pain from those without neck pain (sensitivity 82%, specificity 79%, +LR 3.9). "Trigger points" cannot be reliably differentiated from tenderness of the underlying facet joints, and any diagnosis of "cervical trigger point" is problematic.
Range of motion should be assessed. When looking for restriction, reliability is mixed depending on the study. Range of motion testing for restriction lacks validity - there are no data showing that a particular type of restriction signifies a specific source of pain. Range of motion can also be assessed with looking for reproduction of pain with certain tests - flexion-extension test, rotation with overpressure, foramen closure test, and the brachial plexus tension test. However the research has only shown that these tests are positive in patients with neck pain over those without neck pain, rather than looking at whether they signify a specific diagnosis. Segmental motion can be assessed, however this is a very difficult skill to master, and it is likely that it only has validity in a very select number of clinicians[3], and the reliability is poor overall.
Overall a musculoskeletal neck examination should be performed, but it should be kept in mind that it variable reliability, and lacks validity other than being able to distinguish those with and without neck pain rather than being able to find the cause of the pain. Any lack of tenderness can be a useful sign in that it can signify a non-musculoskeletal cause of neck pain such as artery dissection. Otherwise the examination has a strong social and cultural element and conveys care and consideration to the patient.
Imaging
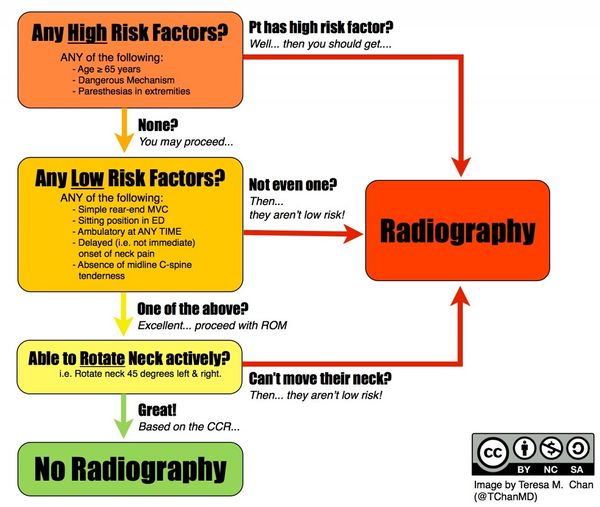
In the event of trauma, the Canadian C-spine rule should be used to determine whether imaging is required, and any fracture managed as appropriate. An AP, lateral, and open-mouth views are sufficient for exclusion of fracture. In the elderly, diagnosis of fracture can be difficult due to degenerative changes, and so many clinicians in New Zealand instead request a CT scan of the cervical spine in these patients. MRI is not indicated for primary screening in uncomplicated neck pain. In the absence of trauma, neurological signs, or features of infection on clinical assessment, there is no indication for cervical spine radiography.
Diagnosis
For patients with no history of injury the diagnosis used by the Australian Acute Musculoskeletal Guidelines is "idiopathic neck pain," while for those with neck pain following a motor vehicle accident the diagnosis is "whiplash-associated neck pain." For ACC medicolegal purposes the coding that should be used is normally "cervical sprain," but this is not a meaningful label in a medical sense as it lacks legitimacy as a diagnosis.
Management
Passive Treatment
Bogduk recommends, writing in 2006, to avoid passive therapy. He states that it is not significantly more effective than other methods. Passive management assumes that a specific diagnosis has been made, and that passive treatment will rectify said diagnosis. However no conventional examination or investigation can identify the pathology and no conventional treatment can target or resolve any specific cause of pain.
In a randomised controlled trial of patients with neck pain for at least two weeks (most patients less than 13 weeks), once weekly manual therapy (muscular mobilisation, specific articular mobilisation, coordination or stabilisation) was more clinically effective and more cost effective than twice weekly physiotherapy (individualised exercise therapy, including active and postural or relaxation exercises, stretching, and functional exercises) and continued general practitioner care (explanation, home exercises, reassurance, medication) over six weeks.[4][5] At 7 weeks, 68.3% of patients in the manual therapy group reported resolved or much improved pain, compared with 50.8% of patients in the physical therapy group and 35.9% of patients in the continued care group. This equates to an NNT of 5.7 of manual therapy over exercise therapy, and an NNT of 3 over general practitioner care. Longitudinal follow up showed that the treatment effect was lost by weeks 13 and 52.[6]. Interestingly, this effect occurred despite there being more patients with chronic pain in the manual therapy and physiotherapy groups than the continued care group (30%, 28.8%, and 18.8% respectively). The study has been criticised for using "perceived recovery" as the primary outcome measure. Also the manual therapy group averaged six visits, versus two visits for GP care, and so the greater success could be due to the increased intensity of patient-therapist interactions.
A systematic review stated that due to heterogeneity, no definite conclusions could be made.[7]
Explanation and Reassurance
These often go together. Elicit the patient's ideas and concerns. Gently correct false beliefs and address any fears about serious causes or about the prognosis. A clinical assessment can effectively rule out sinister causes and so the clinician can provide reassurance based on sound evidence. The patient may not have any specific concerns or fears. Regardless the clinician should fully reassure the patient that serious causes of neck pain are rare and can be recognised on clinical assessment, and common causes are not threatening and have a good prognosis.
Reassure the patient that the severity of pain is greater than the amount of tissue injury. If there is imaging available that shows degenerative changes, reassure the patient that these abnormalities are commonly found in asymptomatic people, and that they will have been present long before the pain onset.
The clinician should be truthful that in the majority of cases no one knows what causes the pain, that it is probably something simple like a sprain or sore muscles, but that there is no simple way to make an exact diagnosis. Explain that even without treatment most patients recover, and that the most effective treatment is a tincture of time. However offer other measures as below to help the process along.
Activation
Encourage the patient to maintain activity as near to normal as possible. This is critical for preventing disability. Identify any barriers to achieving this, and be prepared to suggest alternative ways of maintaining activity levels if pain impedes this. Reassure the patient that there is no injury that will be worsened by resuming activity, and no injury that requires rest. Explain that rest can leads to stiffness and that the neck should be allowed to heal in a way that allows normal function. Resuming activities reminds the neck what is expected of it. In some cases there will need to be goal setting in that the patient should start with a short time engaged in activity and gradually progress the length of engagement. Other interventions may be used to reduce pain to allow activation.
One study found no benefit to work-site ergonomic intervention for spinal pain.[8] While there is often a discussion around posture in the consultation, the notion of there being an "optimal" posture is not supported by the evidence for improving outcomes. A common description of a neutral posture is sitting straight with the top of the head tall, chin slightly tilted down, shoulders down, the scapula retracted and depressed, regular diaphragmatic breathing, screen at neutral eye level, and elbows at 90 degrees. While the "bad" posture is often described as elevation and rounding of the shoulders, craning the neck forward, and intermittent breath-holding. The counter argument to a single neutral posture, is that frequent position changes allows changes in joint position, muscle length, and blood flow to the cervical spine. Patients should probably limit prolonged activities including sitting, telephone use, and fine motor handwork. Patients who sit for prolonged periods at work should get up frequently throughout the day and move their neck. If patients carry heavy equipment then this may need to be addressed.
Adjusting the patients sleep position may be helpful in some cases. Encourage the patient to have their head and neck be aligned with the rest of their body. For back sleepers, ask the patient to try sleeping with their thighs elevated on pillows and a small pillow under their head and neck. For side sleepers, it may be beneficial to use a larger pillow or multiple pillows to maintain cervical spine alignment. Try rolling up a hand-towel and placing it inside the pillow case to create an edge that matches the curve of the neck. In those with radicular pain avoid cervical extension.
Outside of work and sleep there may be other factors that can be modified. For example if the patient struggles to turn their head while driving encourage the use of mirrors. If hanging up the washing is problematic, then recommend that the patient hang the washing down by lowering the clothes line or standing on a stool.
Simple Exercises
Exercises for keeping the neck moving may be the single most effective measure for treatment of acute neck pain. They encourage resumption of normal activities, they have a therapeutic measure, and they are an active rather than passive modality that allows patients to become active participants in their own care. Patients are empowered to be the vehicles for their own recovery, and treatment can be applied when convenient. The patient should engage in the exercises at certain times of the day. Timing can be attached to other activities such as meal times, getting up in the morning, and going to bed at night. The objective is to increase and maintain mobility rather than strengthening the muscles or treating a specific lesion. Encourage the patient to warm up their neck prior to the exercises for example with a wheat bag, hot water bottle, hot shower or bath.
There are a couple of New Zealand publications that can be helpful
- McKenzie RA. Treat your own Neck. Spinal Publications, Waikanae, New Zealand, 1983.
- Mulligan B. Self treatments for back, neck and limbs. Plane View Services, Wellington, 2012.
An example of a home exercise program done with 10-15 repetitions as tolerated 2-4 times daily:
- Neck rotation - Turn the head to the side and provide slight overpressure for a few seconds, repeat on the other side.
- Neck lateral flexion – Tilt the head to the side, try to touch the ear to the shoulder, and apply slight overpressure for a few seconds. Repeat on the other side..
- Neck flexion – Seated or supine, bring the chin down to the chest with the out-breath, hold for a few seconds.
- Shoulder rolls – Seated, slowly swing the arms backwards and try to bring the scapulae together. Then swing them forward. Repeat in a rhythmic motion.
- Scapular retraction – Seated, position the head in a neutral position, and bring the shoulders and scapulae backwards. Hold the position for 10 seconds.
- Deep neck flexor strengthening – Supine, draw the chin down and inwards actively contracting the anterior neck muscles. Hold for five seconds.
- Anterior chest wall stretches – Standing in a doorway, abduct the arms and place the elbows against the door frame slightly lower than shoulder height. Lean forward to create a stretch of the anterior shoulder and chest muscles. Hold for 10-30 seconds.
Alternatively if the clinician does not have sufficient knowledge or experience to teach exercises, then they may wish to refer them to a colleague or allied health provider. The referral should be for active treatment modalities rather than passive therapy.
Follow up can be offered to check compliance and understanding. The patient may wish to continue the exercises after pain resolution, but there is no evidence to support this recommendation.
Analgesia
There is no evidence that any specific analgesic is effective for acute neck pain. The Australian Acute Musculoskeletal Pain Guidelines recommend the use of paracetamol, but this is based on consensus. NSAIDs have not been shown to be more effective than paracetamol, and compound analgesics (paracetamol plus codeine) are only marginally better than paracetamol alone. Opioids are not generally recommended.
Follow up
Early review should be offered if the patient is distressed. And if not then review may be warranted following a week or so, however if they are recovering then this may not be required. There may be financial barriers to review. At review check understanding and compliance and reinforce recommendations. The patient may not be recovering due to lack of understanding.
If the prescribed interventions are not effective at all or are not sufficiently effective then consider multimodal therapy. Multimodal therapy is a combination of exercises and manual therapy guided by a therapist.
There may be other barriers to recovery such as personal, social, or occupational barriers. There may be barriers that can be addressed for example by referral to a psychologist or occupational therapist - however there may be financial barriers.
The patient and practitioner should persist with the recommended interventions for two months. Patients will usually recover in this period if they are going to do so. The patient may be showing significant signs of recovery and so in that case it may be wise to persist with the interventions. At three months they are classified as having chronic pain, and so between the two to three month mark the practitioner should consider organising onward referral to allow timely assessment.
Prognosis
The true natural history is not completely known as many patients don't seek treatment. Also most studies enrol a mixture of both acute and chronic pain pain, further complicating matters. In general, most bouts of acute neck pain resolve within two months. However, many continue to have low grade symptoms or recurrence.[9] For example, in one general practice study, at one year 76% were fully recovered or much improved, but 47% continued to have ongoing neck pain.[10]
Of note, the natural history of neck pain following whiplash is more favourable than acute neck pain without whiplash. With whiplash, one study found 56% are recovered by 3 months, 70% by 6 months, 76% by 1 year, and 82% by 2 years. The proportion of patients with severe pain fell, and 5% had continued severe pain.[11] High initial pain intensity following whiplash is a poor prognostic indicator. Another weak factor is retaining a lawyer, however there is no evidence to support the concept of "litigation neurosis."[1]
Early treatment does not improve prognosis. There is also no association between degenerative changes and prognosis.
Risk factors for developing chronic pain are being female, older age, radiculopathy, higher baseline pain, widespread pain, smoking, obesity, poor general health, and various psychosocial factors.
Resources
Bibliography
- Bogduk, Nikolai, and Brian McGuirk. Management of acute and chronic neck pain : an evidence-based approach. Edinburgh New York: Elsevier, 2006.
- ↑ 1.0 1.1 Bogduk, Nikolai, and Brian McGuirk. Management of acute and chronic neck pain : an evidence-based approach. Edinburgh New York: Elsevier, 2006.
- ↑ Mahmoud et al.. The Relationship Between Forward Head Posture and Neck Pain: a Systematic Review and Meta-Analysis. Current reviews in musculoskeletal medicine 2019. 12:562-577. PMID: 31773477. DOI. Full Text.
- ↑ Jull et al.. The accuracy of manual diagnosis for cervical zygapophysial joint pain syndromes. The Medical journal of Australia 1988. 148:233-6. PMID: 3343953. DOI.
- ↑ Hoving et al.. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Annals of internal medicine 2002. 136:713-22. PMID: 12020139. DOI.
- ↑ Korthals-de Bos et al.. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ (Clinical research ed.) 2003. 326:911. PMID: 12714472. DOI. Full Text.
- ↑ Hoving et al.. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long-term results from a pragmatic randomized clinical trial. The Clinical journal of pain 2006. 22:370-7. PMID: 16691091. DOI.
- ↑ Driessen et al.. Cost-effectiveness of conservative treatments for neck pain: a systematic review on economic evaluations. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2012. 21:1441-50. PMID: 22447407. DOI. Full Text.
- ↑ Grooten et al.. The effect of ergonomic intervention on neck/shoulder and low back pain. Work (Reading, Mass.) 2007. 28:313-23. PMID: 17522452.
- ↑ Cohen & Hooten. Advances in the diagnosis and management of neck pain. BMJ (Clinical research ed.) 2017. 358:j3221. PMID: 28807894. DOI.
- ↑ Vos et al.. Clinical course and prognostic factors in acute neck pain: an inception cohort study in general practice. Pain medicine (Malden, Mass.) 2008. 9:572-80. PMID: 18565009. DOI.
- ↑ Radanov et al.. Long-term outcome after whiplash injury. A 2-year follow-up considering features of injury mechanism and somatic, radiologic, and psychosocial findings. Medicine 1995. 74:281-97. PMID: 7565068. DOI.