Bone Biomechanics: Difference between revisions
No edit summary |
No edit summary |
||
| Line 93: | Line 93: | ||
== Material Properties == | == Material Properties == | ||
{{See also|Material Properties}} | {{See also|Material Properties}} | ||
=== Cortical Bone === | |||
'''Elastic Behaviour''' | '''Elastic Behaviour''' | ||
| Line 151: | Line 153: | ||
** Viscoplastic: visco meaning creep behaviour, and plastic meaning permanent deformation after unloading | ** Viscoplastic: visco meaning creep behaviour, and plastic meaning permanent deformation after unloading | ||
** If cortical bone is longitudinally loaded above 70 MPa or 55% of ultimate strength, the rate of creep deformation increases sharply. | ** If cortical bone is longitudinally loaded above 70 MPa or 55% of ultimate strength, the rate of creep deformation increases sharply. | ||
* Mechanisms: | * Mechanisms: Tensile loading: osteon pullout; Longitudinal loading: fractures across osteons. | ||
'''Age Effects''' | '''Age Effects''' | ||
| Line 162: | Line 162: | ||
'''Microstructure and Mechanical Properties''' | '''Microstructure and Mechanical Properties''' | ||
* The change with age in mechanical properties differs with different bones | |||
* Determinants of mechanical properties are density (proportional to porosity), ash density (total mineral content divided by bulk volume), histology (number of osteons, primary versus secondary bone), collagen composition and content, collagen fibre and mineral orientation, cement line composition, bonding between mineral and collagen phases, and accumulation of microcracks in the bone matrix and around osteons. | |||
* Modulus and ultimate strength are correlated with apparent density using a power law. | |||
* Monotonic and fatigue strengths are related to the number of osteons | |||
* The most important determinant of modulus and strength is the ash density. | |||
* Wet bone is less stiff, less strong, and less brittle than fully dried bone. | |||
* After yielding, collagen content dominates stiffness. | |||
'''Fatigue Properties''' | |||
* Fatigue properties of bone: mechanical properties of bone under action of cyclic, repetitive loading. | |||
* In vivo cortical bone is exposed primarily to repetitive, low intensity loading than monotonic loading. | |||
* Cyclic loading can result in microstructural damage. | |||
* Stress fractures are a result of fatigue damage accumulation e.g. military recruits, long distance runners, race horses. | |||
* Fatigue fracture, like creep fracture, can occur at stress levels that are much lower than the monotonic strength. | |||
* One role of bone remodelling is repair of microcracks as a result of repetitive loading. | |||
* Fatigue behaviour of bone may be a factor in spontaneous age related fractures | |||
** With fatigue cracks, there may be a reduction in bone monotonic strength with age. | |||
** 10% of age related hip and over 50% of age related spine fractures are spontaneous (i.e. no obvious trauma) | |||
* Fatigue life reduces with increased body temperature. | |||
* Fatigue damage increases with increasing strain rate. | |||
* Fatigue life is less for uniaxial tension than uniaxial compression. | |||
* Mechanisms: Tension: osteon debonding; compression: oblique cracking. | |||
'''Mechanisms of Fatigue Damage Accumulation''' | |||
* Three stages of fatigue fracture: | |||
** Primary stage: crack initiation, with small decrease in stiffness and strength | |||
*** Haversian canals, lacunae, and canaliculi act as crack initiators. | |||
*** Bone remodels to reduce stress around these cracks. | |||
** Secondary stage: crack growth, slow further decrease in stiffness and strength | |||
*** cracks joint together | |||
*** Some osteons debond from matrix, contributing to osteon pullout | |||
*** Direction of crack propagation changes from perpendicular to loading to parallel to loading. | |||
*** These changes have an effect of stopping propagation of transverse cracks under longitudinal loading. | |||
*** Other weak effects stopping progression include interfaces between osteons and interstitial material, interfaces between adjacent lamellae in interstitial material, and interfaces within single osteon. | |||
** Tertiary stage: final fracture, rapid decrease in ability to support load | |||
*** cracks coalesce and become so large that weak interfaces no longer absorb them. Fails as final cracks travels across bone. | |||
* Modulus of bone decreases with crack formation. | |||
=== Trabecular Bone === | |||
* large variation in density for trabecular bone based on location and age | |||
* material properties of trabecular bone are very sensitive to apparent density | |||
* architecture: cortical bone is a low porosity solid. | |||
** Trabecular bone is an open-celled porous foam made up of a series of interconnecting trabeculae. | |||
** Idealised as a combination of rod-rod, rod-plate, or plat-plate cellular structures. (Rods are thin, and plates are thick trabeculae) | |||
'''Elastic Behaviour''' | |||
* Modulus of trabecular bone varies greater from 10 MPa to 2,000 MPa depending on location and age. | |||
* Less stiff than cortical bone (cortical bone modulus is 17,000 MPa) | |||
* Some regions less clear distinction (less research in these areas): cranium, subchondral proximal tibial plate, proximal femur metaphyseal shell, and vertebral body endplates. Mean modulus here ranges from 1,150 MPa to 9,650 MPa. | |||
'''Dependence of Apparent Density''' | |||
* Material properties of trabecular bone are very sensitive to apparent density | |||
* Power-law relationship of modulus with apparent density. | |||
* A 25% reduction in density in elderly cadaveric vertebrae, results in a 56% decrease in modulus | |||
'''Dependence on Architecture''' | |||
* Other than apparent density, architecture can also affect modulus | |||
* Architecture: shape and orientation of bone, general connectivity of trabeculae, mean thickness of trabeculae, mean spacing between trabeculae, and number of trabeculae. | |||
* Relationship varies depending on site for density and these variables. | |||
* Differences in architecture result in anisotropy of elastic properties. Nearly isotropic at some sites (proximal humerus), and highly anisotropic at others (elderly lumbar spine) | |||
'''Uniaxial Strength''' | |||
* In vivo failure is dominated by compressive loads | |||
* Both elastic and postyield behaviours are sensitive to apparent density. | |||
* Three regions of material behaviour in stress strain curve | |||
** First stage: material is in linear region, individual trabeculae bend and compress as the bulk is compressed | |||
** Second stage: failure occurs by fracture of some trabeculae and buckling of others. Lower density bone can deform more before final stiffening phase. | |||
** Third stage: as more trabeculae fail, strain increases until broken trabeculae begin to fill the pores. | |||
* Trabecular bone has a unique ability to absorb considerable energy for large compressive loads while maintaining a minimum mass. It can deform to compressive strains of over 50%. | |||
* | * | ||
[[Category:Anatomy]] | [[Category:Anatomy]] | ||
[[Category:Biomechanics]] | [[Category:Biomechanics]] | ||
Revision as of 11:30, 26 July 2021
Types of Bone
Bone consists of two forms: woven and lamella
| Property | Woven Bone | Lamellar Bone |
|---|---|---|
| Definition | "Primitive", immature | "Mature" bone, remodelled from woven bone |
| Found in | Embryo and new-born, in fracture callus, metaphyseal region of growing bone, tumours, osteogenesis imperfecta, and pagetic bone. | Throughout the mature skeleton in both trabecular and cortical bone. |
| Composition | Dense coarse-fibred collagen, varied mineral content, greater turnover, more cells per unit volume with random arrangement, no lamellae. | Formed by intramembranous or endochondral ossification, contains collagen fibres. |
| Organisation | Randomly arranged collagen fibres, disorganised | Highly ordered, stress-oriented collagen fibres |
| Mechanical Properties | Isotropic | Anisotropic |
| Strength | Weaker, more flexible, more easily deformed | More stiffness and strength |
Woven and lamellar bone are organised structurally into trabecular (spongy or cancellous) bone and cortical (dense or compact) bone.
| Trabecular Bone | Cortical Bone | |
|---|---|---|
| Mass | Cortical bone has four times the mass of trabecular bone | |
| Metabolic turnover | Trabecular bone has 8 times greater metabolic turnover due to its high surface area as bone turnover happens at the surface. | |
| Found in | Metaphysis and epiphysis of long bones and in cuboid bones such as the vertebrae | Diaphysis of long bones, and envelope of cuboid bones. |
| Structure | Internal beams/spicules form a 3D branching lattice aligned along areas of mechanical stress. | Compact bone is formed by layers of lamellar bone.
Plexiform bone in larger animals is formed by layers of lamellar and woven bone. Haversian bone is composed of vascular channels circumferentially surrounded by lamellar bone, with a unit being an osteon. |
| Subjected forces | Compression predominates, but is subjected to complex set of stresses and strains | Bending, torsional, and compressive forces. |
| Density | Proximal tibial trabecular bone: 0.30 g/cm³
Greater percentage deviation in density compared to cortical bone. |
Femoral cortical bone: 1.85g/cm³ |
| Porosity | Typically 50% to 90% | Typically 10%. Densities of trabecular and cortical bone can overlap, cortical bone is usually defined as bone with less than approximately 30% porosity. |
| Architecture | Network of small, interconnected plates and rods of individual trabeculae with relatively large spaces between the trabeculae. Individual trabeculae contains only some of the voids found in cortical bone (canaliculi, lacunae, and rarely Haversian canals) | Solid containing a series of dense voids: Haversian and Volkmann's canals and to a lesser extent lacunae and canaliculi. |
Osteons in Haversian Bone
- Osteon: the major structural unit of cortical bone, is an irregular, branching, and anastomosing cylinder composed of a more or less centrally placed neurovascular canal surrounded by cell-permeated layers of bone matrix.
- Osteons are generally oriented in the long axis of the bone
- Haversian canal: The central canal of an osteon. This contains cells, vessels, and occasionally nerves
- Volkmann's canal: the canals connecting osteons
- Vessels: capillaries but smaller vessels resemble lymphatic vessels. Derived from th4e principal nutrient arteries of the bone or epiphyseal and metaphyseal arteries. A vascular network is formed.
Biomechanics of Bone
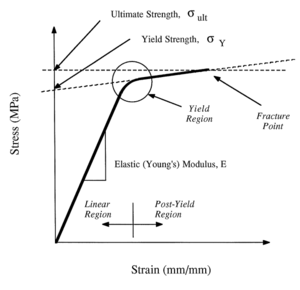
- The stress-strain curve has three regions: initial linear region, yield region, and postyield region
- Young's modulus is the slope of the linear region
- The strength properties are obtained from the yield and postyield regions
- Yielding (onset of permanent deformation) occurs at the junction of the linear and postyield regions
- Fracture occurs when the ultimate strength is reached.
Material Properties
- See also: Material Properties
Cortical Bone
Elastic Behaviour
- Isotropic materials: elastic properties do not depend on the orientation of the material with respect to the loading direction. Characterised by Young's modulus. Poisson's ratio measures how much a material bulges with compression or contracts with stretching.
- Anisotropic materials: elastic properties depend on their orientation with respect to the loading direction. Includes bone in the longitudinal direction. Cortical bone is transversely isotropic, i.e. it is isotropic with loading in the transverse plane. Transverse isotropy is a subset of anisotropy.
- Young's modulus of bone: modulus of cortical bone in longitudinal direction is 1.5 times the modulus in the transverse direction, and over 5 times the modulus in the shear direction.
- Poisson's ratio of bone: relatively high indicating that cortical bone bulges more than metals when subjected to uniaxial compression.
Strength
- The strength properties of bone also depends on
- The loading direction. Bone is transversely isotropic from both modulus and strength perspectives
- The method of loading: tension, compression, or torsion.
- Due to the above complexity it isn't possible to specify the strength of cortical bone with a single value.
- Cortical bone longitudinal strength: stronger in longitudinal compression (190 MPa) than tension (130 MPa)
- Cortical bone transverse strength: stronger in compression (130 MPa) than tension (50 MPa)
- Consistent with everyday loads where maximum compressive stresses are larger than maximum tensile stresses
- When cortical bone is loaded close to its yield point it is close to fracture as its yield strength is close to its ultimate strength. Before fracture cortical bone undergoes relatively large deformations.
Energy Absorption, Ductility, and Brittleness
- Toughness: a tough material is a material that absorbs substantial energy before failure.
- Fracture occurs if energy delivered is greater than the capacity of the bone to absorb energy
- Longitudinal loading
- Bone is tough in longitudinal loading
- Bone is relatively ductile in longitudinal loading, i.e. it undergoes a large amount of deformation prior to fracture.
- Transverse loading
- Bone is tougher under compressive than tensile loads. The ultimate strains are much larger than the yield strains.
- Ultimate strain is close to the yield strain for tensile loading in the transverse direction, i.e. it is relatively brittle for transverse loading.
- Therefore cortical bone can be relatively ductile or brittle depending on the loading direction and on whether tensile or compressive forces are applied
Viscoelastic Behaviour
- Cortical bone is viscoelastic because the mechanical properties are sensitive to both strain rate and duration of applied load.
Strain Rate Sensitivity
- Strain rates increase by orders of magnitude from slow walking, to brisk walking, to slow running.
- With increasing strain rates
- Modulus: Young's modulus increases
- Strength: Yield and ultimate strength of cortical bone increases
- Same increase strain rates results in relatively larger change in strength than modulus.
- At very high strain rates (high-impact trauma), cortical bone because more brittle (ultimate strain decreases) for loading in longitudinal direction.
- But in normal activity, increase in strain rates results in increase in ductility (ultimate strain increases). Optimal range of strain rate is 0.01 to 0.1 per second.
Creep Behaviour
- Creep: When bone is subjected to a constant stress over an extended period of time it will continue to deform.
- Three stages of creep:
- Primary stage: strain continues after loading and creep gradually decreases
- Secondary stage: lower usually constant creep
- Tertiary stage: marked increase in creep just before creep fracture
- Creep fracture:
- Stress level well below yield and ultimate strengths.
- Time required until creep fracture reduces with increasing strength
- Resistance to creep fracture is greater for compressive than tensile loading
- Permanent deformation:
- Prolonged loading then unloaded before creep fracture
- Viscoplastic: visco meaning creep behaviour, and plastic meaning permanent deformation after unloading
- If cortical bone is longitudinally loaded above 70 MPa or 55% of ultimate strength, the rate of creep deformation increases sharply.
- Mechanisms: Tensile loading: osteon pullout; Longitudinal loading: fractures across osteons.
Age Effects
- Modulus and strength properties deteriorates with aging, e.g. reduction of 2% per decade after 20 years of femoral middiaphysis.
- Reduction of energy absorption with aging by 7% per decade mainly due to reduced ultimate strain
- With aging cortical bone is less stiff, less strong, and more brittle
Microstructure and Mechanical Properties
- The change with age in mechanical properties differs with different bones
- Determinants of mechanical properties are density (proportional to porosity), ash density (total mineral content divided by bulk volume), histology (number of osteons, primary versus secondary bone), collagen composition and content, collagen fibre and mineral orientation, cement line composition, bonding between mineral and collagen phases, and accumulation of microcracks in the bone matrix and around osteons.
- Modulus and ultimate strength are correlated with apparent density using a power law.
- Monotonic and fatigue strengths are related to the number of osteons
- The most important determinant of modulus and strength is the ash density.
- Wet bone is less stiff, less strong, and less brittle than fully dried bone.
- After yielding, collagen content dominates stiffness.
Fatigue Properties
- Fatigue properties of bone: mechanical properties of bone under action of cyclic, repetitive loading.
- In vivo cortical bone is exposed primarily to repetitive, low intensity loading than monotonic loading.
- Cyclic loading can result in microstructural damage.
- Stress fractures are a result of fatigue damage accumulation e.g. military recruits, long distance runners, race horses.
- Fatigue fracture, like creep fracture, can occur at stress levels that are much lower than the monotonic strength.
- One role of bone remodelling is repair of microcracks as a result of repetitive loading.
- Fatigue behaviour of bone may be a factor in spontaneous age related fractures
- With fatigue cracks, there may be a reduction in bone monotonic strength with age.
- 10% of age related hip and over 50% of age related spine fractures are spontaneous (i.e. no obvious trauma)
- Fatigue life reduces with increased body temperature.
- Fatigue damage increases with increasing strain rate.
- Fatigue life is less for uniaxial tension than uniaxial compression.
- Mechanisms: Tension: osteon debonding; compression: oblique cracking.
Mechanisms of Fatigue Damage Accumulation
- Three stages of fatigue fracture:
- Primary stage: crack initiation, with small decrease in stiffness and strength
- Haversian canals, lacunae, and canaliculi act as crack initiators.
- Bone remodels to reduce stress around these cracks.
- Secondary stage: crack growth, slow further decrease in stiffness and strength
- cracks joint together
- Some osteons debond from matrix, contributing to osteon pullout
- Direction of crack propagation changes from perpendicular to loading to parallel to loading.
- These changes have an effect of stopping propagation of transverse cracks under longitudinal loading.
- Other weak effects stopping progression include interfaces between osteons and interstitial material, interfaces between adjacent lamellae in interstitial material, and interfaces within single osteon.
- Tertiary stage: final fracture, rapid decrease in ability to support load
- cracks coalesce and become so large that weak interfaces no longer absorb them. Fails as final cracks travels across bone.
- Primary stage: crack initiation, with small decrease in stiffness and strength
- Modulus of bone decreases with crack formation.
Trabecular Bone
- large variation in density for trabecular bone based on location and age
- material properties of trabecular bone are very sensitive to apparent density
- architecture: cortical bone is a low porosity solid.
- Trabecular bone is an open-celled porous foam made up of a series of interconnecting trabeculae.
- Idealised as a combination of rod-rod, rod-plate, or plat-plate cellular structures. (Rods are thin, and plates are thick trabeculae)
Elastic Behaviour
- Modulus of trabecular bone varies greater from 10 MPa to 2,000 MPa depending on location and age.
- Less stiff than cortical bone (cortical bone modulus is 17,000 MPa)
- Some regions less clear distinction (less research in these areas): cranium, subchondral proximal tibial plate, proximal femur metaphyseal shell, and vertebral body endplates. Mean modulus here ranges from 1,150 MPa to 9,650 MPa.
Dependence of Apparent Density
- Material properties of trabecular bone are very sensitive to apparent density
- Power-law relationship of modulus with apparent density.
- A 25% reduction in density in elderly cadaveric vertebrae, results in a 56% decrease in modulus
Dependence on Architecture
- Other than apparent density, architecture can also affect modulus
- Architecture: shape and orientation of bone, general connectivity of trabeculae, mean thickness of trabeculae, mean spacing between trabeculae, and number of trabeculae.
- Relationship varies depending on site for density and these variables.
- Differences in architecture result in anisotropy of elastic properties. Nearly isotropic at some sites (proximal humerus), and highly anisotropic at others (elderly lumbar spine)
Uniaxial Strength
- In vivo failure is dominated by compressive loads
- Both elastic and postyield behaviours are sensitive to apparent density.
- Three regions of material behaviour in stress strain curve
- First stage: material is in linear region, individual trabeculae bend and compress as the bulk is compressed
- Second stage: failure occurs by fracture of some trabeculae and buckling of others. Lower density bone can deform more before final stiffening phase.
- Third stage: as more trabeculae fail, strain increases until broken trabeculae begin to fill the pores.
- Trabecular bone has a unique ability to absorb considerable energy for large compressive loads while maintaining a minimum mass. It can deform to compressive strains of over 50%.