Bone Biomechanics
Biomechanics of Bone
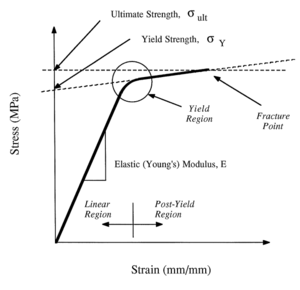
- The stress-strain curve has three regions: initial linear region, yield region, and postyield region
- Young's modulus is the slope of the linear region
- The strength properties are obtained from the yield and postyield regions
- Yielding (onset of permanent deformation) occurs at the junction of the linear and postyield regions
- Fracture occurs when the ultimate strength is reached.
Material Properties
- See also: Material Properties
Cortical Bone
Elastic Behaviour
- Isotropic materials: elastic properties do not depend on the orientation of the material with respect to the loading direction. Characterised by Young's modulus. Poisson's ratio measures how much a material bulges with compression or contracts with stretching.
- Anisotropic materials: elastic properties depend on their orientation with respect to the loading direction. Includes bone in the longitudinal direction. Cortical bone is transversely isotropic, i.e. it is isotropic with loading in the transverse plane. Transverse isotropy is a subset of anisotropy.
- Young's modulus of bone: modulus of cortical bone in longitudinal direction is 1.5 times the modulus in the transverse direction, and over 5 times the modulus in the shear direction.
- Poisson's ratio of bone: relatively high indicating that cortical bone bulges more than metals when subjected to uniaxial compression.
Strength
- The strength properties of bone also depends on
- The loading direction. Bone is transversely isotropic from both modulus and strength perspectives
- The method of loading: tension, compression, or torsion.
- Due to the above complexity it isn't possible to specify the strength of cortical bone with a single value.
- Cortical bone longitudinal strength: stronger in longitudinal compression (190 MPa) than tension (130 MPa)
- Cortical bone transverse strength: stronger in compression (130 MPa) than tension (50 MPa)
- Consistent with everyday loads where maximum compressive stresses are larger than maximum tensile stresses
- When cortical bone is loaded close to its yield point it is close to fracture as its yield strength is close to its ultimate strength. Before fracture cortical bone undergoes relatively large deformations.
Energy Absorption, Ductility, and Brittleness
- Toughness: a tough material is a material that absorbs substantial energy before failure.
- Fracture occurs if energy delivered is greater than the capacity of the bone to absorb energy
- Longitudinal loading
- Bone is tough in longitudinal loading
- Bone is relatively ductile in longitudinal loading, i.e. it undergoes a large amount of deformation prior to fracture.
- Transverse loading
- Bone is tougher under compressive than tensile loads. The ultimate strains are much larger than the yield strains.
- Ultimate strain is close to the yield strain for tensile loading in the transverse direction, i.e. it is relatively brittle for transverse loading.
- Therefore cortical bone can be relatively ductile or brittle depending on the loading direction and on whether tensile or compressive forces are applied
Viscoelastic Behaviour
- Cortical bone is viscoelastic because the mechanical properties are sensitive to both strain rate and duration of applied load.
Strain Rate Sensitivity
- Strain rates increase by orders of magnitude from slow walking, to brisk walking, to slow running.
- With increasing strain rates
- Modulus: Young's modulus increases
- Strength: Yield and ultimate strength of cortical bone increases
- Same increase strain rates results in relatively larger change in strength than modulus.
- At very high strain rates (high-impact trauma), cortical bone becomes more brittle (ultimate strain decreases) for loading in longitudinal direction.
- But in normal activity, increase in strain rates results in increase in ductility (ultimate strain increases). Optimal range of strain rate is 0.01 to 0.1 per second.
Creep Behaviour
- Creep: When bone is subjected to a constant stress over an extended period of time it will continue to deform.
- Three stages of creep:
- Primary stage: strain continues after loading and creep gradually decreases
- Secondary stage: lower usually constant creep
- Tertiary stage: marked increase in creep just before creep fracture
- Creep fracture:
- Stress level well below yield and ultimate strengths.
- Time required until creep fracture reduces with increasing strength
- Resistance to creep fracture is greater for compressive than tensile loading
- Permanent deformation:
- Prolonged loading then unloaded before creep fracture
- Viscoplastic: visco meaning creep behaviour, and plastic meaning permanent deformation after unloading
- If cortical bone is longitudinally loaded above 70 MPa or 55% of ultimate strength, the rate of creep deformation increases sharply.
- Mechanisms: Tensile loading: osteon pullout; Longitudinal loading: fractures across osteons.
Age Effects
- Modulus and strength properties deteriorates with aging, e.g. reduction of 2% per decade after 20 years of femoral middiaphysis.
- Reduction of energy absorption with aging by 7% per decade mainly due to reduced ultimate strain
- With aging cortical bone is less stiff, less strong, and more brittle
Microstructure and Mechanical Properties
- The change with age in mechanical properties differs with different bones
- Determinants of mechanical properties are
- Density (proportional to porosity)
- Ash density (total mineral content divided by bulk volume)
- Histology (number of osteons, primary versus secondary bone)
- Collagen composition and content
- Collagen fibre and mineral orientation
- Cement line composition
- Bonding between mineral and collagen phases
- Accumulation of microcracks in the bone matrix and around osteons.
- Modulus and ultimate strength are correlated with apparent density using a power law.
- Monotonic and fatigue strengths are related to the number of osteons
- The most important determinant of modulus and strength is the ash density.
- Wet bone is less stiff, less strong, and less brittle than fully dried bone.
- After yielding, collagen content dominates stiffness.
Fatigue Properties
- Fatigue properties of bone: mechanical properties of bone under action of cyclic, repetitive loading.
- In vivo cortical bone is exposed primarily to repetitive, low intensity loading than monotonic loading.
- Cyclic loading can result in microstructural damage.
- Stress fractures are a result of fatigue damage accumulation e.g. military recruits, long distance runners, race horses.
- Fatigue fracture, like creep fracture, can occur at stress levels that are much lower than the monotonic strength.
- One role of bone remodelling is repair of microcracks as a result of repetitive loading.
- Fatigue behaviour of bone may be a factor in spontaneous age related fractures
- With fatigue cracks, there may be a reduction in bone monotonic strength with age.
- 10% of age related hip and over 50% of age related spine fractures are spontaneous (i.e. no obvious trauma)
- Fatigue life reduces with increased body temperature.
- Fatigue damage increases with increasing strain rate.
- Fatigue life is less for uniaxial tension than uniaxial compression.
- Mechanisms: Tension: osteon debonding; compression: oblique cracking.
Mechanisms of Fatigue Damage Accumulation
- Three stages of fatigue fracture:
- Primary stage: crack initiation, with small decrease in stiffness and strength
- Haversian canals, lacunae, and canaliculi act as crack initiators.
- Bone remodels to reduce stress around these cracks.
- Secondary stage: crack growth, slow further decrease in stiffness and strength
- cracks joint together
- Some osteons debond from matrix, contributing to osteon pullout
- Direction of crack propagation changes from perpendicular to loading to parallel to loading.
- These changes have an effect of stopping propagation of transverse cracks under longitudinal loading.
- Other weak effects stopping progression include interfaces between osteons and interstitial material, interfaces between adjacent lamellae in interstitial material, and interfaces within single osteon.
- Tertiary stage: final fracture, rapid decrease in ability to support load
- cracks coalesce and become so large that weak interfaces no longer absorb them. Fails as final cracks travels across bone.
- Primary stage: crack initiation, with small decrease in stiffness and strength
- Modulus of bone decreases with crack formation.
Trabecular Bone
- large variation in density for trabecular bone based on location and age
- material properties of trabecular bone are very sensitive to apparent density
- architecture: cortical bone is a low porosity solid.
- Trabecular bone is an open-celled porous foam made up of a series of interconnecting trabeculae.
- Idealised as a combination of rod-rod, rod-plate, or plat-plate cellular structures. (Rods are thin, and plates are thick trabeculae)
Elastic Behaviour
- Modulus of trabecular bone varies greater from 10 MPa to 2,000 MPa depending on location and age.
- Less stiff than cortical bone (cortical bone modulus is 17,000 MPa)
- Some regions less clear distinction (less research in these areas): cranium, subchondral proximal tibial plate, proximal femur metaphyseal shell, and vertebral body endplates. Mean modulus here ranges from 1,150 MPa to 9,650 MPa.
Dependence of Apparent Density
- Material properties of trabecular bone are very sensitive to apparent density
- Power-law relationship of modulus with apparent density.
- A 25% reduction in density in elderly cadaveric vertebrae, results in a 56% decrease in modulus
Dependence on Architecture
- Other than apparent density, architecture can also affect modulus
- Architecture: shape and orientation of bone, general connectivity of trabeculae, mean thickness of trabeculae, mean spacing between trabeculae, and number of trabeculae.
- Relationship varies depending on site for density and these variables.
- Differences in architecture result in anisotropy of elastic properties. Nearly isotropic at some sites (proximal humerus), and highly anisotropic at others (elderly lumbar spine)
Uniaxial Strength
- In vivo failure is dominated by compressive loads
- Both elastic and postyield behaviours are sensitive to apparent density.
- Three regions of material behaviour in stress strain curve for compression
- First stage: material is in linear region, individual trabeculae bend and compress as the bulk is compressed
- Second stage: failure occurs by fracture of some trabeculae and buckling of others. Lower density bone can deform more before final stiffening phase.
- Third stage: as more trabeculae fail, strain increases until broken trabeculae begin to fill the pores.
- Trabecular bone has a unique ability to absorb considerable energy for large compressive loads while maintaining a minimum mass. It can deform to compressive strains of over 50%.
- Compressive strength of trabecular bone also related to apparent density by a power-law relationship.
- Main parameter that controls failure in trabecular bone is maximum level of strain rather than stress.
- Subtle changes in bone apparent density results in large changes in strength and modulus.
- Tensile behaviour is different to its compressive behaviour
- Linear behaviour is similar to compressive loading
- Postyield behaviour : as more trabeculae fracture the specimen can take progressively less load until complete fracture occurs.
- Postyield load carrying capacity of trabecular bone
- high for compression and almost negligible for tension.
- Trabecular bone loaded beyond ultimate strength in compression can still carry substantial load. Local failure in compression isn't likely to lead to failure of the whole bone.
- loaded beyond ultimate strength in tension no load can be carried because it fractures. The surrounding tissue must carry the load and a cascade occurs propagating across the whole one causing fracture.
Age Effects
- Spine, distal radius, and proximal femur are largely trabecular bone structures, and fractures here occur commonly.
- Age related trabecular bone fragility associated with increased incidence of hip, spine, and radial fractures.
- Absolute bone density isn't a good predictor, however decreases in bone density and resulting increase in bone fragility are good predictors of spine fracture.
- Bone mineral density reflects areal density of both trabecular and cortical bone, decreases with age.
- Senile osteoporosis results in equal reductions in cortical and trabecular bone mass.
- Postmenopausal osteoporosis is characterised by excessive and disproportionate trabecular bone loss.
- With decreasing density, there is decreasing number and thickness of trabeculae, and increase in intertrabecular spaces.
- Preferential loss of of vertical trabeculae with increasing age: Number of horizontal trabeculae less than vertical trabeculae in lumbar spine, regardless of density. With decreasing density, loss of vertical trabeculae occurs at twice the rate of loss of horizontal trabeculae.
- Complete loss of a single trabeculum is irreversible because bone can only be formed on existing surfaces.
- Strength of trabecular bone depends on both apparent density and architecture, age related changes substantially weaken it. Failure mechanisms are
- Failure by buckling occurs through triple jeopardy through reduction in number, decrease in thickness, and increase in length of individual trabeculae.
- Failure by fracture occurs through double jeopardy through reduction in number and thickness of trabeculae.
- Accompanying reduction in strength through above mechanisms may be greater than reductions in density alone.
Structural Properties
- Bones of appendicular skeleton are long, slender, and slightly curved.
- Long bones are subjected to a combination of compressive forces, bending moments, and torsion.
- Long bones are loaded primarily in
- Compression through contact forces applied at the joint surfaces
- Tension through muscle forces applied about the joint surfaces.
- Contact forces larger than muscle forces generally.
- Combined compressive and tensile forces results in net bending moment on the diaphysis. Bending can occur even without muscle forces because of bone curvature. Torsion can also occur due to torque about the longitudinal axis.
Bending of Bone
- Cross-sectional area is most important parameter for axial loading
- Moment of inertia is most important parameter for bending.
- Moment of inertia: how the material is distributed with respect to a specified reference axis (neutral axis).
- A region of material that is at a greater distance from neutral axis is more efficient in resisting bending about that axis than a region of material coincident with it.
- Long bones are hollow, most bone tissue is located away from the neutral axis. The hollow nature resists primarily bending loads in both frontal and sagittal planes, and torsional loads about the diaphyseal axis.
Combined Axial and Bending Loads on Bone
- Bending in frontal plane causes tensile stresses along lateral aspect and compressive forces along medial aspect.
- Bending in sagittal plane (posteriorly directed loads) also results in tensile stresses in the anterior aspect, and compressive stresses in the posterior aspect.
- In general compressive stresses are higher than tensile stresses for the appendicular skeleton, and the compressive strength of cortical bone is greater than its tensile strength.
Age-Related Remodelling of the Diaphysis
- Axial stresses are not very sensitive to age-related geometric changes
- Bending stresses are very sensitive to these changes.
- There is an age-related endosteal and periosteal expansion of the diaphysis
- This expansion can reduce bending stresses by over 25% compared to younger bones.
- This age-related geometric remodelling processes helps to compensate for age-related reductions in strength.
- Age-related compensatory geometric remodelling however doesn't occur in the proximal femur and spine. This explains why there isn't an exponential increase in diaphyseal fracture in the elderly, compared to proximal femur and spine fracture.
Combined Axial, Bending, and Torsional Loads
- Principal stress acts in the principal direction.
- Stresses from axial loading and bending: Without torsion the principal stress is the sum of the axial and bending stress.
- Superimposed shear stresses: axial, bending, and shear stresses are combined in a more complex manner. Adding a torsional load on combined axial and bending loads increases the principal stress and changes the principal direction.
In Vivo Fracture Prediction
Fracture Risk
- Three important pieces of information for failure-resistant design
- Geometry of the structure
- Mechanical properties of the materials from which the structure is made
- Location and direction of loads to which the structure is subjected
- Safety factor: ratio of material strength to the imposed stress at each point, or ratio of force required to cause failure of the entire structure to the imposed force.
- Risk factor: inverse of safety factor, i.e. imposed load divided by the load that would cause failure. A risk factor much less than one is low risk of failure, a risk factor close to or greater than 1 is high risk of failure.
- To decrease the risk factor engineers can increase the size of the structure, use a stronger material, or reduce the imposed loads
- Most engineering structures have risk factors of 0.15 to 0.2
- Applying to human skeleton is complicated due to uncertainty about magnitudes and directions of imposed loads, forces generated due to traumatic events, and age-related changes.
Quantitative CT (QCT) and Material Properties of Trabecular and Cortical Bone
- Trabecular bone: Strong correlations between QCT density and modulus and compressive strength. QCT can estimate modulus and strength of trabecular bone tissue
- Cortical bone: poor correlations between QCT data and modulus and strength of cortical bone. Possibly due QCT inability to differentiate between very narrow range of cortical bone densities.
QCT and Vertebral Body Failure
- Strong correlations between fracture load and measured density of trabecular bone in vertebral body, but only moderate correlations between fracture load and QCT density.
- Fracture load for uniaxial compression of isolated intact elderly vertebrae: 3,100 to 3,400N
- Loads during activities: 440-770N for relaxed standing, 1110N for coughing, 1800N for sit-ups, 1850N for forward flexion of 20 degrees while lifting a 20kg mass, 3400N for lifting 20kg with bent back and straight knees, 5400N for lifting a 50kg mass with straight knees, 18800 to 36400N for power lifting in highly trained athletes.
Fracture Risk Factors for the Spine
- Intra-abdominal press reduces spinal compressive forces only by about 15%
- Facet joints carry only between 3-25% of lumbar spine loads.
- Additive contributions of 40%, theoretically can reduce above numbers by 40%.
- Risk factor is therefore 0.33 for forward flexion with 20kg in each hand, and about 1 for lifting 50kg with knees straight. I.e. not surprising that compression fractures are so common.
QCT and Proximal Femur Failure
- Fracture forces in vitro
- Single-leg stance: 2,000 to 8,500 N
- Simulated fall: 800 to 4,000 N
- Simulated normal gait: 1,000 to 12,750 N (i.e. higher than for a fall)
- More than 90% of hip fractures are associated with trauma from a fall usually from standing height or lower. There is reduced tissue strength for transverse loading.
- Intertrochanteric region: very significant positive correlation between mean intertrochanteric trabecular QCT value and whole bone strength. Even stronger correlation with QCT value multiplied by total intertrochanteric cross-sectional area.
Fracture Risk Factors for the Hip
- In vivo estimated forces with risk factors for failure loads of 1,000 -12,750 N
- Single-leg stance: 1.8 to 6 times BW, risk factor 0.13 to 1.6.
- Normal gait: 3 to 8 times BW
- Stair ascent: 7 to 8 times BW, risk factor 0.25 to 3.2
- Rising from a chair: 3 times BW
- A fall results in substantial trauma to the skeleton. Epidemiologic studies show order of magnitude greater energy than in vitro experiments.
- Other factors influences force delivery:
- soft tissue energy absorption over greater trochanter, muscle contraction state (increased impact forces with muscle-active state), position of trunk and extremities on impact., soft tissue thickness (reduced force)
- In elderly, any fall with direct impact to the greater trochanter has a high probability of hip fracture., regardless of these factors, or even the fragility of the bone within the proximal femur.
In Vivo Fracture Risk Prediction
- There is substantial overlap in QCT mineral densities between individuals with atraumatic vertebral fractures and controls.
- Loading conditions are important in fracture aetiology. Simple densitometric comparisons to fracture thresholds don't account for this.
- For atraumatic fracture data on activity is important.
- For falls in elderly factors relating to the mechanics of the fall dominate the fracture aetiology, while densitometric measures have less significance.
See Also
References
- Study notes from Orthopaedic Basic Science, Chapter 13 Form and Function of Bone