Bradykinin
Bradykinin is a potent inflammatory peptide messenger, and as a kinin is part of the kallikrein-kinin system which has wide ranging effects on the body.
Roles in the Body
Bradykinin is released from damaged tissue following injury or with inflammation. Mast cells also release bradykinin.
- Nociceptive system: Bradykinin both activates and sensitises sensory neurons. it is a very potent pain-producing substance. Following the release with injury or inflammation, it excites a high percentage or nociceptors and sensitises them to other noxious stimuli. The sensitisation occurs through activation of B1 and B2 receptors.
- Rheumatological system: The des-Arg kinin derivates induce collagen synthesis, fibroblast proliferation, and cytokine release from macrophages.
- Vascular system: bradykinin acts as a vasodilator (through local production of NO and prostaglandins), increases vessel permeability, and stimulates the formation of prostacyclin. It has a role in the pathophysiology of C1 esterase inhibitor deficiency.
- Renal system: It increases renal flow through vasodilation and inhibits inhibits sodium reabsorption leading to natriuresis. This leads to reduced blood pressure.
- Respiratory system: It has bronchoconstrictor effects and plays a role in asthma and rhinitis.
- Gastrointestinal system: causes smooth muscle contraction, and is involved in visceral nociception.
Kallikrein-Kinin System
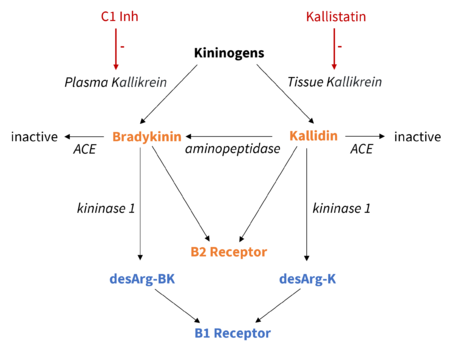
Kinins are the active peptides of the kallikrein-kinin system . Kinins are released either by tissue or the plasma. These are two distinct proteolytic pathways and are initiated by the activation of serine proteases called plasma kallikrein and tissue kallikrein. Plasma kallikrein and Tissue kallikrein differ in their tissue location, substrate specificity, and each have specific inhibitory factors.[1]
- Tissue kallikrein-kinin system: Tissue kallikrein acts to form kallidin from kininogens, which are inactive precursors. Tissue kallikrein is inhibited by kallikrein-binding protein or kallistatin.
- Plasma kallikrein-kinin system: Plasma kallikrein is released from prekallikrein by activated factor XII. Prekallikrein reciprocally activates FXII. Plasma kallikrein forms bradykinin from the kininogens. Plasma kallikrein is inhibited by compliment 1 inhibitor protein.
Bradykinin and Kallidin (also known as Lys-bradykinin) are vasoactive, and cause the classical signs of inflammation. Kallidin is similar to bradykinin in its effects, and can be converted to bradykinin by aminopeptidase. They mediate their effects through kinin receptor B2.
The half lives of bradykinin and kallidin are seconds, as they are rapidly hydrolysed by kininase 1 to other biologically active des-Arg kinin derivatives. The des-Arg derviatives are involved in fibrous tissue synthesis. They mediate their effects through kinin receptor B1.
Kininase 2 (Angiotensin converting enzyme ) inactivates bradykinin in the lungs and kidneys. Neuro endopeptidase is also involved in kinin degradation.
Bradykinin Receptors
The B1 and B2 receptors are coupled to G proteins. In doing so they are involved in second messenger signalling at the site of nerve endings. B2 is expressed constitutively (constitutive means a gene is expressed in an ongoing manner) while B1 is expressed with trauma and inflammation.
B2 Receptor - constitutive
In the normal state with intact tissue, bradykinin and kallidin bind to the B2 receptor. B2 is expressed constitutively, including both the central and peripheral nervous system. B2 has a role in acute inflammatory events.
When bradykinin activates B2, there is direct stimulation of nociceptors (C & Aδ fibres). Kinins cause sensitisation of sensory fibres to thermal, chemical, and mechanical stimuli.
There is a cascade of intracellular reactions through the protein kinase C (PKC) pathway that results in an increase in sodium conductance causing membrane depolarisation and influx of calcium through voltage gated calcium channels.
B1 Receptor - inducible
B1 expression is inducible. With chronic inflammation (compare to B2 with acute inflammation) and certain forms of persistent hyperalgesia, B1 is synthesised by the nociceptor cell body. B1 is then transported to the nerve ending membrane. B1 production is an important aspect of neural sensitisation and tissue repair through the des-Arg derivatives.
Note how the tanoxomy is the opposite to COX, with COX-1 being the "constitutive enzyme" and COX-2 being the "inducible one"
Broader Picture
There is a synergy between bradykinin and other inflammatory mediators.
There are many downstream effects with the activation of the bradykinin system. For example it leads to the production of 12-lipoxygenase metabolites from arachidonic acid, and this activates the TRPV1 receptor.[2] TRPV1 is involved in mechanical, thermal, and chemical sensitivity. TRPA1 is also activated which is a mechanosensitive and thermosensitive channel.
Bradykinins, prostaglandins, and histamine are all mediators of vasodilation. Vasodilation being a process involved in clinical signs of inflammation - redness (rubor) and warmth (calor).
Bradykinin, prostaglandin E2, and histamine also all sensitise sensory nerve endings. This leads to the pain (dolor) aspect of inflammation.
Bradykinin acts directs on sensory neurons, and via a separate 12-lipoxygenase pathway, stimulates TRPV1.
References
- ↑ Webb JG. The kallikrein/kinin system in ocular function. J Ocul Pharmacol Ther. 2011 Dec;27(6):539-43. doi: 10.1089/jop.2011.0187. Epub 2011 Dec 2. PMID: 22136090.
- ↑ Shin J, Cho H, Hwang SW, Jung J, Shin CY, Lee SY, Kim SH, Lee MG, Choi YH, Kim J, Haber NA, Reichling DB, Khasar S, Levine JD, Oh U. Bradykinin-12-lipoxygenase-VR1 signaling pathway for inflammatory hyperalgesia. Proc Natl Acad Sci U S A. 2002 Jul 23;99(15):10150-5. doi: 10.1073/pnas.152002699. Epub 2002 Jul 3. PMID: 12097645; PMCID: PMC126639.