Carpal Tunnel Syndrome
Carpal Tunnel Syndrome (CTS) is a common clinical condition that causes pain, numbness, and tingling in the hand. CTS occurs when the median nerve is squeezed or compressed as it travels through the carpal tunnel. It was first described by Paget 1913. Studies by Phalen in the 1950 established the principles of CTS
Epidemiology
It is the most common condition among patients complaining of hand and finger symptoms. It is the most common entrapment neuropathy (90%). It occurs in 4-6% of the general population. The peak age range is 40-60 with 75% of affected patients being female.
Anatomy
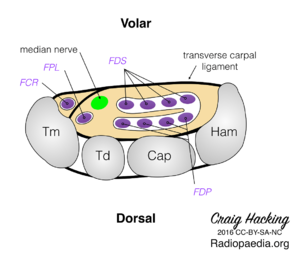
The carpal tunnel is a non-extendible osteofibrous tunnel surrounded by the following structures
- Roof: flexor retinaculum. The transverse carpal ligament is the thick (2-4mm) central segment of the flexor retinaculum formed by strong interwoven bundles of fibrous connective tissue. It is short and broad (average width is 25mm and average length is 31mm). It extends from the distal part of the radius to the distal segment of the base of the third metacarpal. The mean proximal limit of its central portion is 11 mm distal to the capitate-lunate joint and the mean distal limit of its distal portion is 10 mm distal to the carpometacarpal joint of the third metacarpal.
- Base: carpal sulcus. The base is formed by the capsule and the anterior radiocarpal ligaments cover the underlying portions of the scaphoid, lunate, capitate, hamate, trapezium, and trapezoid.
- Ulnar edge: hamate hook, pyramidal bone and pisiform bone
- Radial edge: scaphoid bone, trapezoid bone and tendon of the flexor carpi radialis (FCR) muscle.
The tunnel gives passage to:
- Eight digital flexor tendons (two for each of the medial four fingers)
- Flexor pollicis longus (FPL) tendon for the thumb and their flexor synovial sheaths
- Median nerve (MN).
The carpal tunnel is tightly packed and so any condition that increases the volume of the structures inside it can lead to compression of the median nerve resulting in pain and paraesthesia.
Aetiology
- Pregnancy
- Obesity
- Diabetes Mellitus
- Hypothyroidism
- Acute fluid retention
- Connective tissue diseases
- Rheumatoid arthritis
- Local abnormalities/lesions involving the wrist, including previous fractures
Differential Diagnosis
- Cervical radicular pain (C6 or C7): Neck pain, positive Spurlings test
- First Carpometacarpal Joint Osteoarthritis : Painful thumb motion, positive grind test, radiographic findings
- De Quervain Tendinopathy: Tenderness distal radial styloid
- Polyneuropathy: History of diabetes mellitus, bilateral, lower extremity involvement.
- Thoracic Outlet Syndrome: ulnar sided symptoms, positive EAST and ULTT.
- Pronator teres syndrome (median nerve compression at the elbow): Forearm pain; sensory loss over the thenar eminence; weakness with thumb flexion, wrist extension, and forearm pronation
- Ulnar neuropathy: Paresthesias of the ring and little fingers, positive Tinel sign and compression tests at the elbow or wrist (Guyon canal)
- Radial neuropathy
- Raynaud syndrome:Symptoms related to cold exposure, typical color changes
- Vibration white finger:Use of vibratory hand power tools, symptoms of Raynaud phenomenon
- Wrist osteoarthritis: painful wrist motion, radiographic findings
- Inflammatory arthropathy
- Peripheral nerve tumour
- Multiple sclerosis
- Amyotrophic lateral sclerosis
- Acute compression syndromes (eg, Saturday night palsy)
Assessment
- Symptoms are often variable but classically include pain or paraesthesia in the median nerve distribution.
- Neurological examination
- Provocative tests
| Test Name | LR+ | LR- | Sens | Spec | Kappa |
|---|---|---|---|---|---|
| Flick sign | 21 | 0.1 | 93% | 96% | |
| Closed fist sign | 7.3 | 0.4 | 61% | 92% | |
| Hypalgesia | 3.1 | 0.7 | 39% | 88% | |
| Square wrist sign | 2.7 | 0.6 | 53% | 80% | |
| Classic or probable Katz hand diagram | 2.4 | 0.5 | 64% | 73% | |
| Weak thumb adduction | 1.8 | 0.5 | 65% | 65% | |
| Thenar atrophy | 1.6 | 0.9 | 16% | 90% | |
| Abnormal vibration | 1.6 | 0.8 | 36% | 77% | |
| Abnormal monofilament findings | 1.5 | 0.7 | 59% | 59% | |
| Bilateral symptoms | 1.4 | 0.7 | 61% | 58% | |
| Tinel sign | 1.4 | 0.8 | 36% | 75% | |
| Phalen sign | 1.3 | 0.7 | 57% | 58% | |
| Age > 40 years | 1.3 | 0.5 | 80% | 41% | |
| Nocturnal paresthesias | 1.2 | 0.7 | 70% | 43% | |
| 2-point discrimination | 1.2 | 1.0 | 20% | 83% |
Investigations
Not normally required, but can include nerve conduction studies or diagnostic ultrasound. These modalities cannot exclude the condition.
Treatment
Conservative treatment for mild and intermittent symptoms, or symptoms that are likely to resolve soon such as during pregnancy.
- Activity Modification
- Corticosteroid injection
See Carpal Tunnel Injection article.
- Splinting
A hand therapist can provide a custom thermoplastic or the patient can buy an off the shelf splints.
- Manual Therapy
In one study 120 women with carpal tunnel syndrome were randomised to hand therapy versus surgery with no significant differences in pain or function at 1 year and 4 years. The hand therapy group had three 30 minute weekly sessions of physical therapy (figure). The sessions included desensitisation techniques targeted at potential sites of median nerve entrapment, lateral glide mobilisation of the cervical spine, a tendon/nerve gliding exercise, and instructions for a home tendon/nerve gliding exercise. The potential anatomical sites were scalene, pectoralis minor, bicipital aponeurosis, pronator teres, transverse carpal ligament, palmar aponeurosis. At each of these sites the therapist evaluated for pain on palpation and reproduction of sensory or motor symptoms. The surgery group also received the same educational session for performing the tendon/nerve gliding exercises at home.[2][3]
- Surgery (Carpal tunnel release or decompression)
Consider conservative therapy first until severe pain or marked neurological signs. Access to surgery is variable across New Zealand. Surgery may not result in complete recovery of any neurological deficit but may prevent progression.
References
- ↑ D'Arcy & McGee. The rational clinical examination. Does this patient have carpal tunnel syndrome?. JAMA 2000. 283:3110-7. PMID: 10865306. DOI.
- ↑ Fernández-de-Las-Peñas et al.. Manual Therapy Versus Surgery for Carpal Tunnel Syndrome: 4-Year Follow-Up From a Randomized Controlled Trial. Physical therapy 2020. 100:1987-1996. PMID: 32766779. DOI.
- ↑ Fernández-de-Las Peñas et al.. Manual Physical Therapy Versus Surgery for Carpal Tunnel Syndrome: A Randomized Parallel-Group Trial. The journal of pain : official journal of the American Pain Society 2015. 16:1087-94. PMID: 26281946. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,