Carpal Tunnel Syndrome
| Carpal Tunnel Syndrome | |
|---|---|
| Pathophysiology | Entrapment of the median nerve in the carpal tunnel |
| Clinical Features | Sensor loss palmar portion of the first three digits and radial half of the fourth digit plus the distal dorsal aspects of these digits. Weakness of abductor pollicis brevis, opponens pollicis, superficial head of flexor pollicis brevis, lumbricals I/II. Positive Phalen and Tinel's signs. |
Carpal Tunnel Syndrome (CTS) is a common clinical condition that causes pain, numbness, and tingling in the hand. CTS occurs when the median nerve is squeezed or compressed as it travels through the carpal tunnel. It was first described by Paget 1913. Studies by Phalen in the 1950 established the principles of CTS
Epidemiology
It is the most common condition among patients complaining of hand and finger symptoms. It is the most common entrapment neuropathy (90%). It occurs in 4-6% of the general population. The peak age range is 40-60 with 75% of affected patients being female.
Anatomy
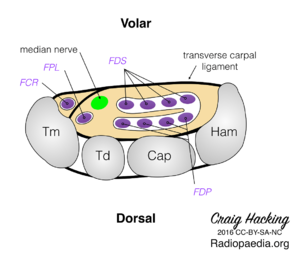
Carpal Tunnel
The carpal tunnel is a non-extendible osteofibrous tunnel surrounded by the following structures
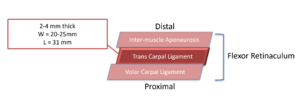
- Roof: flexor retinaculum. There are three continuous segments of the flexor retinaculum.
- The proximal segment is a thickened portion of the deep antebrachial fascia of the forearm.
- The middle segment is the transverse carpal ligament. It is formed by strong interwoven bundles of fibrous connective tissue. It is thick (2-4mm), short (average length is 31mm), and broad (average width is 25mm). It extends from the distal part of the radius to the distal segment of the base of the third metacarpal. The mean proximal limit of its central portion is 11 mm distal to the capitate-lunate joint and the mean distal limit of its distal portion is 10 mm distal to the carpometacarpal joint of the third metacarpal.
- The distal segment is the inter-muscle aponeurosis. It is formed from an aponeurosis which extends distally between the thenar and hypothenar muscles
- Base: carpal sulcus. The base is formed by the capsule and the anterior radiocarpal ligaments cover the underlying portions of the scaphoid, lunate, capitate, hamate, trapezium, and trapezoid.
- Ulnar edge: hamate hook, pyramidal bone and pisiform bone
- Radial edge: scaphoid bone, trapezoid bone and tendon of the flexor carpi radialis (FCR) muscle.
The tunnel gives passage to:
- Eight digital flexor tendons (two for each of the medial four fingers)
- Flexor pollicis longus (FPL) tendon for the thumb and their flexor synovial sheaths
- Median nerve (MN).
The carpal tunnel is tightly packed and so any condition that increases the volume of the structures inside it can lead to compression of the median nerve resulting in pain and paraesthesia.
Median Nerve
The median nerve supplies sensation to the palm of the hand, the distal dorsal aspect of the lateral three and half digits, and the lateral palm. It provides motor innervation to abductor pollicis brevis, opponens pollicis, flexor pollicis brevis, and the lateral lumbricals.
The median nerve runs along the middle of the arm and forearm to the hand. It is formed from the lateral and medial cords of the brachial plexus, deriving fibres from C6-T1. The lateral and medial cords unite either in front of or lateral to the axillary artery.
In the proximal arm it is found lateral to the brachial artery. At the level of the insertion of the corachobrachialis it crosses the artery. It then lies on the medial side of the flexor elbow crease behind the lacertus fibrosus. The brachialis muscle separates it from the elbow joint.
In the forearm it runs between the two heads of pronator teres, crosses the ulnar artery, and descends beneath the flexor digitorum superficialis. It lies on the floor of the flexor digitorum profundus to within 5cm of the transverse carpal ligament. At this point it becomes more superficial, being found between the tendons of flexor digitorum superficialis and flexor carpi radialis. Here it lies radial to the tendon of palmaris longus and passes under the transverse carpal ligament into the hand.
The palm of the hand is unaffected by carpal tunnel syndrome because it is supplied by the sensory cutaneous branch of the median nerve. This branch arises about 6cm proximal to the transverse carpal ligament and passes superficially to the ligament. Therefore it isn't affected by pressure changes within the carpal tunnel.
The median nerve is accompanied by the median artery and a branch of the volar interosseous artery. It is also accompanied by four tendons from the superficial flexors of the fingers, four tendons from the deep flexors of the fingers and the long flexor of the thumb. The long flexor of the thumb is the most radial element. The ulnar artery is in a superficial position, under the fascia and above the muscle.
At the entrance to the carpal tunnel, the median nerve is located dorsal to the palmaris longus or between the flexor carpi radialis and the palmaris longus. In a neutral wrist position the median nerve is volar to the superficial flexor of the index finger, or between the long flexor of the thumb and the superficial flexor of the index finger, or in front of the superficial flexor of the middle finger. In the distal part of the tunnel, the medial nerve divides into six branches: the motor or thenar branch; three specific palmar digital nerves (radial and ulnar of the thumb and radial of the index finger); and the common palmar digital nerves of the second and third spaces. The thenar branch passes through a separate tunnel before entering the thenar muscles, in 56% of the cases.[1]
Anatomic Variations
Understanding anatomic variations is important because it can help to explain the variable clinical presentation and also reduce the risk of iatrogenic injury.
Median nerve variations
Lanz classified the variations of the motor (thenar) branch of the median nerve. There is the extraligamentous form, which is the most frequent type (46%); the subligamentous form (31%) and the transligamentous form (23%). There are two motor branches that cross the flexor retinaculum in 4% of cases. The nerve bundles destined for the thenar branch are located radially to the median nerve in 60% of the cases, anteriorly in 20% and centrally in 18%.9 Sometimes, the thenar branch passes through a tunnel before entering the thenar muscles. These variations may explain the variable motor impact in cases of severe compression of the median nerve.[1]
Berrettini anastomosis
Here there is an anastomosis with the sensory ulnar nerve in the palm and is found in 67-92% of cases. The anastomosis is situated below the superficial palmar arch and is responsible for variations in the sensory supply at the level of the ulnar edge of the 3rd and 4th fingers and the radial edge of the 5th finger between the median and ulnar nerves. In some cases the anastomosis is immediately distal to the flexor retinaculum.[1]
Riche and Cannieu motor anastomosis
This is an anastomosis with the sensory ulnar nerve in the hand and is found in 77-100% of people. It is responsible for the distribution of innervation of the thenar muscles between median and ulnar nerves.
There are a variety of forms. The most classical is a communicating branch between thenar branch and deep branch of the ulnar nerve. Other forms are an anastomosis at the level of the adductor muscles of the thumb, between the thenar branch and the deep branch of the ulnar nerve at the level of the first lumbrical muscle, and between a collateral nerve of the thumb and the deep branch of the ulnar nerve.[1]
Martin Gruber median ulnar anastomosis
This is an anastomosis with the sensory ulnar nerve in the forearm and is found in 5-40% of cases. The anastomosis comes from the median nerve or anterior interosseous nerve, or is situated between the branches that innervate the deep flexors of the fingers. This anastomosis coexists most frequently with an anastomosis in the hand and contains fibres that innervate the deep flexors of the fingers and the intrinsic muscles. There is controversy regarding the participation of sensory fibres. Inverse anastomoses from the ulnar nerve to the median nerve are very rare and are situated in the distal part of the forearm.[1]
Vascular variations
The persistence of the artery of the median nerve is leftover from the embryonic stage and is observed in 1–16% the cases. A bifid median nerve may be found together with this artery. The complication produced is thrombosis, which gives rise to acute carpal tunnel syndrome.[1]
Muscle and tendon variations
The palmaris tendon is absent in 14% of individuals. There is a variation of the palmaris longus with an intratunnel tendon called the deep palmaris longus muscle. This inserts in the deep face of the palmar aponeurosis and can lead to median nerve compression. The palmaris longus can also be in an inverse position with intratunnel muscle bodies.
Aetiology
Aetiology can be thought of as idiopathic versus secondary, plus acute.
Idiopathic: This is related to Gender (hormonal effects, relative wrist size), age (menopausal), genetic influences (IL 6 expression - collagen abnormalities), anatomic variation, and anthropometric parameters.
Secondary: Secondary is divided into problems with the Content or Container.
Container
- Shape of the carpal bones and distal radius-ulna
- Joint abnormalities: joint subluxations, wrist arthrosis, inflammatory arthritis, infectious arthrosis, villonodular synovitis
- Acromegaly
Content
- Tenosynovial hypertrophy
- Inflammatory: infection, autoimmune
- Metabolic: Diabetes mellitus, amyloidosis, gout, chondrocalcinosis
- Fluid distribution: Pregnancy, hypothyroidism, kidney failure
- Space occupying lesion: abnormal or supernumerary muscle, persistent arterial hypertrophy, aneurysms, infra-tunnel tumour (lipoma, synovial cyst, sarcoma, neural tumour), haematoma, obesity
- Increased pressure: wrist flexion and extension, RSI with incursion of muscle belly of flexor tendons, vibration effects with microcirculatory compression and intraneural oedema
Acute Carpal Tunnel Syndrome
- Trauma
- Infection
- Haemorrhage
- Iatrogenic
- Thrombosis of median artery
- Burns
- Increased pressure
Pathophysiology
Pressure Change: The normal internal carpal pressure is 2-10mmHg. Wrist positions change pressure dramatically: wrist flexion increases the pressure by eight times and wrist extension by 10 times. There is a pressure increase due to a change in the carpal tunnel cross sectional area and a change in the volume of the carpal tunnel due to tissue changes and oedema.
Cross-Sectional Area: In women the cross-sectional area is significantly smaller as well as disproportionally smaller for body size. The risk of carpal tunnel syndrome is elevated around menopause, pregnancy, bilateral oophorectomy, oral contraceptives, and HRT. Estrogen receptor alpha is expressed in the transverse carpal ligament and flexor synovium. Upregulation of the receptors in tenosynovial tissue is associated with carpal tunnel syndrome.
Inflammation: Inflammation may be involved in the pathophysiology. There may be tenosynovitis from autoimmune diseases or repetitive movement. Hypertrophy of synovial lining of flexor tendons in the carpal tunnel can occur. Increased levels of inflammatory markers found (Interleukin 6, Prostaglandin E-2, Vascular endothelia growth factor). This leads to an increase in fibroblast density, type 3 collagen, and vascular proliferation.
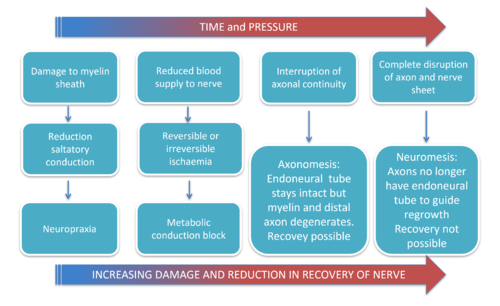
Blood-Nerve Barrier: Compression of the median nerve can lead to blood-nerve barrier injury as well as ischaemic injury. The Blood-Nerve Barrier is formed by the inner cells of the perineurium. There are tight junctions of the endo-neural micro-vessels. It's function is to regulate the intra-neural environment and provide immune protection. Breakdown results in an increase in intra-fascicular pressure and oedema, as well as an interference with microcirculation leading to mini compartmental syndrome. High risk in patients with pre-existing vascular conditions.
Ischaemic Injury: Ischaemic injury plus mechanical contact pressure leads to various effects. It causes axonal injury and changes to the myelin sheath that is detectable on nerve conduction studies. Early compression of the venous system leads to outflow obstruction. This increases pressure as blood accumulates, ultimately blocking flow in the vasa nervorum leading to ischaemia.
Tethering: Median nerve tethering is thought to be important in the pathophysiology. The median nerve moves up to 9.6mm in flexion. Nerve gliding is crucial for physical activity. Gliding prevents excessive stretch of nerve. Chronic compression of the nerve causes fibrosis. Mesoneural scarring causes the median nerve to adhere to surrounding tissue. This leads to traction during wrist movement.
Differential Diagnosis
- Cervical radicular pain (C6 or C7): Neck pain, positive Spurlings test
- First Carpometacarpal Joint Osteoarthritis : Painful thumb motion, positive grind test, radiographic findings
- De Quervain Tendinopathy: Tenderness distal radial styloid
- Polyneuropathy: History of diabetes mellitus, bilateral, lower extremity involvement.
- Thoracic Outlet Syndrome: ulnar sided symptoms, positive EAST and ULTT.
- Pronator teres syndrome (median nerve compression at the elbow): Forearm pain; sensory loss over the thenar eminence; weakness with thumb flexion, wrist extension, and forearm pronation
- Ulnar neuropathy: Paresthesias of the ring and little fingers, positive Tinel sign and compression tests at the elbow or wrist (Guyon canal)
- Radial neuropathy
- Raynaud syndrome:Symptoms related to cold exposure, typical color changes
- Vibration white finger:Use of vibratory hand power tools, symptoms of Raynaud phenomenon
- Wrist osteoarthritis: painful wrist motion, radiographic findings
- Inflammatory arthropathy
- Peripheral nerve tumour
- Multiple sclerosis
- Amyotrophic lateral sclerosis
- Acute compression syndromes (eg, Saturday night palsy)
Clinical Features
Clinical Stages
The condition has been described to occur in three stages.
Early or First Stage:
- Awaken from sleep with feeling of numb or swollen hand.
- Severe pain in their wrist radiating to their upper arm and or shoulder.
- "Tingling” in their hand and finger.
- Flicking the hand with stop the pain.
- Hand may feel stiff in the morning.
- Symptoms are often variable but classically include pain or paraesthesia in the median nerve distribution.
- Neurological examination
- Provocative tests
Second Stage:
- Daytime symptoms.
- Increase with respective movement or prolonged static positions.
- Might remark on clumsiness, dropping objects.
Third Stage
- Atrophy of the thenar eminence.
- Sensory symptoms might no longer be present.
Physical Examination
| Test Name | LR+ | LR- | Sens | Spec | Kappa |
|---|---|---|---|---|---|
| Flick sign | 21 | 0.1 | 93% | 96% | |
| Closed fist sign | 7.3 | 0.4 | 61% | 92% | |
| Hypalgesia | 3.1 | 0.7 | 39% | 88% | |
| Square wrist sign | 2.7 | 0.6 | 53% | 80% | |
| Classic or probable Katz hand diagram | 2.4 | 0.5 | 64% | 73% | |
| Weak thumb adduction | 1.8 | 0.5 | 65% | 65% | |
| Thenar atrophy | 1.6 | 0.9 | 16% | 90% | |
| Abnormal vibration | 1.6 | 0.8 | 36% | 77% | |
| Abnormal monofilament findings | 1.5 | 0.7 | 59% | 59% | |
| Bilateral symptoms | 1.4 | 0.7 | 61% | 58% | |
| Tinel sign | 1.4 | 0.8 | 36% | 75% | |
| Phalen sign | 1.3 | 0.7 | 57% | 58% | |
| Age > 40 years | 1.3 | 0.5 | 80% | 41% | |
| Nocturnal paresthesias | 1.2 | 0.7 | 70% | 43% | |
| 2-point discrimination | 1.2 | 1.0 | 20% | 83% |
Investigations
Not normally required, but can include nerve conduction studies or diagnostic ultrasound. These modalities cannot exclude the condition.
Treatment
Conservative treatment for mild and intermittent symptoms, or symptoms that are likely to resolve soon such as during pregnancy.
- Activity Modification
- Corticosteroid injection
See Carpal Tunnel Injection article. Several systemic review support local carpal tunnel corticosteroid injection as an effective treatment for carpal tunnel syndrome. The evidence does not support one injection technique over another or a particular steroid formulation. Ultrasound-guided injection may be safer than blind injection and allows for direct visualization to ensure accurate and safe needle placement. Although injection is generally safe, there is risk of median nerve injury and tendon rupture. A repeat injection in the same wrist may be offered after six months. If symptoms recur after two injections, another treatment or surgery should be considered.
PRP injection
PRP is not superior to wrist splinting.[3]
- Splinting
A hand therapist can provide a custom thermoplastic or the patient can buy an off the shelf splints. Night splinting to maintain the wrist in a neutral position is suitable for mild to moderate carpal tunnel syndrome and this is supported by level 1 evidence.
- Manual Therapy
In one study 120 women with carpal tunnel syndrome were randomised to hand therapy versus surgery with no significant differences in pain or function at 1 year and 4 years. The hand therapy group had three 30 minute weekly sessions of physical therapy (figure). The sessions included desensitisation techniques targeted at potential sites of median nerve entrapment, lateral glide mobilisation of the cervical spine, a tendon/nerve gliding exercise, and instructions for a home tendon/nerve gliding exercise. The potential anatomical sites were scalene, pectoralis minor, bicipital aponeurosis, pronator teres, transverse carpal ligament, palmar aponeurosis. At each of these sites the therapist evaluated for pain on palpation and reproduction of sensory or motor symptoms. The surgery group also received the same educational session for performing the tendon/nerve gliding exercises at home.[4][5]
See open access article by Mehner and Lewis for the American osteopathic medicine approach to treating carpal tunnel syndrome.[6]
- Surgery (Carpal tunnel release or decompression)
Consider conservative therapy first until severe pain or marked neurological signs. Access to surgery is variable across New Zealand. Surgery may not result in complete recovery of any neurological deficit but may prevent progression.
Surgery is the treatment of choice for patients with severe median nerve damage, permanent sensory or motor loss, or ongoing axonal loss or denervation on electrodiagnostic studies. Endoscopic and open techniques are equally effective; however, patients return to work on average eight days earlier with endoscopic repair than with open repair. However there is an increased risk of nerve and vascular injury with endoscopic techniques.
The most common complications are a painful scar and pillar pain (pain adjacent to the site of ligament release). Most patients note significant improvement in one week and are able to return to normal activities in two weeks. However, some patients (especially those with severe CTS) take up to one year to recover fully. Carpal tunnel decompression provides a lasting, good outcome in 70% to 90% of cases.
Ultrasound guided carpal tunnel release is a novel treatment.
Summary
- Knowledge of anatomy variations.
- Consider the pathophysiology for individual patients to improve treatment plan.
- Diagnosis is mostly clinical.
- Combination of examination tests rather than single tests improves diagnostic accuracy.
- US useful in some conditions and for CT injections
- NCS and EMG for atypical cases.
- Splints and steroid injections useful relief in mild to moderate CTS.
- Surgery if failing conservative or severe CTS
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Chammas, Michel et al. “Carpal tunnel syndrome - Part I (anatomy, physiology, etiology and diagnosis).” Revista brasileira de ortopedia vol. 49,5 429-36. 20 Aug. 2014, doi:10.1016/j.rboe.2014.08.001
- ↑ D'Arcy & McGee. The rational clinical examination. Does this patient have carpal tunnel syndrome?. JAMA 2000. 283:3110-7. PMID: 10865306. DOI.
- ↑ Raeissadat, Seyed Ahmad et al. “Safety and efficacy of platelet-rich plasma in treatment of carpal tunnel syndrome; a randomized controlled trial.” BMC musculoskeletal disorders vol. 19,1 49. 13 Feb. 2018, doi:10.1186/s12891-018-1963-4
- ↑ Fernández-de-Las-Peñas et al.. Manual Therapy Versus Surgery for Carpal Tunnel Syndrome: 4-Year Follow-Up From a Randomized Controlled Trial. Physical therapy 2020. 100:1987-1996. PMID: 32766779. DOI.
- ↑ Fernández-de-Las Peñas et al.. Manual Physical Therapy Versus Surgery for Carpal Tunnel Syndrome: A Randomized Parallel-Group Trial. The journal of pain : official journal of the American Pain Society 2015. 16:1087-94. PMID: 26281946. DOI.
- ↑ Mehner TR, Lewis DD. Osteopathic Approach to Treatment of Carpal Dysfunction: The Carpal Mobilization Technique. J Am Osteopath Assoc. 2020 Nov 1;120(11):783-784. doi: 10.7556/jaoa.2020.120. PMID: 32877924.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,