Caudal Epidural Steroid Injection
| |
| Caudal Epidural Steroid Injection | |
|---|---|
| Indication | Lumbar Radicular Pain, Lumbar Spinal Stenosis, Chronic Low Back Pain |
| Needle path | Through sacrococcygeal ligament into sacral hiatus |
| Syringe | 20mL |
| Needle | 21G 40mm, or 25G 50mm |
| Steroid | Dexamethasone 15mg or triamcinolone 40-80mg |
| Local | No local or bupivicaine 0.5% 3mL, add normal saline to add volume |
| Volume | S1: 5-10mL L5: 10mL L4: 15mL |
Available approaches to access the epidural space are caudal, interlaminar, and transforaminal. The caudal approach allows a relative easy access and minimal risk of dural puncture. It involves placing a needle through the sacral hiatus to reach the epidural space.
Anatomy
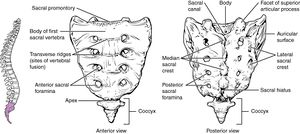
The sacrum has five fused vertebrae and has a dorsal convex curve. The coccyx has three to five rudimentary vertebral bones, with a base that attaches to the sacrum, and has a triangular shape.
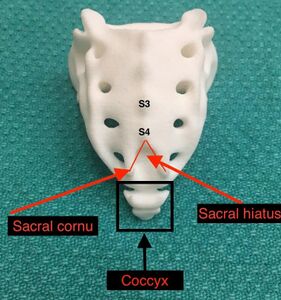
The sacral hiatus sits between the sacral cornua. The sacral hiatus is a natural partial defect that arises from the union of the dorsal midline of the S4 and S5 vertebrae. The floor of the sacral hiatus is the S5 vertebral body. It contains the filum terminale and coccygeal nerve. The roof contains the sacrococcygeal ligament.
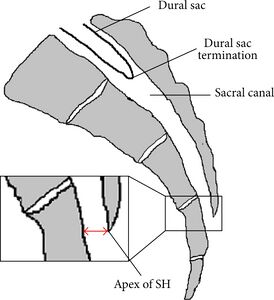
The sacral canal contains the epidural venous plexus that extends down to the S4 level, and is concentrated in the anterior wall of the sacral canal. It also contains epidural fat. The thecal sac generally terminates at the lower border of the S1 foramen in adults and S3 foramen in children. The PSIS is at the level of S2. Thecal sac puncture should be avoided.[1]
Indications and Efficacy
Caudal epidural steroid injection has been used in radicular leg pain, axial pain (internal disc disruption), and spinal stenosis. There is balanced evidence supporting the effectiveness in managing low back pain and radicular pain. A systematic review in 2012 found that "for lumbar disc herniation, the evidence is good for short- and long-term relief of chronic pain secondary to disc herniation or radiculitis with local anesthetic and steroids and fair relief with local anesthetic only. In managing chronic axial or discogenic pain, spinal stenosis, and post surgery syndrome, the indicated evidence is fair."[2]
There are several advantages for the caudal approach. These include the ease of entry, minimal risk of inadvertent dural puncture, it has been well studied, and it may be safer than other epidural approaches for those with coagulopathies or those on anticoagulants.[1]
There are also some disadvantages to this approach. High volume of fluid is generally needed. The S1 nerve is usually covered by the injectate (82% in nonsurgical and 88% in postsurgical patients), but there is a much lower chance of filling the L5 nerve (12% of nonsurgical and 30% of surgical). So overall it is only suitable for lower lumbar and sacral pathology. The possibility of incorrect needle placement is another disadvantage when done under landmark guidance. See complications for risks.[1]
A recent RCT found that caudal injections were more efficacious than selective nerve root injections.[3] In an RCT by Murakibhavi et al they used landmark guidance but checked needle placement with a C-arm, but without contrast injection, so it wasn't a full image guided injection. They compared caudal epidural to conservative management, at 12 months complete relief was found in 86% of the caudal group and 24% of the conservative care group. At three weeks it was 92% vs 32%.[4]
Contraindications
The following are factors that predispose to dural puncture in caudal epidural injections.[1]
- Short stature (height less than 5 feet)
- Short sagittal dimension of the sacrum
- Blind injection without imaging guidance
- Inexperienced operator
- Tip of the needle above the level of the anterior foramen of S1 in AP view on fluoroscopy
- Atypical anatomy within the sacral canal, including presence of a tethered cord.
The following are potential causes of difficulty entering the caudal epidural space.[1]
- Acute angle of sacral dorsal convexity
- Inability to identify anatomic landmarks
- Severe to morbid obesity blocking radiologic (fluoroscopic) visualisation
- Deformity of sacral coccygeal area secondary to previous
- Trauma or birth defect
- Sealed sacra; hiatus, seen in 2-3%.[5]
- Relatively long coccyx with “superior” location of sacral hiatus
- Developmental fusion of sacral canal
- Being elderly due to reduced AP diameter of the sacral hiatus[5]
Pre-procedural Evaluation
Usual volume is 5-25mL. Lower volumes are used in the elderly and short statured. Higher volumes are used when the pathology is at the lower upper lumbar level. 10mL can be used for reaching the L5 segment, and 15mL for reaching the L4 segment. However there is some evidence that increasing volumes does not seem to improve the filling pattern.[1]
Technique
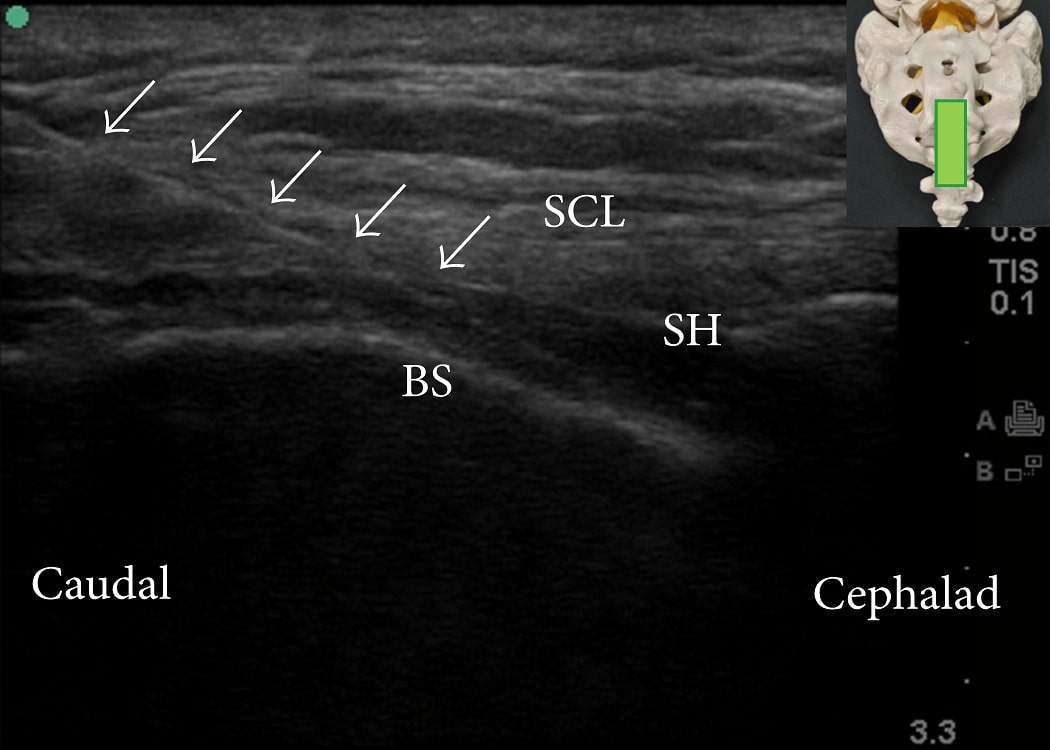
Ultrasound Guided
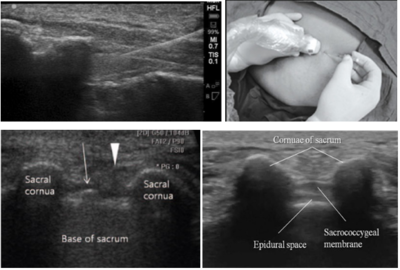
Ultrasound has very high success rates reported to be 96.9-100%. The main difficulty with the ultrasound guided technqiue arises in elderly individuals where the AP diameter of the sacral hiatus is significantly smaller.[5]
- Position: prone with heels rotated laterally, and a cushion pillow is used as an iliac wedge.
- Identify sacral cornua at base of imaginary triangle with thumb (needle will go between cornua)
- Obtain a transverse image for the sacral hiatus and dorsal sacrococcygeal ligament between the bilateral sacral cornua,
- Obtain a longitudinal view and advance needle at a 45 degree angle.
- Terminate needle advancement right after piercing the sacrococcygeal ligament. This is to avoid injection into the venous plexus and intrathecal injection in those with unusually low terminating dural sacs.
- Aspirate to ensure needle not penetrated thecal sac or blood vessel. If aspirate CSF then abort procedure and retry in one week.
- Inject solution, can use doppler to confirm correct injectable positioning and flow.
Landmark Guided
Difficulties
- Inaccurate needle placement is reported in 9-38%, even in experienced operators.[1]
- This technique should not be attempted if the landmarks cannot be palpated, such as in obesity. The cornuae are impalpable bilaterally in around 50% of adults.[5] It is more successful in children, possibly due to more easily palpable landmarks[5]
- The AP diameter decreases with age and so being elderly is another relative contraindication.[4]
- A shorter sacrococcygeal ligament is associated with difficulty with landmark guidance.[4]
Technique
- Patient in prone or lateral decubitus position
- Draw a line to connect the bilateral PSIS to mark one side of an equilateral triangle
- Find and mark cornuae and sacral hiatus which is at the apex of the equilateral triangle. The cornuae are two bony prominences, and the sacral hiatus is a dimple in between them.
- Infiltrate lidocaine to overlying soft tissue with 2-3mL of lidocaine without adrenaline
- Enter at midline between the sacral cornu at about a 45° angle with the bevel of the needle facing ventrally until contact with the sacral triangle.
- Redirect the needle more cephalad, horizontal, and parallel to the table until it passes through the sacrococcygeal ligament into the epidural space.
- Confirm needle placement using one or several of the following methods:[4]
- Loss of resistance with piercing the sacrococcygeal ligament
- Aspiration test - there should be no CSF aspiration, if CSF is aspirated then the needle has punctured the dura. If blood is aspirated then it has punctured a blood vessel.
- "whoosh" test: Inject air into the caudal epidural space while simultaneously auscultating over the thoracolumbar spine (sensitivity of 80% and specificity of 60%). However this has a risk of causing portal vein air embolism and motor weakness.[5]
- Palpating for subcutaneous bulging on rapid injection of 5mL air or saline has a PPV of 83% and NPV of 44%.[5]
- Hanging drop test: - A drop of injected saline staying at the Luer-lock of the needle and not getting sucked in or expressed together with other fluid.
- Inject solution. Look for bulging at the sacrum to indicate inadvertent subcutaneous injection. If there is resistance then the needle may be subperiosteal.
Fluoroscopic Guidance
The advantage of fluoroscopy over ultrasound is that one can use contrast to confirm that the injectate reaches the target disc level. The technique described by Ogoke is as follows[1]
- Position: patient prone or in lateral decubitus with hip flexed
- Strict aseptic technique is required
- Palpate the sacral cornu, and infiltrate with local anaesthetic using a 25-G 1.5 inch needle
- Consider preparing the epidural needle by creating a convexity at the first 1 inch of the needle (epidural Tuohy), and then producing another convexity that is more diffuse throughout the remainder of the needle.
- Advance the epidural needle and confirm radiographically with AP and lateral views before advancement
- May feel a "pop" when passing through the sacral-coccygeal ligament
- After puncture, slowly reduce the angle of the entire needle by bringing the hub of the needle closer to the horizontal plane and attempt to pass the needle forward.
- The tip of the needle may touch the roof of the sacral canal. Withdraw the needle by 2-3mm and rotate 180 degrees, then advance forward slowly to the desired level under fluorscopic guidance.
- The lateral view is useful for confirming the needle is in the epidural space. The AP view is good for confirming the level that the tip of the needle is at relative to the expected location of the thecal sac.
- Confirm needle location by loss-of-resistance technique using a puff of air or saline.
- Aspirate with a 2mL syringe to exclude intravascular placement.
- Inject 5-25mL
- Monitor in supine position for cardiorespiratory stability.
Complications
- Infection
- Subcutaneous injection
- Spinal cord infarction
- Nerve injury - rare, likely unrelated to the procedure when present.
- Allergic reaction or ADR from steroids
- Intravascular injection (minimal risks with dexamethasone due to small particulate size)
- Intra-osseous injection and subsequent Local Anaesthetic Toxicity
- Intra-thecal injection with prolonged and/or high subarachnoid block, respiratory distress or arrest, and total spinal anaesthesia. An early sign is the patient's inability to evaluate the lower extremity soon after the injection and being unable to push up the knees in a supine position. Most patients will feel lower extremity numbness, not expected for epidural injection[1]
- Dural puncture with headache
- PE
- Post-injection pain at the sacral hiatus. This may be prolonged but doesn't usually persist for longer than 2-6 months.[1]
Aftercare
Monitor for allergy. Advised to keep active within pain limits, and is reassessed about 10 days later. Steroid remains in situ for about 2 weeks.
Up to 3-4 injections may be performed before declaring the therapy a failure. Max 0.6mg/kg or 40mg dexamethasone per year.
Methylprednisolone and triamcinolone are more effective than dexamethasone by the second injection. Dexamethasone requires a third injection in a significant number of cases.[6]
Videos
See Also
- Lumbar Radicular Pain
- Lumbar Transforaminal Epidural Steroid Injection
- Ultrasound Guided Caudal Anaesthesia : WFSA - Resources (wfsahq.org) - focus on paediatrics.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Ogoke. Caudal epidural steroid injections. Pain physician 2000. 3:305-12. PMID: 16906188.
- ↑ Parr et al.. Caudal epidural injections in the management of chronic low back pain: a systematic appraisal of the literature. Pain physician 2012. 15:E159-98. PMID: 22622911.
- ↑ Singh S, Kumar S, Chahal G, Verma R. Selective nerve root blocks vs. caudal epidural injection for single level prolapsed lumbar intervertebral disc - A prospective randomized study. J Clin Orthop Trauma. 2017 Apr-Jun;8(2):142-147. doi: 10.1016/j.jcot.2016.02.001. Epub 2016 Feb 22. PMID: 28720990; PMCID: PMC5498739.
- ↑ 4.0 4.1 4.2 4.3 Murakibhavi, V. G.; Khemka, Aditya G. (2011-11). "Caudal epidural steroid injection: a randomized controlled trial". Evidence-Based Spine-Care Journal. 2 (4): 19–26. doi:10.1055/s-0031-1274753. ISSN 1663-7976. PMC 3506149. PMID 23230402. Check date values in:
|date=(help) - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Kao, Sheng-Chin; Lin, Chia-Shiang (2017). "Caudal Epidural Block: An Updated Review of Anatomy and Techniques". BioMed Research International. 2017: 9217145. doi:10.1155/2017/9217145. ISSN 2314-6141. PMC 5346404. PMID 28337460.
- ↑ Datta & Upadhyay. A Randomized Clinical Trial of Three Different Steroid Agents for Treatment of Low Backache through the Caudal Route. Medical journal, Armed Forces India 2011. 67:25-33. PMID: 27365757. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,