Cervical Radicular Pain and Radiculopathy: Difference between revisions
mNo edit summary |
m (→References) |
||
| Line 194: | Line 194: | ||
=== Surgery === | === Surgery === | ||
There is only one randomised controlled trial using an active control rather than sham control. The findings were some improvement at 3-4 months over conservative therapy, but none at 12 months. Only 8% complete relief, 19% improved, 42% unchanged and 31% worse.<ref>Peolsson A, Öberg B, Wibault J, Dedering Å, Zsigmond P, Bernfort L, Kammerlind AS, Persson LC, Löfgren H. Outcome of physiotherapy after surgery for cervical disc disease: a prospective randomised multi-centre trial. BMC Musculoskelet Disord. 2014 Feb 6;15:34. doi: 10.1186/1471-2474-15-34. PMID: 24502414; PMCID: PMC3923245.</ref> Surgery might be considered for chronic symptoms but it shouldn't be promoted as a cure for the majority of cases. | There is only one randomised controlled trial using an active control rather than sham control. The findings were some improvement at 3-4 months over conservative therapy, but none at 12 months. Only 8% complete relief, 19% improved, 42% unchanged and 31% worse.<ref>Peolsson A, Öberg B, Wibault J, Dedering Å, Zsigmond P, Bernfort L, Kammerlind AS, Persson LC, Löfgren H. Outcome of physiotherapy after surgery for cervical disc disease: a prospective randomised multi-centre trial. BMC Musculoskelet Disord. 2014 Feb 6;15:34. doi: 10.1186/1471-2474-15-34. PMID: 24502414; PMCID: PMC3923245.</ref> Surgery might be considered for chronic symptoms but it shouldn't be promoted as a cure for the majority of cases. | ||
== See Also == | |||
* [[Lumbar Radicular Pain]] | |||
* [[Radicular Pain and Radiculopathy]] | |||
* [[Neuropathic Pain]] | |||
* [[Acute Low Back Pain]] | |||
* [[Chronic Low Back Pain]] | |||
==References== | ==References== | ||
Revision as of 18:23, 17 September 2021
Cervical radicular pain is pain perceived as arising in a limb or the trunk wall caused by ectopic activation of nociceptive afferent fibres in a spinal nerve or its roots or other neuropathic mechanisms. Cervical radiculopathy is the objective loss of function in some combination of sensory loss, motor loss, or impaired reflexes, in a segmental distribution. Pain is not a component of radiculopathy, and so it can be helpful to distinguish it from cervical radicular pain.[1] (See also Cervical Spine Pain Definitions and Radicular Pain and Radiculopathy to be clear on taxonomy)
Pathophysiology
Less is known about the causes and mechanisms of cervical radicular pain compared to lumbar radicular pain.
Mechanism of Pain and Radiculopathy
The literature often uses the term cervical radiculopathy, but radiculopathy and radicular pain are not synonymous.
Radiculopathy arises from either direct compression of a cervical spinal nerve or root, or by ischaemia from vascular injury to their blood supply. There is a conduction block along the affected axons which results in sensory or motor loss. Compression of axons, including those of the lumbar nerve roots, does not cause activity in nociceptive afferent fibres. Meanwhile, compression of a dorsal root ganglion does cause pain through activation of Aβ, Aδ, and C fibres. The causes of cervical radicular pain cannot therefore be attributed to the same causes as those of radiculopathy.
It is thought that inflammation of the cervical nerve roots is the underlying mechanism through which radicular pain occurs secondary to disc herniation. Pro-inflammatory molecules have been found in disc material, however unlike with lumbar radicular pain it hasn't been explicitly shown that cervical radicular pain is inflammatory in origin.
Meanwhile, inflammation cannot be the cause of pain in other causes of radicular pain when due to tumours, cysts, and osteophytes. In these conditions it must be through dorsal root ganglion compression that pain occurs, as these conditions are non-inflammatory in nature.[1]
"Hard" and "Soft" Processes
Soft protrusion are lesions in which the disc material, ostensibly the nucleus pulposus, is extruded into the vertebral canal. The extrusion can be medial or lateral. With medial protrusions the effect is primarily on the spinal cord and myelopathy may occur, while pain is uncommon or inconspicuous. With lateral protrusions there is impingement on the spinal nerve and its roots in the intervertebral foramen, and this is regularly associated with pain.
In cervical spondylosis there may be narrowing of the cervical vertebral canal and the cervical intervertebral foramina due to
- Osteophytes of the zygapophysial joints or the uncinate process
- Hard protrusions of the intervertebral discs. This consists of osteophytes from the margins of the vertebral bodies or fibrocartilaginous or osseous bars that protrude transversely across the back of the disc - i.e. "hard disc"
Aetiology
- Disc
- Protrusion
- Osteophytes
- Facet joint
- Osteophytes
- Ganglion
- Tumor
- Rheumatoid arthritis
- Gout
- Ankylosing spondylitis
- Fracture
- Vertebral body
- Tumor
- Paget’s disease
- Fracture
- Osteomyelitis
- Hydatid
- Hyperparathyroidism
- Meninges
- Cysts
- Meningioma
- Dermoid cyst
- Epidermoid cyst
- Epidural abscess
- Epidural hematoma
- Blood vessels
- Angioma
- Arteritis
- Nerve sheath
- Neurofibroma
- Schwannoma
- Nerve
- Neuroblastoma
- Ganglioneuroma
The most common cause of cervical radiculopathy is intervertebral disc herniation. It is not completely clear why some people with disc herniation develop radiculopathy while others don't but it appears that an inflammatory response can lead to neurophysiologic dysfunction.
The second most common cause is degenerative change. This includes ligamentous hypertrophy, hyperostosis, disc degeneration, facet joint hypertrophy, and uncovertebral joint hypertrophy. Hypertrophy of the latter two structures can lead to foraminal stenosis and nerve root compression. Osteophytosis can also be involved in compression.
Other causes are less common such as facet joint cysts, trauma, haematomas, fibroproliferation, and various tumours.[2]
Epidemiology
The most commonly affected nerve roots are C6 and C7. The pre-test probability of C7 is 54%. C4 and C8 are rare. C5 is variable.
The incidence estimated as 5.5 per 100,000 population per year.
Trauma is the alleged cause in fewer than 20% of cases
Risk Factors associated with cervical disc prolapse are diving, coughing and heavy lifting. There is a trend with golfing, smoking, manual labour, driving, and using vibrating tools. There is no association with psychosocial factors.
Clinical Features
Radicular pain is strongly associated with neurological signs, such as numbness, weakness and hyporeflexia. Neck pain alone, or pain in the shoulder girdle or proximal regions of the upper arm is more likely to be somatic referred pain (see Acute Neck Pain and Chronic Neck Pain)
Pain Pattern
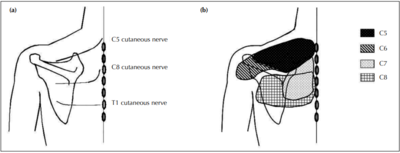
(b) The site of radicular pain involving the C6 root overlaps with that of the C5 root, and also involves the posterior deltoid.[3]
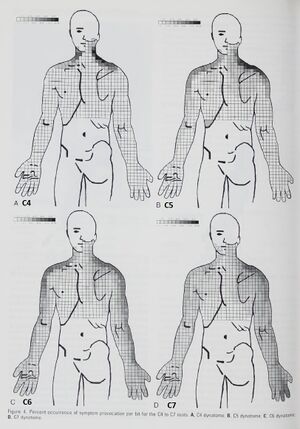
The pattern of cervical radicular pain is not dermatomal, but rather dynatomal (figure 3). The pain is typically in the neck (89% in one surgical series[5]) and arm , but can also be felt in the head, shoulder girdle, and the anterior chest.[5]
- With dorsal root pain the quality is described as lightning or electric-shocks, with radiation along the entire length of the upper arm. Proximally the pain is diffuse, but peripherally it is distinct where it typically involves the hand.
- With ventral root pain the pain is never felt distally. It is deep and boring, and perceived over the scapula and/or dorsal arm.
Proximal pain in the scapula and shoulder girdle usually precedes pain in the arm and/or fingers (figure 2). This is analogous to the common finding of buttock pain with lumbar radicular syndrome. The reason it is not dermatomal is likely due to the pain not being restricted to cutaneous fibres, but there is also a deeper pain arising from the muscles and joints.
The segmental innervation of the skin (dermatomes) is different to that of the deeper tissues. The muscles of the shoulder girdle are supplied by C6 and C7, very different to their dermatomes. See C6 and C7 columns in the complete myotome chart, and note how for example latissimus dorsi receives innervation from C6-C8. As such, the segmental innervation of the muscles is more closely related to the radicular pain patterns than the segmental innervation of the skin (dermatomes). Dermatomes are more helpful for patterns of sensory loss in radiculopathy.[1][3]
The site of scapula pain may be a helpful data point in determining the affected level in cervical radicular pain (table 1). Mizutamari et al suspect that scapula pain occurs through the medial branches of the dorsal rami of the cervical nerves. They found that there was no cutaneous course of C6 and C7 and that these patients complained of deep scapula pain only. This is compared to patients with C5 and C8 lesions having both superficial and deep pain.[3]
| Nerve root | Shoulder Girdle Region | Deep or superficial |
|---|---|---|
| C5 | Suprascapular region | Superficial and deep pain |
| C6 | Suprascapular to posterior deltoid region | Deep pain |
| C7 | Interscapular region | Deep pain |
| C8 | Interscapular and scapular regions | Superficial and deep pain |
Slipman and colleagues coined the term dynatomal pain to describe radicular pain patterns. They purposefully stimulated the nerve roots of patients with cervical radicular syndromes and diligently recorded the pain patterns (figure 3). They found that while there was overlap with dermatomes, symptoms frequently were perceived outside of dermatomal regions.
- Pain in the lateral or posterior upper arm is most likely to be C7 radiculopathy, although C6 can also present with lateral limb posterior arm pain.
- Pain or paraesthesia in lateral forearm is typically C6 or C7 (most likely C7), NOT C5 C8.
- Pain or paraesthesia in medial or posterior forearm C7 or C8 (most likely C7), NOT C5 C6
- Forearm pain or paraesthesia is most likely C7[4]
Neurological Examination
Patients with cervical radicular pain often have a concomitant radiculopathy and so warrant a neurological examination. The neurological examination is used to determine the severity of the condition, identify signs of myelopathy, and potentially determine the affected segmental level.
Cervical radiculopathy is typically characterised by negative objective signs: sensory loss, motor loss, or impaired reflexes, which occur in a segmental distribution. It may be possible to determine the affected level based on the neurological examination.[7]
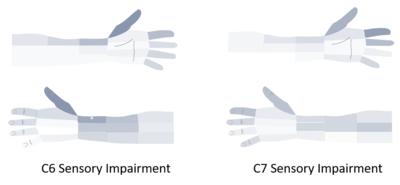
Sensory loss in surgically proven disc prolapse was present in 25% in one study (method of exam not defined)[7], and and 85% in another (pin prick).[5] The sensory loss occurs in the upper limbs, and classically has been described to be dermatomal in distribution.[1] The validity of this statement is questionable, one study found that C6 and C7 could not be differentiated based on dermatomes alone.[6]
The reliability of sensory loss has a Kappa score of 0.45-0.64.
If a patient only has sensory signs then the weight of the evidence suggests that the segmental level can't be determined with any level of accuracy. (See also Dermatomes).
Paraesthesias are present with or without pain in 90% of surgically proven radiculopathy due to disc prolapse.[7] None of the patterns of paraesthesias are pathognomonic. 45% of patients are unable to localise the paraesthesias with diffuse and/or non-dermatomal symptoms.[5] Some of these patients may have combined C6 and C7 radiculopathy further complicating matters.
The classic distribution of paraesthesias is as follows: [7]
- C5: Generally no hand paraesthesias, however the lack of hand paraesthesias can also occur with C6 and C7.
- C6: Thumb or index finger is C6. However C7 is also possible.
- C7: Middle finger is generally C7 with or without the thumb, index, and middle fingers. Index finger alone is generally C7.
- C8: Ring, little finger +/- the middle finger is generally C8. However C7 is also possible.
Weakness can be subjective or objective and occurs in a myotomal pattern. In patients with surgically proven radiculopathy, in one study subjective weakness was present in 34% and objective weakness in 75%,[7] while another study found objective weakness in 68%.[5] Weakness of the biceps is relatively specific for C6, and weakness of the triceps is relatively specific for C7.
The myotomal pattern is very different to the dermatomal pattern. Because of the myotomes also supply proximal shoulder girdle muscles this can be used to differentiate between a proximal lesion (spinal nerve or root) versus a lesion in a peripheral nerve (radial, ulnar, median, etc). A peripheral nerve lesion is not going to cause proximal motor weakness. So patients with cervical motor radiculopathy will tend to have scapular winging in addition to distal weakness.
Hyporeflexia can occur with lateral protrusions, while hyperreflexia can occur with medial protrusions. Reflex loss is present in approximately three quarters of patients with surgically proven radiculopathy.[7] Reflex loss can aid in distinguishing the spinal level.. (See also Reflex Testing).
- A loss of biceps or brachioradialis reflex has a positive likelihood ratio of 14.2 for C6 radiculopathy (but can also occur in C5),
- A loss of triceps reflex has a positive likelihood ratio of 3 for a C7 radiculopathy (but can also occur in C8).[8]
Spurling's test (compression test) is a special test used to reproduce the patients radicular pain (see video). It has good reliability with Kappa score of 0.4-0.77, and good validity if a positive test is taken as the reproduction of the arm pain not only the neck pain. It is highly specific but has poor sensitivity and so it isn't useful as a screening test. Many patients with significant and symptomatic radiological changes do not have a positive compression test.
Myelopathy is a rare condition that can occur with a central disc protrusion. Symptoms and signs of myelopathy occur in the upper limbs, trunk, and lower limbs. The examination is used to determine whether long tract signs are present such as hyperreflexia, spasticity, and a positive Hoffman's sign.
Red Flags
Serious causes of radiculopathy are rare.
- Spinal infection – fever – history of risk factor (body penetration).
- Metastatic disease – history of cancer
- Primary tumours of spinal nerves – may present with radicular pain, but normally profound sensory loss
- Arteritis – fever and malaise (patient sicker than disc protrusion)
- Sarcoidosis – profound sensory and motor loss
- Apical tumours of the lung (Pancoast tumour) – involvement of C8 or T1 spinal nerves
- Intracranial tumour – no valid alerting features if presenting features restricted to neck and upper limb – rapid progression of symptoms only feature
Differential Diagnosis
- Myelopathy: symptoms and signs of long-tract impairment affecting lower limbs and trunk. Patients may present with signs only in the upper limbs. There is the absence of lower motor neurone signs
- Spinal cord lesion
- Multiple sclerosis
- Thoracic outlet Syndrome
- Pancoast Syndrome
- Peripheral Neuropathy : Nerve conduction studies discriminate here, in radiculopathy they are normal, in peripheral neuropathy they are abnormal
- Brachial Neuritis: ill-defined condition, not recognised in neurology
- Stinger: In sportspeople, ‘traction injury to the upper trunk of the brachial plexus. Need to exclude C6 radiculopathy
Investigations
Imaging
Plain films are routinely unhelpful diagnostically as a sole diagnostic test.
Previously myelography and CT were used but this has been replaced by MRI due to its technical superiority and better safety profile. MRI is slightly inferior for detection of bony impingement of nerve roots but this can be aided by also doing plain radiographs. Also newer MRI small slice sequence techniques can be used which are much better at showing bone.
Electrodiagnostic Studies
These are only potentially helpful if clinically a peripheral neuropathy is suspected.
Prognosis
The prognosis is generally good, although not as good as neck pain alone. One study found that recurrences were common at 31.7%, and 90.5% had minimal or no pain at a mean follow up of 5.9 years. A systematic review found that most patients improve within six months. Complete improvement took two to three years and was achieved by 83% of people. This recovery has radiographic correlation as half of cervical disc herniations decrease within the first six months, and 75% decrease by more than 50% within two years. Risk factors for poor outcome is an ongoing worker's compensation claim.[9]
Studies using CT and MRI over 1-30 months show cervical disc protrusions decrease as a rule
Treatment
Conservative
Conservative therapy includes measures such as oral medication, physiotherapy, traction, collar, bed rest, exercise, and TENS. Much of the comparative research on conservative therapy is quite old (?external validity), all of it showing no benefit for any particular conservative passive intervention, and that conservative therapy is effectively equal to sham therapy. A 1966 study found no difference between traction, sham traction, collar, heat, and placebo tablets.[10] A 1970 study found no difference between exercise, traction, and no treatment. A 1990 study found no clinically important difference between traction and placebo traction.[11]
Generally patients with cervical radicular pain should be offered some form of therapy, because no treatment results in a greater proportion of patients feeling that they haven't improved. However no specific therapy can be recommended as being superior to one another.
Injections
This refers to transforaminal or interlaminar epidural corticosteroid injections. The standard preferred technique now is transforaminal. This has been evaluated in multiple different trials. The Pain Physician Epidural Guidelines found that there is level I evidence for cervical interlaminar epidural injections with strong recommendation for long-term effectiveness.[12]
Surgery
There is only one randomised controlled trial using an active control rather than sham control. The findings were some improvement at 3-4 months over conservative therapy, but none at 12 months. Only 8% complete relief, 19% improved, 42% unchanged and 31% worse.[13] Surgery might be considered for chronic symptoms but it shouldn't be promoted as a cure for the majority of cases.
See Also
- Lumbar Radicular Pain
- Radicular Pain and Radiculopathy
- Neuropathic Pain
- Acute Low Back Pain
- Chronic Low Back Pain
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Bogduk. The anatomy and pathophysiology of neck pain. Physical medicine and rehabilitation clinics of North America 2011. 22:367-82, vii. PMID: 21824580. DOI.
- ↑ Manchikanti L, et al. Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines. Pain Physician. 2021 Jan;24(S1):S27-S208. PMID: 33492918.
- ↑ 3.0 3.1 3.2 Mizutamari et al.. Corresponding scapular pain with the nerve root involved in cervical radiculopathy. Journal of orthopaedic surgery (Hong Kong) 2010. 18:356-60. PMID: 21187551. DOI.
- ↑ 4.0 4.1 Slipman CW, Plastaras CT, Palmitier RA, Huston CW, Sterenfeld EB. Symptom provocation of fluoroscopically guided cervical nerve root stimulation. Are dynatomal maps identical to dermatomal maps? Spine (Phila Pa 1976). 1998 Oct 15;23(20):2235-42. doi: 10.1097/00007632-199810150-00019. PMID: 9802168.
- ↑ 5.0 5.1 5.2 5.3 5.4 Henderson CM, Hennessy RG, Shuey HM Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983 Nov;13(5):504-12. doi: 10.1227/00006123-198311000-00004. PMID: 6316196.
- ↑ 6.0 6.1 Rainville et al.. Exploration of sensory impairments associated with C6 and C7 radiculopathies. The spine journal : official journal of the North American Spine Society 2016. 16:49-54. PMID: 26253986. DOI.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 YOSS RE, CORBIN KB, MACCARTY CS, LOVE JG. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology. 1957 Oct;7(10):673-83. doi: 10.1212/wnl.7.10.673. PMID: 13477342.
- ↑ McGee, Steven R. Evidence-based physical diagnosis. Philadelphia, PA: Elsevier, 2018.
- ↑ Cohen & Hooten. Advances in the diagnosis and management of neck pain. BMJ (Clinical research ed.) 2017. 358:j3221. PMID: 28807894. DOI.
- ↑ Pain in the neck and arm: a multicentre trial of the effects of physiotherapy, arranged by the British Association of Physical Medicine. Br Med J. 1966 Jan 29;1(5482):253-8. doi: 10.1136/bmj.1.5482.253. PMID: 5322503; PMCID: PMC1843524.
- ↑ Goldie I, Landquist A. Evaluation of the effects of different forms of physiotherapy in cervical pain. Scand J Rehabil Med. 1970;2(2):117-21. PMID: 5523822.
- ↑ Manchikanti L, et al. Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines. Pain Physician. 2021 Jan;24(S1):S27-S208. PMID: 33492918.
- ↑ Peolsson A, Öberg B, Wibault J, Dedering Å, Zsigmond P, Bernfort L, Kammerlind AS, Persson LC, Löfgren H. Outcome of physiotherapy after surgery for cervical disc disease: a prospective randomised multi-centre trial. BMC Musculoskelet Disord. 2014 Feb 6;15:34. doi: 10.1186/1471-2474-15-34. PMID: 24502414; PMCID: PMC3923245.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


