Cervicogenic Headache
Cervicogenic headache is defined as pain that is perceived in the head that actually arises from the cervical region, and is a form of cervical referred pain. It is one of the few common headache disorders that can be diagnosed objectively. It is treated by four main groups of health professionals each with different views: neurologists, headache specialists, pain medicine, and manual therapists.
Mechanism
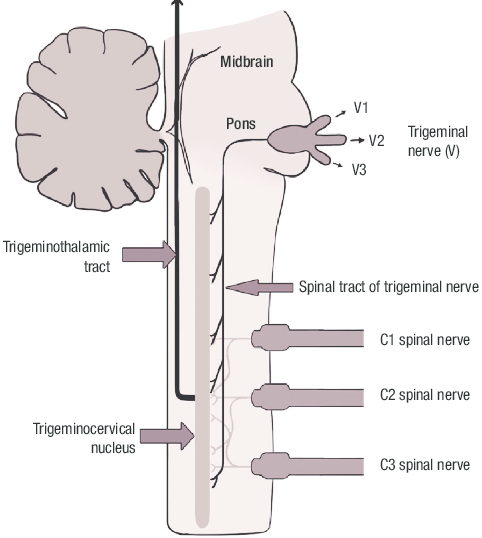
There are sensory axons in the C1, C2, and C2 spinal nerves that converge on dorsal horn neurons that also receive trigeminal afferents. These trigeminal afferents are mostly from the ophthalmic division. The convergence allows pain mediated in the C1, C2, or C3 nerves to be perceived in regions innervated by the trigeminal nerve (cervical - trigeminal referral). Can also have cervical - cervical referred pain. In those with clinically suspected cervicogenic headache, the source can be found through controlled blocks 75% of the time.[1]
Aetiology
The origin of the pain in cervicogenic headache can be
- Nociceptive - irritation of nerve endings in damaged or diseased structures
- Neuropathic - intrinsic disorder of a peripheral nerve
- Central - disturbance of pain pathways within the central nervous system.
| C1 Nerve Root | C2 Nerve Root | C3 Nerve Root | C4 Nerve Root | |
|---|---|---|---|---|
| Joints | Median C1-2 C0-C1 |
Lateral C1-2 joint (7%)[1] | C2-3 ZA joint (62%)[1] C2-3 disc |
C3/4 ZA joint (6%)[1] |
| Ligaments | Transverse C1-2 Alar |
|||
| Muscles | Prevertebral Sternocleidomastoid Trapezius Suboccipital |
Semispinalis Splenius |
Multifidus Semispinalis |
|
| Dura | Upper spinal cord Posterior cranial fossa |
|||
| Arteries | Vertebral Internal carotid |
Any structure that is innervated by the C1-C3 spinal nerves could be a potential source of headache. It is important to remember that the dura mater, vessels of the posterior cranial fossa, and common carotid arteries are also innervated by cervical nerves, and conditions affecting these structures are therefore potential sources. Likewise the common carotid artery can be considered a cervical structure. There is less evidence for structures below C3 being sources of cervicogenic headache.
Causes of cervicogenic headache classified by prevalence and validity.
- Detectable but rare
- Aneurysms - vertebral and internal carotid artery
- Tumours and infection of the posterior cranial fossa
- Neck tongue syndrome
- C2 neuralgia
- Common
- Uncommon
- Putative
- Osteoarthrosis of upper cervical spine joints (Median C1-2 joint and C0-C1 joints).
- Refuted
- Occipital neuralgia
- Barré–Lieou syndrome, or migraine cervale - dated entity, was thought to be due to irritation of the vertebral nerve, which causes spasm of the vertebral artery, but this has been disproven.
- Trigger points - not confirmed by formal studies.
Distinctions
The following first two conditions involve a cervical nerve - namely C2 - and are technically a form of cervicogenic headache, but have unique features and pathology. The third condition below is a refuted diagnosis.
Neck-tongue syndrome: sudden onset of occipital headache with rotation of the head, associated with numbness of the ipsilateral half of the tongue. Excessive rotation leads to subluxation of the atlanto-axial joint leading to occipital pain. The C2 ventral ramus sits behind the joint and is stretched. The proprioceptive afferents from the tongue pass from the ansa hypoglossi into the C2 ventral ramus and are compressed.
C2 neuralgia: The pain is paroxysmal and lancinating in the occiput and associated with lacrimation and ciliary injection. There is also often an associated background of dull occipital pain with dull referral to the temporal, frontal, and orbital regions. The C2 nerve runs behind the lateral atlanto-axial joint and sits on its capsule. The condition is caused by C2 spinal nerve irritation by post-traumatic or post-inflammatory atlanto-axial periarticular fibrosis, nerve tumours, meningiomas, or vascular malformations that compress the C2 dorsal root ganglion. The diagnosis is confirmed with selective C2 spinal nerve block.
Occipital neuralgia: This entity does not have validity and is a dated diagnosis that comes from a time when neurologists and neurosurgeons didn't appreciate the concept of somatic referred pain. There is no proven pathology nor method of diagnosis or treatment. Lancinating pain in the occipital area is more likely to be C2 neuralgia, otherwise if the pain is aching it is more likely to be somatic referred pain from an upper cervical joint.
Clinical Assessment
History
The pain of cervicogenic headache is dull and aching and can be perceived in the occipital, parietal, frontal, or orbital regions of the head; or in a combination of these areas. Getsoian et al used diagnostic blocks of C2-3 and C3-4 as a gold standard to evaluate clinical assessment against (C0-1 and C1-2 not blocked due to increased risk). They found that there are no major distinguishing characteristics on history between cervicogenic headache (positive diagnostic blocks) and non-responders to blocks. Responders more frequently have headache onset related to trauma and neck pain (50% vs 14.3%), and symptoms are more often brought on by pressure to the back of the head or neck (100% vs 43%). Non-responders more often have pain that changes sides (57% vs 20%) and more often have premonitory symptoms (85% vs 50%).[1]
Examination
Getsoian et al found that cervical dysfunction cannot be defined based on any one single examination sign such as isolated tenderness or isolated reduced cervical extension. They found that dysfunction was characterised by, at least, the simultaneous presentation of reduced cervical extension, painful upper cervical joint dysfunction (segmental restriction plus pain), and impaired muscle function (craniocervical flexion test). They assessed cervical extension, craniocervical flexion test, and symptomatic joint dysfunction (segmental restriction plus pain). The C1-2 flexion rotation test was also used to assess for C1-2 cervicogenic headache because they did not do diagnostic blocks at this level. They found that greater flexion-rotation test values (i.e. less likely to have C1-2 dysfunction) was associated with a greater chance of relief with C2-3 and C3-4 blocks.[1]
In effect, the evidence thus far for useful examination features
- C1/2 - Reduced flexion-rotation test
- C2/3 and C3/4 - Simultaneous reduced cervical extension, segmental restriction plus pain, and reduced craniocervical flexion test values.
Diagnosis
The ICHD-3 criteria (below) are problematic because the clinical tests lack validity, and most lack reliability. Controlled diagnostic blocks are the preferred means of confirming the diagnosis. In the absence of controlled blocks, Bogduk suggests that the modifiers possible and probable can be used.
Definitive: Positive controlled medial branch blocks. Or imaging evidence in the case of rare and serious causes such as tumours, aneurysms, and infections.
Probable: pain plus three of:
- Pain triggered by neck movements, sustained awkward posture, or by external pressure on the posterior neck or occiput
- Reduced range of motion of the neck
- Ipsilateral neck, shoulder or arm pain
- Recent history of neck trauma.
Possible: Unilateral plus pain that appears to start in the neck
ICHD-3 Diagnostic criteria (2018)[2]
A. Any headache fulfilling criterion C
B. Clinical and/or imaging evidence[Notes 1] of a disorder or lesion within the cervical spine or soft tissues of the neck, known to be able to cause headache[Notes 2][Notes 3]
C. Evidence of causation demonstrated by at least two of the following:
- 1. headache has developed in temporal relation to the onset of the cervical disorder or appearance of the lesion
- 2. headache has significantly improved or resolved in parallel with improvement in or resolution of the cervical disorder or lesion
- 3. cervical range of motion is reduced and headache is made significantly worse by provocative manœuvres
- 4. headache is abolished following diagnostic blockade of a cervical structure or its nerve supply[Notes 4]
D. Not better accounted for by another ICHD-3 diagnosis.[Notes 5][Notes 6][Notes 7]
Notes
- ↑ ICDH Note: Imaging findings in the upper cervical spine are common in patients without headache; they are suggestive but not firm evidence of causation.
- ↑ ICDH Note: Tumours, fractures, infections and rheumatoid arthritis of the upper cervical spine have not been formally validated as causes of headache, but are accepted to fulfil criterion B in individual cases. Cervical spondylosis and osteochondritis may or may not be valid causes fulfilling criterion B, again depending on the individual case.
- ↑ Clinical sign must be reliable and valid, but none is established at present. Neck pain, focal neck tenderness, history of neck trauma, mechanical exacerbation of pain, unilaterality, coexisting shoulder pain, reduced range of motion in the neck, nausea, vomiting, photophobia, etc are not unique to cervicogenic headache. Maybe features of cervicogenic headache, but they do not define relationship between the disorder and the source of the headache.
Editor's note: Not technically true that no valid clinical sign see Clinical Assessment. - ↑ Abolition of headache means VAS 0/100. But >90% reduction in pain is accepted, or pain <5/100 on VAS.
- ↑ ICDH Note: When cervical myofascial pain is the cause, the headache should probably be coded under 2. Tension-type headache; however, awaiting further evidence, an alternative diagnosis of A11.2.5 Headache attributed to cervical myofascial pain is in the Appendix.
- ↑ ICDH Note: Headache caused by upper cervical radiculopathy has been postulated and, considering the now well-understood convergence between upper cervical and trigeminal nociception, this is a logical cause of headache. Pending further evidence, this diagnosis is in the Appendix as A11.2.4 Headache attributed to upper cervical radiculopathy.
- ↑ ICDH Note: Features that tend to distinguish 11.2.1 Cervicogenic headache from 1. Migraine and 2. Tension-type headache include side-locked pain, provocation of typical headache by digital pressure on neck muscles and by head movement, and posterior-to-anterior radiation of pain. However, while these may be features of 11.2.1 Cervicogenic headache, they are not unique to it and they do not necessarily define causal relationships. Migrainous features such as nausea, vomiting and photo/phonophobia may be present with 11.2.1 Cervicogenic headache, although to a generally lesser degree than in 1. Migraine, and may differentiate some cases from 2. Tension-type headache.
C2 neuralgia: Diagnosed by complete relief of pain with selective local anaesthetic blockade of the suspected nerve root.
Treatment
An open access review of interventional treatment strategies was published by Goyal and colleagues in 2022.[3]
Rare causes of cervicogenic headache: Generally have specific treatments, for example aneurysm clipping, tumour excision, and atlanto-axial fusion for instability.
Probable cervicogenic headache: manual therapy (mobilisations not manipulation), exercises, or a combination, are all similarly effective.
Third occipital nerve headache:
- Intra-articular C2-3 zygapophyseal joint corticosteroid injection
- Radiofrequency neurotomy in those who have obtained complete relief of their headache following controlled diagnostic third occipital nerve blocks. This has level 2 evidence.[4]
C2-3 intervertebral disc origin: Arthrodesis is a treatment option if discography is positive.
Lateral atlanto-axial joint origin: There is no proven treatment. A peri- or intra-articular corticosteroid injection could be considered but this is experimental. Arthrodesis is another option.
C2 neuralgia: surgery appears to be the only definitive treatment
Resources
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Govind, Jayantilal; Bogduk, Nikolai (2022-05-30). "Sources of Cervicogenic Headache Among the Upper Cervical Synovial Joints". Pain Medicine (Malden, Mass.). 23 (6): 1059–1065. doi:10.1093/pm/pnaa469. ISSN 1526-4637. PMID 33484154.
- ↑ ICHD-3. Full Text
- ↑ Goyal S, Kumar A, Mishra P, Goyal D. Efficacy of interventional treatment strategies for managing patients with cervicogenic headache: a systematic review. Korean J Anesthesiol. 2022 Feb;75(1):12-24. doi: 10.4097/kja.21328. Epub 2021 Oct 1. PMID: 34592806; PMCID: PMC8831436.
- ↑ Suer, Michael; Wahezi, Sayed Emal; Abd-Elsayed, Alaa; Sehgal, Nalini (2022-05). "Cervical Facet Joint Pain and Cervicogenic Headache Treated With Radiofrequency Ablation: A Systematic Review". Pain Physician. 25 (3): 251–263. ISSN 2150-1149. PMID 35652765. Check date values in:
|date=(help)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,