Chronic Inflammatory Demyelinating Polyneuropathy
| Chronic Inflammatory Demyelinating Polyneuropathy | |
|---|---|
| Epidemiology | 0.7-1.6 cases per 100,000 per year, median age 58 |
| Pathophysiology | Autoimmune demyelination of large peripheral nerve fibres |
| Classification | Typical and atypical phenotypes |
| Risk Factors | Diabetes, anti TNF-alpha medication |
| History | Proximal and distal weakness, paraesthesias, numbness, fatigue, difficulty with fine motor control |
| Examination | Weakness, areflexia without wasting, joint position and vibration sense loss, foot drop, sensory ataxia |
| Diagnosis | Diagnostic criteria |
| Tests | Laboratory tests, electrophysiology studies |
| Treatment | Immunoglobulin and plasma exchange |
See Ryan et al for an open access review.[1] CIDP should be considered in any patient with progressive symmetrical or asymmetrical polyradiculopathy that is relapsing and remitting or that progresses for longer than 2 months.[1]
| The common manifestations of CIDP are: |
|---|
| Gradually worsening paraesthesia and numbness |
| Muscle weakness in legs and arms |
| Areflexia without wasting |
| Preferential loss of joint position or vibration sense |
| Foot drop and difficulty getting out of the chair |
| Difficulty with fine motor control |
| Sensory ataxia |
| Fatigue |
Notably motor and proprioceptive deficits predominate over pain and autonomic symptoms. Severe pain occurs in 13-17% of patients.
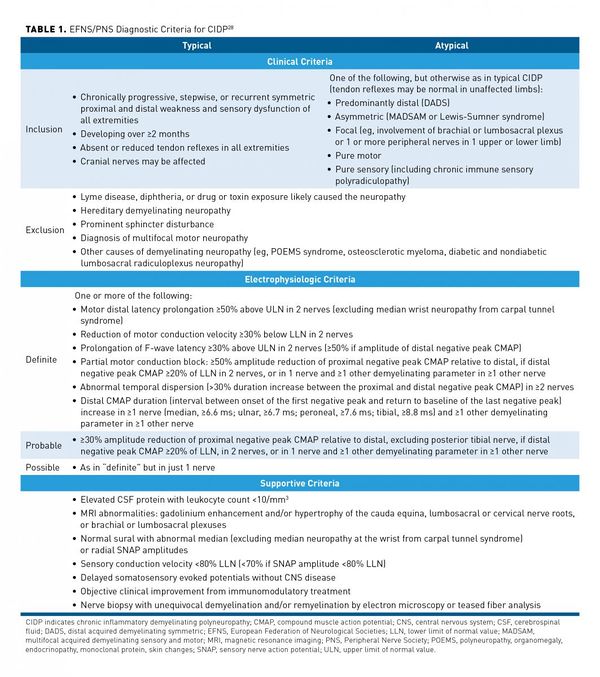
The typical form of CIDP occurs in 50% of patients and manifests as both proximal and distal weakness. Atypical forms include a predominant distal distribution (distal acquired demyelinating symmetric - DADS), an asymmetric distribution (multifocal acquired demyelinating sensory and motor neuropathy - MADSAM), pure sensory, pure motor, and extremely rarely focal CIDP.
There is a temporal continuum between the demyelinating form of Guillain-Barre on the one end (acute inflammatory demyelinating polyneuropathy - AIDP), and CIDP in those with AIDP that don't recover.
There are many diagnostic criteria. See below for an example from the European Federation of Neurological Societies and the Peripheral Nerve Society. The criteria are highly specific (96.2%) but not sensitive (81.3%). Clinical history, physical examination, Electrophysiology studies, and laboratory tests form part of the criteria. Misdiagnosis is common, with misinterpretation of nerve conduction studies being a common reason.
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,