Chronic Low Back Pain
Chronic low back pain is a common cause of persistent suffering and disability for the affected individual, but also has significant effects on those around them. The biomedical assessment involves determining whether they have the IASP definition of low back pain, whether it is indeed chronic, ascertaining whether they have referred pain and whether it is somatic referred pain or radicular pain, and identifying "red flag" conditions. A decision is then made about whether to go down an investigative pathway to determine the source and cause of the pain. Treatment approaches include monotherapies (e.g. physiotherapy, surgery, medication), multi-disciplinary treatments, and reductionist treatments if a precision diagnosis is made and a relevant treatment is available, efficacious, and acceptable to the patient (e.g. medial branch radiofrequency neurotomy for confirmed facet joint pain).
Definitions
- Main article: Low Back Pain Definitions
Topography
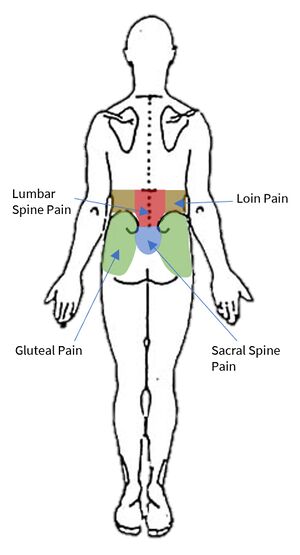
Starting with the wrong definition of low back pain can lead to the wrong diagnosis, and so it is important to be clear here. Low back pain is not loin pain, nor is it gluteal pain. The IASP taxonomy categorises low back pain into lumbar spinal pain and sacral spinal pain. There is also an overlapping definition called lumbosacral pain. These three categories constitute the colloquial term "low back pain."
Lumbar spinal pain is pain in a region bounded superiorly by an imaginary transverse line through the tip T12, inferiorly by an imaginary transverse line through the tip of S1, and laterally by vertical lines tangential to the lateral margins of the erector spinae muscles.
Sacral Spinal Pain is pain in a region bounded superiorly by an imaginary transverse line through the tip of S1, inferiorly by an imaginary transverse line through the posterior sacrococcygeal joints, and laterally by imaginary lines passing through the posterior superior and posterior inferior iliac spines."
Lumbosacral Pain is pain perceived as arising from a region encompassing or centred over the lower third of the lumbar region as described above and the upper third of the sacral region as described above.
Acuity
Chronic pain is pain present for longer than 3 months (91 days). One pragmatic approach is to include in the definition of chronic those patients with acute low back pain who are not improving when it may not be sensible to wait until the 91 day mark, say at two months. However if they have had pain for more than two months and not had evidence based management for acute low back pain then they should have that first. Indeed, following the acute approach may still be appropriate for some patients who have had pain for longer than 3 months.
Referred Pain
- Main article: Low_Back_Pain_Definitions#Referred_Pain
Referred pain is "pain perceived as arising or occurring in a region of the body innervated by nerves or branches of nerves other than those that innervate the actual source of pain"
Visceral referred pain is referred pain where the source lies in an organ or blood vessel of the body. With low back pain, the uterus and abdominal aorta are important considerations. Other viscera with higher segmental supply may cause back pain such as pancreatitis, but this may be due to irritation of the posterior abdominal wall, in which case the pain is not truly referred in nature.
Somatic referred pain is referred pain where the source originates in a tissue or structure of the body wall or limbs. A number of structures in the lumbar spine are capable of nociception including the lumbar zygapophysial joints, intervertebral discs, sacroiliac joints, and more.
Radicular pain is a subset of neuropathic pain, and refers to pain that is evoked with stimulation of the nerve roots or dorsal root ganglion of a spinal nerve. In radicular pain, the pain is felt in the peripheral innervation of the affected nerve.
Somatic referred pain and radicular pain can usually be differentiated based on the quality and spread of the pain, see the assessment section below.
Aetiology
- Main article: Causes and Sources of Chronic Low Back Pain
Various structures in the low back are capable of nociception as determined through noxious stimulation, including the muscles, interspinous ligaments, zygapophysial joints, sacroiliac joints, and the intervertebral discs which are the most sensitive. These constitute possible sources of pain.[2]
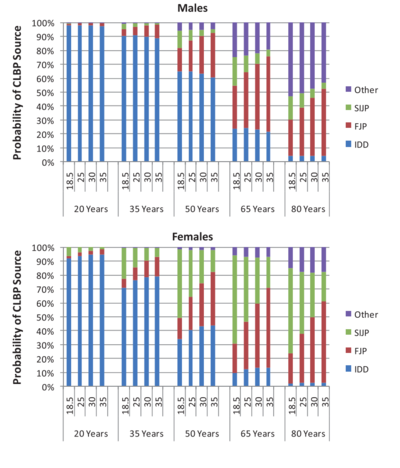
The lumbar intervertebral discs and lumbar zygapophysial joints have the most evidence as established sources (i.e implicated structure) of pain. The sacroiliac joint has the next best evidence. In terms of causes (i.e the pathology is known) only discogenic pain has high level evidence with respect to internal disc disruption. The prevalence of the various sources of pain depends on age, BMI, and gender[1] Overall around 40% have disc pain, around 30% have facet joint pain, and around 20% have sacroiliac joint pain.[3] The common aphorism that "most chronic low back pain is non-specific" is 30 years out of date and demonstrably false.
Epidemiology
- Main article: Epidemiology of Low Back Pain
The prevalence of chronic low back pain was estimated to be 9.1% in the 2013/14 New Zealand Health Survey. The prevalence increases with age, reaching 13.6% in the 60+ group. It also increases with social deprivation. It was estimated that around 7% had an active ACC claim lasting more than 6 months.
The New Zealand Burden of Disease Study (NZBDS) estimated that "back disorders" (included various regions) were associated with 27,112 DALYs in the New Zealand population in 2006 (2.8% of all DALYs) and ranked seventh. In the United Kingdom, low back pain was identified as the most common cause of disability in young adults.
Assessment
The assessment of chronic low back pain has some slight modifications to that of acute low back pain. History is still important, while physical examination still has major limitations. Imaging however now plays a greater role. The doctor must take care to avoid missing any serious causes of pain, formulate a diagnosis, instigate an investigation and treatment plan, and identify and manage any psychosocial barriers to recovery. Unlike with acute low back pain, a precise diagnosis is often possible for chronic low back pain. A decision is made whether to pursue a definitive diagnosis to enable specific targeted treatment, or apply general treatments that don't require precise source identification.
Pain History
- See also: Acute Low Back Pain#Pain History, Medical History
The age of the patient is of vital importance. This is because the potential causes are dependent on age, as well as certain malignancies.
The site of pain helps to determine the taxonomy, whether they have lumbar spine pain, loin pain, gluteal pain, or abdominal pain, each of which have a different assessment and management. Abdominal pain takes priority over low back pain.
For sacroiliac joint and presumably also sacroiliac ligament pain, the pain does not tend to project above the L5 level. So if the pain is restricted below L5, then the sacroiliac joints are more likely.[4][5] Conversely, if the pain is above L5 then the intervertebral discs or zygapophysial joints are more likely. In patients with bilateral pain when considering between zygapophysial joint pain and sacroiliac joint pain, it is more likely for bilateral zygapophysial joints to be injured than bilateral sacroiliac joints.[6]
The duration of illness establishes whether they have chronic pain as it is defined, and make some sort of assessment as to the likelihood of red flag conditions. The idea being that pain present for a long time without deterioration may suggest a low risk of red flags. However certain infections and tumours can develop very slowly.
The distribution of pain its quality helps distinguish between somatic referred and radicular pain. (see article on referred pain). These two entities are commonly confused, so much so that the reliability of prevalence studies on radicular pain has been called into question.[7] Somatic referred pain is thought to be much more common than radicular pain. Patients can have combined states (e.g. radicular pain from nerve root irritation, somatic referred pain from dural sleeve irritation, and somatic back pain from internal disc disruption) which complicates assessment. In this setting each underlying feature may have separate treatment, for example discectomy only works for radicular pain, not for back pain.[8]
| Somatic Referred | Radicular | |
|---|---|---|
| Pain quality | Dull, deep ache, or pressure-like, perhaps like an expanding pressure | Shooting, lancinating, or electric-shocks |
| Relation to back pain | Referred pain is always concurrent with back pain. If the back pain ceases then so does the referred pain. If the back pain flares then so does the leg pain intensity and spatial spread. | Not always concurrent with back pain. |
| Distribution | Anywhere in the lower limb, fixed in location, commonly in the buttock or proximal thigh. Spread of pain distal to the knee can occur when severe even to the foot, and it can skip regions such as the thigh. It can feel like an expanding pressure into the lower limb, but remains in location once established without traveling. It can wax and wane, but does so in the same location. | Entire length of lower limb, but below knee > above knee. In mild cases the pain may be restricted proximally. |
| Pattern | Felt in a wide area, with difficult to perceive boundaries, often demonstrated with an open hand rather than pointing finger. The centres in contrast can be confidently indicated. | Travels along a narrow band no more than 5-8 cm wide in a quasi-segmental fashion but not related to dermatomes (dynatomal). |
| Depth | Deep only, lacks any cutaneous quality | Deep as well as superficial |
| Neurological signs | Not characteristic | Favours radicular pain, but not required. |
| Neuroanatomical basis | Discharge of the peripheral nerve endings of Aδ and C fibres from the lower back converge onto second order neurons in the dorsal horn that also receive input from from the lower limb, and so the frontal lobe has no way of knowing where the pain came from. | Heterotopic discharge of Aδ, Aβ, and C fibres through stimulation of a dorsal root or dorsal root ganglion of a spinal nerve, typically in the presence of inflammation, with pain being felt in the peripheral innervation of the affected nerve |
The intensity of pain can be recoded using the VAS or NRS scale. For those individuals where pain fluctuates, record the average intensity during activity, and the worst pain recently. Pain intensity is the single most significant patient factor for decision about seeking medical care, and so the pain is likely to be significant enough to them regardless of the actual figure given. Sometimes patients may indicate very high pain scores such as "12/10" and this may reflect suffering and psychological distress. The intensity of pain can be useful for recording a baseline, monitoring progress, and judging the effectiveness of treatment.
There is no association between pain intensity and how likely it is that the cause of the pain is due to a serious condition.
The periodicity refers to whether the pain is constant or intermittent. Most patients with chronic low back pain have constant pain. Intermittent can mean either the pain is constantly there but fluctuates in intensity, or can mean that it is present in between pain-free episodes. The exact meaning should therefore be clarified.
If the pain is indeed intermittent - it occurs in between pain-free episodes - then determine the periodicity, time of onset, and mode of onset of the pain. Periodicity means the frequency of episodes, and their duration. Time of onset is relevant in identifying the morning stiffness of inflammatory back pain (ankylosing spondylitis). Mode of onset is whether it is gradual or sudden in onset. Because chronic low back pain is usually constant, these parameters are not typically helpful.
Precipitating factors (what triggers episodes of pain), aggravating factors (what makes the pain worse), and relieving factors (what relieves the pain) are not helpful diagnostically, but paint a picture of the disability experienced by the patient.
Associated features are particularly relevant to red flag conditions. They are listed in the red flags section below, and discussed in more detail in the acute low back pain article.
Circumstances of onset is what they were doing when the pain started, and what the pain was like initially. The biomechanics of any particular injury with regards to the forces and posture of the patient at the time may allow a "guess" as to the injured structure.[2] However I am not aware of any literature that has validated circumstances of onset with validated diagnostic techniques.
- Fractures: A fall for instance would raise suspicions for fracture. In the elderly fracture can occur from standing height.
- Internal disc disruption: Compression injuries are the most relevant which can occur with a single event such as a fall onto the buttocks or with repetitive compression loads over a period of time such as with repetitive heaving lifting or pulling. Internal disc disruption occurs gradually however (following endplate fracture), and initially there may only be mild discomfort, with significant pain only developing following the development of fissures, and the onset of chemical and mechanical nociception.
- Zygapophysial joint injury: Sudden severe rotation could indicate a torsional injury to the zygapophysial joints and/or the anulus fibrosus (see Torsion Injuries)
- Sacroiliac joint injury: A fall onto the buttocks or a motor vehicle accident where the lower limb is impacted.
- Spondylolysis: A stress reaction of the pars interarticularis could be considered in sportspeople where there is forceful or repetitive extension and rotation. In other people there is no association.
- Interspinous soft tissue injury: This may occur by lifting in flexion and occasionally in hyperextension. It can also occur with a fall.
In New Zealand there is a perverse incentive to link pain to an injury event because under ACC there is drastically better access to allied health, investigations, and specialist care. Without an ACC claim the patient is relegated to the far more restrictive public health system. Because of this, most patients with back pain end up with an ACC number, and trauma is the "cause" at rates far higher than seen internationally. Many sarcomas for example are diagnosed under an ACC claim. Also often injury events that occurred gradually over time may be recorded as single events, because injuries over time only have a chance of being covered under ACC if they occurred at work (called "gradual process injury")
Widespread Pain
It should be determined whether there is widespread pain, as widespread pain may indicate a more systemic condition such as rheumatological conditions, fibromyalgia, central sensitisation, or controversially some heritable connective tissue disorders. These categories of patients can still nonetheless have the standard causes and sources of chronic low back pain, but the assessment and management is made much more difficult.
Widespread pain should not be confused with somatic referred pain: the latter does not spread cranially. Another common pitfall is assuming that multiple concurrent primary nociceptive drivers can't co-exist. For example symptomatic hip osteoarthritis and lateral elbow tendinopathy are both very common conditions, and may occur simultaneously as separate primary nociceptive conditions through aleotoric processes (See article on uncertainty). A single "unifying diagnosis" of central sensitisation may not apply here. Here we see the opposing aphorisms of Occams razor ("entities should not be multiplied beyond necessity") and Hickams dictum ("patients can have as many diseases as they damn well please"). Each individual affected region should be assessed on its own merit.
In someone with multiple areas of pain, "solving" the low back pain of someone with widespread chronic pain pain may not reduce their overall pain score or improve their overall function. The clinician can end up moving around the body of the patient over years without any significant overall improvement. Some consider such patients to be best served by a multidisciplinary pain clinic, but this is not a hard and fast rule. In those where MDT is not acceptable or suitable, one approach is to address the "worst area" (patient defined) first.
Red Flags
- See also: Acute Low Back Pain#Red Flags
The same red flags in acute low back pain can be used for chronic low back pain. Any red flags that are identified prompts further consideration for a serious conditions, which may include investigation. They are not diagnostic or such conditions, and are not designed to have great positive predictive power. They were developed on the basis of case reports of unusual causes that were overlooked during assessment but could have been identified if the appropriate question was asked.[2]
If there are no positive responses then the likelihood of a serious condition is extremely low. In the presence of neurological features, this complicates the presentation, and investigating this becomes more important than investigating the cause of the back pain, as the investigations are not always the same.
- History of: Trauma, sports injury, fever, night sweats, recent surgery, catheterisation, venipuncture, illicit drug use, weight loss, cancer, occupational exposure, hobby exposure, overseas travel, pain severe worsening or unremitting especially at night
- Cardiovascular: Risk factors
- Respiratory: Cough in a smoker or ex-smoker
- Gentio-urinary: Infection, haematuria, retention, stream problems
- Gynaecological: abnormal uterine bleeding, dysmenorrhoea
- Haematological
- Endocrine: Diabetes, corticosteroids, parathyroid
- Musculoskeletal: pain elsewhere
- Neurologic: symptoms/signs including for cauda equina compression
- Skin: Infection, rashes
- Gastrointestinal: Diarrhoea, inflammatory bowel disease
- Demographic: Aged over 50 years with first episode, especially age over 65 years
Psychosocial Assessment
Much of the same psychosocial assessment principles in acute low back pain apply. Of importance is that diagnoses such as "factitious disorder" and "malingering" have no valid operational criteria for diagnosis, and should not be used. A similar related concept is "secondary gain" and this too has weak scientific support. "Secondary losses" generally outweigh any "secondary gains," and so it does not constitute a diagnosis.[10]
Various questionnaires have been developed to identify psychological features such as fear avoidance, kinesiophobia, catastrophising, depression, and anxiety. Such features can account for some of the disability a patient is experiencing as a result of their pain. Such patients may be pre-occupied with their pain, depressed, and feel unable to do anything about it, and be focused on passive therapies.
Psychological symptoms are generally a consequence of experiencing chronic pain in susceptible individuals, they are not indicative of the reverse i.e. the pain arising from psychosocial distress. In the biopsychosocial model, the biological features are essential to the experience of pain. The maladaptive response to the pain experience would not exist without the pain experience itself. However the doctor should be aware of any related psychosocial issues.[2]
However, patients with high levels of psychological distress tend to respond poorly to conventional biomedical treatment. Identifying high levels of distress may cause pause for the doctor. Further biomedical treatments that are destined to fail can lead to cycles of hope and despair, exacerbating the patients psychological distress.
The social history includes asking about ability to work, financial distress, social supports, relationships, and functioning at home with activities of daily living. It may also include assessing for any substance abuse.
Physical Examination
As for acute low back pain, the physical examination is not able to make a reliable patho-anatomic diagnosis in chronic low back pain due to the lack of pathognomonic signs. However, there are three main reasons for doing a physical examination
- The first reason is that patients expect it, and doing it shows interest and caring.
- The second reason is that if no signs of somatic dysfunction are found in the spine, then this could indicate a serious underlying visceral or vascular condition. However, due to visceral referred pain, patients with visceral pathology can still have somatic segmental dysfunction. Therefore an abdominal and vascular examination is still warranted in those at increased risk.
- The third reason is that the doctor can provide positive reinforcement (e.g. celebrating normal findings) with the view of reducing patient fear.
The lumbar spine exam involves inspection, palpation, and movement testing.
- Inspection: posture standing and sitting (scoliosis, kyphosis, loss of lordosis), dynamic posture (antalgic gait), deformities, scars, puncture marks, swelling. The reliability reported in studies has varied. The validity is unknown.
- Palpation: altered sensitivity (hypoesthesia, hyperesthesia), tenderness and its relationship to bony landmarks, and whether localised or diffuse. The reliability is excellent for tenderness somewhere in the lumbar spine (kappa 1.0), but when the location is specified the agreement is variable. Tenderness over the iliac crest superomedial to the PSIS is good (kappa 0.66), but the validity is unknown.
- Movement testing: active, passive, and accessory movement testing. Active and passive ranges are tested in flexion and extension, side bending, and rotation. Quadrant tested can also be done (e.g. extension with rotation). The reliability is fair to moderate, but the validity is unknown.
The reliability and validity of the physical examination has been studied with regards to the three most common causes of chronic low back pain: internal disc disruption, facet joint pain, and sacroiliac joint pain.
A specialised examination sequence has been developed to detect sacroiliac joint pain (known as the cluster of Laslett)[11] and internal disc disruption (McKenzie assessment method).[12][13] This protocol can't detect zygapophysial joint pain. It also requires special training.[14]
For internal disc disruption, a positive centralisation response under the McKenzie assessment method has a positive LR of 2.4.[15] In a 50 year old male this increases probability from ~60% to ~80%, but in a person over 65 it rises from ~5-20% to ~10-40%.
For facet joint pain there are no diagnostic examination findings. However certain combinations of features may suggest a facet joint origin: age greater than 65; pain relieved by recumbency; and absence of aggravation of pain by coughing, forward flexion, rising from flexion, hyperextension, and extension-rotation. Five or more features has a positive LR of 3.0.[16] In a 50 year old the pre-test probability rises from ~20% to ~40%, and in a person over 65 the pre-test probability rises from ~30% to ~55%.
The "Wadell's inorganic tests" are not appropriate for clinical use as they are neither diagnostic nor predictive. They were designed to identify patients in need of psychosocial assessment, but became abused to identify non-genuine patients. They are not a basis of denying biopsychosocial treatment. Furthermore they don't actually predict failure to return to work.[10]
As for acute low back pain, a neurological examination is only necessary if the patient has indicated neurological symptoms. Any neurological signs indicate a neurological disorder and this should be investigated within its own merits.
Review of Previous Investigations
During the initial assessment there may be previous imaging studies on hand, as well as previous diagnostic or therapeutic procedures. Reviewing these images before formulating a clinical impression can lead the doctor down the wrong path. King and Bogduk suggest the doctor take pause and reflect on two caveats.[2]
The first caveat is that appearances on imaging do not correlate with pain. The doctor can be mislead by irrelevant findings. The second caveat is that the reliability of radiology reports is not perfect. The quality is operator dependent and is subject to human error. It is always recommended that the doctor looks at the imaging themselves.[2] Orthopaedic surgeons do this, and doctors in other specialties would be wise to follow suit.
Another consideration is that very often somatic referred pain is confused as radicular pain, and this leads to confusion when interpreting the report. Imaging is generally helpful in radicular pain and radiculopathy as it can often identify the cause. With somatic referred pain however, imaging is not helpful diagnostically in the majority of cases. Undertaking imaging for somatic referred pain runs the risk of false positive interpretations, as any possible nerve root compression is not relevant in this setting. This can even lead down a path towards unnecessary microdiscectomy and fusion surgery.[8]
With previous diagnostic or therapeutic procedures, King and Bogduk suggest that they may not have been done optimally. For example the response may not have been recorded accurately. If they have had a certain procedure the technique may not have been successful. For example if they have had a previous sacroiliac intra-articular joint block, there may be no proof of intra-articular placement in the form of contrast deposition on a saved image. It can be useful to look through previous images keeping this in mind, or the doctor can ask an interventionalist if they are unsure.[2]
Any previous investigations can otherwise assist with the assessment. Also, repeat investigations may not be needed.
Provisional Diagnosis
After the assessment and review of previous imaging (if available), a provisional diagnosis is made. It is rare to be able to make a definitive diagnosis at this point.[2]
The doctor formulates the provisional diagnosis based on historical features, physical examination, and data from prevalence studies of the three most common causes of chronic low back pain. These are namely discogenic pain (generally internal disc disruption), zygapophysial joint pain, and sacroiliac joint pain (either the joint or ligaments). If a red flag is detected then this becomes the provisional diagnosis.[2]
The provisional diagnosis serves as a hypothesis that can be tested with further investigations. Once a definitive diagnosis is made, targeted treatment may be available.[2]
A definitive diagnosis is not necessary if targeted treatment is not acceptable or suitable. In this case the IASP diagnosis of "Lumbar Spinal Pain of Unknown or Uncertain Origin" can be applied, and general forms of treatment can be offered. "Nonspecific chronic low back pain" is not an IASP diagnosis and should be avoided as the term has a history of being applied to patients in a definitive sense that have not actually had appropriate investigations.[2]
King and Bogduk suggest that if a provisional diagnosis cannot be made, then there should be no attempt at a specific treatment. This is because a specific treatment in the absence of a valid diagnosis does not tend to abolish the pain, but simply exacerbates the hope-despair cycle. If a specific treatment is still desired then they should be referred to a colleague for a second opinion.[2]
Utility of Precision Diagnoses
Whether the cause should be diagnosed, and whether the cause can be cured are two entirely separate questions from whether it can be diagnosed. Bogduk has presented the value of making a biomedical diagnosis as being viewed from three lenses: positive therapeutic value (does making a diagnosis lead to improved outcomes), negative therapeutic value (does making a diagnosis prevent inappropriate treatment), and diagnostic utility (is making a diagnosis helpful in itself without treatment being available).[17]
- Positive therapeutic utility: as per the treatment section of this article, there treatments proven in RCTs to work for facet joint mediated pain, sacroiliac joint pain, and discogenic pain.
- Negative therapeutic utility: Providing a diagnosis may stop a potentially inappropriate intervention. For example, if provocation discography is negative or indeterminate then it may not be appropriate to have spinal fusion.
- Diagnostic utility: Making a diagnosis provides an explanation, and reduces the fear around not knowing what is causing the pain. It also serves to inform treating clinicians that the patient doesn't have primary nociplastic pain, which otherwise may lead to the patient not being taken seriously.
Investigations
There are two possible reasons to refer for investigations: excluding red flag conditions and to test the provisional diagnosis.
For screening for serious or rare causes of chronic low back pain MRI has the best sensitivity and specificity. As well as soft tissue abnormalities, MRI can also detect fractures, and so in principle there is no point in doing plain films or CT if MRI is available.
Some consider failure to improve is a criterion for checking for red flag conditions, and suggest MRI be done. The pick up rate for this single red flag alone is very low, and so usually guidelines do not suggest MRI here.
Imaging
Plain Radiography
- Main article: Lumbar Spine Radiographs
Plain films can detect bone lesions such as myeloma and metastases, but may miss these if early. They also don't detect serious lesions of soft tissues. Therefore x-rays can't fully exclude serious conditions. Furthermore they have a risk of detecting issues such as spondylosis or "degenerative change" that are not causes of pain but might lead to patient misunderstanding and distress. CT has some similar issues however it may detect neurological conditions, but is not available in primary care.
MRI
- Main article: Lumbar Spine MRI
MRI can visualise both bones and soft tissues. It has high sensitivity and specificity, and is safe. It is therefore the best available screening test on face value. Plain films and CT are inferior options. The major limitations are the high cost (around $1500 privately) and the low pick-up rate for serious conditions. Despite widespread availability in New Zealand the cost has not come down, unlike the situation in Australia. ACC and Southern Cross both run a scheme for GP access, but the criteria are very strict. For example low back pain with radicular pain a sensory radiculopathy does not qualify.
Like with plain films, there are many findings on MRI that do not constitute a diagnosis. These include disc bulges and degenerative changes. However high intensity zones and Modic changes (endplate changes) are relevant to chronic low back pain, in that they are indicative of internal disc disruption.
Some authors state these are not valid signs because they also occur in asymptomatic patients. The second statement is true, it is not pathognomonic, but it is more common in symptomatic patients. Many clinical tests in medicine are not pathognomonic (e.g. ANA) but still have utility. In a patient with chronic low back pain where the pre-test probability of discogenic pain is already high, they strongly indicates that the affected disc is the source of the pain. Both findings having positive LRs of around 3. The overall pretest probability of internal disc disruption is ~40%, which gives a post-test probability of ~67%. In a 35 year old, the probability rises from ~80-90% to ~90-95%; In a 50 year old it rises from ~40-65% to ~65-85%.
A further utility of MRI is that if the MRI images of the intervertebral discs are normal then the discs are unlikely to be the source of the pain. In this case other sources of pain should be considered (zygapophysial joints and sacroiliac joints)
High Intensity Zone
High-intensity zones (HIZ) can occur in the innervated posterior anulus of lumbar intervertebral discs. They are seen on T2 weighted images as a bright signal surrounded by dark signal of surrounding fibres. It reflects a circumferential grade IV anular tear, best seen in a sagittal section, but can also correlate with a grade III tear. The brightness should be similar or exceed the brightness of the CSF, it is not just any white spot in the anulus.
The prevalence in patients with chronic low back pain is 20-30%, and they correlate with the disc being painful on provocation discography with a positive LR of greater than 3 (one pooled estimate is 3.8).[17]
Endplate (Modic) Changes
Modic changes or lesions are changes in the spongiosa of the vertebral body above or below a disc with internal disc disruption. Type 1 lesions are dark on T1 and bright on T2 and reflect bone marrow oedema. Type 2 lesions are bright on both T1 and T2 and reflect fatty change that is usually post-inflammatory.
The prevalence amongst individuals with chronic low back pain is around 33%, and they correlate with the disc being painful on provocation discography with a positive LR of around 3 (one pooled estimate is 3.4).[17] They also predict response to basivertebral nerve ablation, and some authors therefore subdivide patients with endplate changes and positive provocation discography as having "vertebrogenic pain".[18]
Electrophysiology
There is no role for nerve conduction studies in the evaluation of chronic low back pain. They should only be considered if peripheral neuropathy is a possibility, but peripheral neuropathy is not in the list of differential diagnoses for chronic low back pain They also do not have any proven validity in distinguishing radicular pain from somatic referred pain.[2]
Physiological Tests
As pain is a sensory experience, imaging studies are only helpful diagnostically if the abnormality has been previously shown to be correlated with pain in prevalence studies. In the absence of such a correlation, or when a definitive diagnosis is required, imaging can't be used to diagnose pain. Physiological tests are the criterion standard for identifying the source of an individuals chronic low back pain. Such physiological tests don't identify the cause of pain, only the source of pain. Imaging is sometimes helpful for identifying the cause of disc pain, but is typically unhelpful for zygapophysial and sacroiliac joint pain.
Disc Stimulation
The gold standard test for internal disc disruption is disc stimulation (also known as provocation discography) to test for pain and post-discography CT to visualise the disruption.
A needle is placed into the nucleus pulposus and it is distended with contrast to a predetermined pressure, all under visualisation with fluoroscopy. The test is positive if the pain is reproduced at pressures of less than 50 psi (preferably less than 15 psi) and stimulation of adjacent control discs (i.e. with separate needles) doesn't reproduce the pain. With the contrast in place, CT imaging shows up any fissures and their grade.[19]
The indications for undergoing disc stimulation is if there is a need to establish a definitive diagnosis if disc targeted therapies are being considered. In New Zealand it is not commonly done due to limited interventional options for discogenic pain available. Note however that in the basivertebral nerve ablation research, discography was not part of the inclusion criteria, Modic change was the key inclusion criteria.[18] For intradiscal biacuplasty, disc stimulation was part of the inclusion criteria.[20]
Medial Branch Blocks
The gold standard diagnostic test for lumbar facet joint pain are medial branch blocks. The medial branches are the nociceptive supply to the facet joints (also multifidus and the interspinous space). It is a type of diagnostic nerve block. This is preferred over intra-articular blocks because the latter have not been formally validated.[2]
A needle is placed onto each of the two nerves that innervate the target facet joint. A tiny amount of local anaesthetic is injected (0.3-0.5mL) to achieve specificity for the target. This is visualised under fluoroscopy, however there has been more recent research using ultrasound.
The cut-off for a positive test varies, but in New Zealand we generally use 80% pain reduction, but some people use 100%. Some centres overseas use 50%. The International Spine Society procedure is that initially multiple facet joints are screened to identify those patients who don't have zygapophysial joint pain.
A single block has a high false positive rate, and so the blocks are controlled. Ideally this is done with placebo control. Due to resourcing constraints we usually do comparative blocks as the next best thing with accepting that there will still be some false positives even with two blocks (14% false positive for a concordant response, and 35% for discordant). Comparative blocks involves doing one injection with lidocaine and another with bupivacaine, and blinding the patient to the agent used (single blind). See Causes and Sources of Chronic Low Back Pain for a full discussion.
Because the chance of a false positive from a single block is high, and the prevalence of zygapophysial joint pain is low, the SIS guidelines recommend that in the ideal would screening blocks should be done initially at L5, L4, and L3, which covers the two lower segmental levels which are the most commonly affected. The utility of such a screening block is to identify patients who don't have zygapophysial joint pain. If the screening block is negative, all further investigations may cease, or the doctor and patient can decide to move on to investigation of another source such as the sacroiliac joints. If the screening block is positive, then further blocks are done to pinpoint the actual source, and confirmed by controlled blocks.
The indication for doing medial branch blocks is if radiofrequency neurotomy of the medial branches is being considered. If this isn't being considered then medial branch blocks are not indicated.[2]
Sacroiliac Joint Blocks
The gold standard test for sacroiliac joint pain is doing controlled intra-articular local anaesthetic blocks.
This procedure is technically more challenging than medial branch blocks, especially in the elderly where osteophytosis commonly makes needle entry difficult. Access to the joint cavity is confirmed with contrast injection, and then 2mL of local anaesthetic is injected into the joint. Fluoroscopic guidance is preferred.
The cut-off for a positive test again varies. Some use 100% relief of pain, while others use 75%. Also again, a single block has a false positive rate, and so controlled blocks are necessary.[2]
The indication for a sacroiliac joint block is if specific treatments are being considered such as sacroiliac joint fusion. Sacroiliac joint corticosteroid injections are commonly done, and it can be useful to follow the diagnostic technique while doing this in order to provide additional diagnostic value.
Sacral Lateral Branch Blocks
There is no current gold standard test for sacroiliac ligament pain, but this is emerging as a candidate. The interosseous ligament and dorsal ligamentous complex are not blocked by intra-articular sacroiliac joint injection (unless there is leak). These structures are innervated by the lateral branches of the S1-S3 dorsal rami and can be blocked with lateral branch blocks. The lateral branches emerge from the sacral foramina and pass laterally.
There are a few current limitations to this requiring further research. Firstly the prevalence of sacroiliac ligament pain is unknown. Secondly it is unknown whether sacroiliac ligament pain is a separate condition to sacroiliac joint pain or if they occur together. Thirdly the lateral branches have a variable course between people and even between sides within the same person which creates technical difficulties. There has been research into using multiple injections and using cooled radiofrequency which burns a larger area. Finally research needs to be done using controlled blocks.
The indication for sacral lateral branch blocks is to select patients for lateral branch radiofrequency neurotomy.[2]
Management
It can be illustrative to ask the patient what their expectations are in order to establish realistic treatment goals. There is often a big difference between what patients think a worthwhile pain reduction is (median 25%, IQR 20-50), and what they hope to achieve (median 80%, IQR 60-100). There is a consistency between desired reductions in pain and disability.[21] This bears emphasising, patients hope to achieve 60-100% pain relief. Note the huge difference between desired results and what is actually achieved in practice, and what is defined as "successful" in many trials (e.g. 1/10 pain reduction).
King and Bogduk note that expecting complete and enduring relief is not necessarily naive, as patients may have experiences with other types of pain being effectively and enduringly treated such as chronic toothache, chronic hip pain, etc. It is not surprising that patients therefore think that the source just needs to be found and then fixed.[2]
When looking at outcome data for any intervention, it is important to keep in mind a few things, including:
- often only average responses are recorded rather than categorical responses (i.e. reporting average pain reduction versus percentage of people that had 50%/100% pain reduction). There is some evidence that using average responses can lead to missing good outcomes achieved in subgroups of patients, as response rates may not be normally distributed.[22] Categorical analysis is preferred whenever possible.
- There may be regression to the mean i.e patients may enrol in a trial when they have a particularly bad flare, and they then naturally regress to their average pain levels. Therefore patients with acute flares should be excluded from trials.
- Most of the time monotherapies are tested without a pathoanatomic diagnosis ("nonspecific chronic low back pain"), or the diagnosis is based on history and physical examination which lacks reliability and validity. Similarly medical imaging typically doesn't help. So any theoretical benefit for one cause of pain would get lost in the data due to mixing with patients with other causes of pain.
- There is a difference between statistical significance and clinically meaningful change. To be sure any observed changes are clinically meaningful, real, and beyond measurement error, the following changes are needed for commonly used outcome measures: NRS of 2.4 (0-10 scale for pain), RMDQ of 4.9 (0-24 for function), and ODI of 16.7 (0-100 for function).[23] Another study reported an NRS of 2 to be clinically meaningful, and this number is commonly used in trials.[24]
Ideology
- Main article: Low Back Pain Treatment Strategies
The appropriate management of chronic low back pain is a political minefield. King and Bogduk write that the treatment literature on chronic low back pain is mired in ideology and vested interests.[2] There are "camps" or "craft groups" with different ideologies, and this biases their approach: the MDT group, the monotherapy group, and the reductionist group.
The patient's General Practitioner is the most important of all specialists as they can view the biases non-objectively from the outside without vested interests and tend to know the patient the best.
Good Back Consultation
- Main article: Good Back Consultation
The manner in which the doctor communicates can have an effect on outcomes. The following factors are important to consider, based on three interdisciplinary Norwegian RCTs for chronic low back pain.[25]
- Take them seriously
- Examination: explanation during the exam (what was being done and what was found)
- Education: Provide an understandable explanation for the pain given with conviction (exact medical diagnosis is not essential) and address misconceptions. He uses a disc injury explanation.
- Reassurance: given with conviction, address fears but cognitive reassurance is preferred over emotional which can create dependency.
- Psychosocial discussion: deal with possible correlation (in both directions) between daily life, job, family, coping, quality of life aspects, role function and the LBP
- Treatment: Encourage normal activity and avoiding rest. Empower the patient to take responsibility for their own rehabilitation.
Medical General Treatments
- Main article: Low Back Pain Medical Monotherapies
The evidence for conservative general therapies for chronic low back pain is very limited, and this includes both physical and pharmaceutical therapies. As a whole, they generally either have no effect at all, or only have modest short term effects. There are no general treatments that reach the reported expectations of patients.[21][2] Therefore any general treatment should not be promoted as a "cure," but rather as palliative options.
Oral Medication Therapies
The evidence for oral medications is very discouraging. Only NSAIDs and duloxetine have an effect, but it is debatable whether this is clinically meaningful. The common practice of prescribing TCAs and gabapentinoids is not based on evidence.[26][27] Similarly there is high quality evidence that opioids don't work, and if the patient is already on opioids they should be stopped as this is leads to some improvement in pain.[28][29]
No single drug will treat more than a minority of patients. Failure with one drug does not mean to expect failure with others, even within a class. Success or failure can be determined within 2-4 weeks. However, the evidence for pharmaceutical management is still limited.[22]
Bedside Needle Treatments
There is low quality evidence for short term modest relief of pain for tender point injections[30][31][32], total dorsal rami block[33], prolotherapy,[34][35] acupuncture, [36][37][38] and botox.[39] Acupuncture does not provide a long term effect, while the long term effect of the other interventions are unknown. Injections may have a very powerful placebo effect, with one RCT reporting that the primary outcome of 50% pain reduction was achieved by 46% in the prolotherapy group versus 36% for saline (no statistically significant difference), sustained for two years.[35]
Epidural Steroid Injections
Epidural injections are indicated for radicular pain not chronic low back pain.
For radicular pain there is good evidence for at least 50% pain relief in up to 70% of patients (see linked article). For back pain, epidural steroids do not appear to have an effect,[40] however further research is needed specifically on transforaminal epidural steroids for internal disc disruption.[2]
Spinal Cord Stimulation
This is a palliative treatment for radicular pain not back pain where it can lead to improvement in pain but generally not in function. There is a significant complication rate. It should only be considered for those with:
- Predominant radicular pain PLUS
- “Failed back surgery syndrome” PLUS
- Clear anatomical source of pain PLUS
- No abnormal illness behaviour PLUS
- A positive trial period with an external device
Burst stimulation is superior to tonic stimulation for most patients, and it allows placebo controlled trials due to the lack of paraesthesias.[41] It is extremely expensive with limited availability in NZ. The evidence may change as the technology improves.
Nonmedical General Treatments
- Main article: Low Back Pain Nonmedical Monotherapies
Physical Therapies
Physical activity has low quality evidence for being superior to hands on therapy for pain and function, and walking appears to be as good as other forms of physical activity.[42][43][44] In terms of specific exercises, there is low quality evidence that the most effective exercise treatments are Pilates, stabilisation/motor control, resistance training, and aerobic exercise training.[43] Back school doesn't have good evidence[45]
In an RCT of young adults with spondylolysis or spondylolisthesis and chronic back pain, a specific set of dynamic stabilising exercises was moderately superior to the control group.[46] As these radiographic findings don't correlate with chronic pain, this can be considered to be a study of undifferentiated patients.
Manual therapy has a modest short term effect without long-term benefit.[38][47] McKenzie may be superior to other interventions but the effect may not be clinically meaningful.[48][49][50] Massage only has evidence for modest short term relief and in this context it is significantly more effective than manual therapy, exercise, relaxation therapy, acupuncture, physiotherapy and TENS.[51][38]
There are no data to support the use of lumbar supports in chronic low back pain.[52] Traction[53] and TENS[54][55] don't seem to work or be superior to sham
Psychological Interventions
A review looking at CBT for all chronic pain except headache found that it had a very small benefit at treatment end for pain, disability, and distress. The effects were largely maintained at follow up for CBT versus treatment as usual, but not for CBT versus active control. The quality of the evidence was moderate to low for CBT. The quality of evidence for behavioural therapy and ACT was low, limiting conclusions for these modalities.[56]
Behavioural treatment (operant therapy) has moderate quality evidence in the short term than waiting list for a small reduction in pain, but no differences in the intermediate or long term. There is also no difference between behavioural therapy and group exercises. There is low-quality evidence that progressive relaxation therapy moderate improves pain compared to wait list controls.[57]
For mindfulness there is possibly better improvements in short-term pain and function compared with usual care or education. There are no differences between outcomes for mindfulness versus CBT.[38]
Combining physiotherapy and psychological therapies does not improve outcomes.[38] A recent variation called "cognitive functional therapy" was superior to manual therapy and exercise for function, but this was not clinically meaningful, and there was no benefit for pain.[58]
Multidisciplinary Rehabilitation
- Main article: Low Back Pain Multidisciplinary Rehabilitation
The culture of multidisciplinary rehabilitation in New Zealand tends to have a psychosocial focus and discourages the pursuit of finding the source of pain, and the patient tends to be labelled with Non-Specific Chronic Low Back Pain and central sensitisation. The basic premises that underlie multidisciplinary rehabilitation, as it is currently practiced without a biomedical domain, are problematic.
- Premise 1: "It isn't possible to identify the source of the pain" - The source of pain can indeed be found in most patients (see Causes and Sources of Chronic Low Back Pain).[1][3]
- Premise 2: "The injury has healed but the brain has a memory of pain" - The evidence does not support chronic nociceptive becoming "engraved" into the central nervous system (unlike with chronic neuropathic pain).[59][60]
It is not surprising then that MDT has a very small effect at most with pain reduction of 0.5-1.4 on 0-10 scale, and disability reduction of 1.4-2.5 on 0-24 Roland-Morris scale. It is also limited by cost, high time requirements, accessibility.[61] These changes are less than the minimal clinically important differences.[23] However, categorical data were not provided by the Cochrane review.[61] Integrating the full range of biomedical approaches with the full range of psychosocial approaches in MDT could theoretically achieve better outcomes then either individually, but ideology prevents this from happening.
The non-biomedical version of MDT should be reserved for patients with widespread chronic pain and demonstrable central sensitisation (e.g. as identified through simplified bedside quantitative sensory testing), of which the standard chronic low back pain patient does not fit under.[62] It may also be suitable for patients who are not interested in exploring the biomedical aspect of the biopsychosocial model, or who have a dual diagnosis of chronic low back pain and a mental health disorder or past trauma.
Precision Treatment
Precision treatments refer to specific, targeted treatments that are minimally invasive with the goal of relieving pain and secondarily improving function. Precision treatments are the only group of treatments for chronic low back pain that contain a couple key interventions that have been proven in RCTs to have a substantial effect on pain and function well in excess of minimally important change for pain, function, and distress, that persists in the medium term and long term (e.g. 12-18 months for radiofrequency neurotomy, and at least 5 years for basivertebral nerve ablation), Furthermore the quality of evidence is generally quite high due to the frequent use of double blinding with sham control.
The main limitations are cost (although it is an order of magnitude cheaper than spinal surgery), substantial training required for the doctor, accessibility, painstaking diagnostic process needed (hope and despair cycles can occur), and durability of response in the long term for sacral lateral branch and medial branch radiofrequency neurotomy. There is potentially a significant equity issue due to lack of access in the public system and only limited access under ACC.
Zygapophysial Joint Pain Precision Treatments
- Main article: Lumbar Facet Joint Precision Treatment
Intra-articular zygapophysial joint corticosteroid injection is a moderately common procedure, however multiple RCTs have found that it is no more effective than sham therapy.[63][64][65] In those that it does work, the effect may only last for a couple of weeks.
Therapeutic repeated medial branch blocks can be effective as a palliative therapy for pain reduction, but there is no improvement in return to work or use of opioids. Often patients have at least 50% pain relief for several weeks with each injection, and so it is simply repeated whenever the pain returns.[66] This is not generally done in New Zealand.
For facet joint pain medial branch radiofrequency neurotomy is a proven effective treatment.[67][68][69][70] This procedure involves thermally coagulating the sensory supply to the painful facet joint using a radiofrequency probe. The exact technique is paramount for effective outcome, with the Spine Intervention Society guidelines being the gold standard validated technique. Some trials have reported negative outcomes but have not followed the SIS guidelines on patient selection nor on technique.[2]
The indication for medial branch neurotomy is also very important, the patient must have had complete or near complete relief of pain with controlled diagnostic medial branch blocks. When this criteria is followed, success is ~55% when defined as complete relief of pain, full restoration of activities of daily living, and no need for continuing care for back pain. The effect is durable to a median of 15 months, and the procedure can be repeated.[70]
Discogenic Pain Precision Treatment
- Main article: Lumbar Disc Precision Treatment
The most common cause for discogenic pain is internal disc disruption. A variety of treatments have been developed.
Amongst intradisctal therapies, a small sham controlled RCT reported that intradiscal biacuplasty was superior to sham at 6 months with a mean reduction in pain of 2.9 and improvement of function of 22 (ODI). These are results that are generally of far greater magnitude than most if not all monotherapy treatments. However the reductionist philosophy aims for greater improvements, and the exclusion criteria were extensive.[20]
Similarly a small sham controlled trial found intradiscal PRP to be modestly superior to sham for both pain and function at 8 weeks.[71]
Other therapies are unproven and this includes intradiscal steroids (don't work), epidural steroids (short term effect only), transforaminal steroids (unknown), intradiscal etanercept (short term effect only), methylene blue (outcomes unable to be reproduced), proliferants (outcomes not reproduced), and stem cells (no superiority vs sham).[2]
For vertebrogenic pain (i.e. the presence of modic changes), basivertebral nerve ablation has been tested in a sham controlled RCT and found to be both highly effective (mean pain reduction 4.38 on a 0-10 scale, mean ODI reduction 25.95 on a 0-100 scale, 66% achieved >50% reduction in pain, 47% had >75% reduction, and 34% had complete resolution), and highly durable to five years following a single round of ablation treatment.[72][73]
Sacroiliac Joint Pain Precision Treatment
- Main article: Sacroiliac Joint Precision Treatment
Unfortunately many trials confuse sacroiliac joint pain and sacroiliac ligament pain, which clouds the interpretation of results.
Sacroiliac joint corticosteroid injections are a common procedure, and it is preferably done under fluoroscopic guidance. The best study was a retrospective case series in patients with sacroiliac joint pain as diagnosed by physical examination, up to two injections were allowed, and they reported a modest success rate in the short term, but 45% of those with two injections had >50% relief of an average of 36.8 weeks.[74]
For proven sacroiliac joint pain there is evidence for sacroiliac joint fusion[75][76]
For proven sacroiliac ligament pain there is lateral branch cooled radiofrequency neurotomy,[77][78] however the literature has generally confused sacroiliac joint pain with sacroiliac ligament pain by including patients with positive response to intraarticular sacroiliac joint blocks.
Only one sham controlled study selected patients by positive lateral branch blocks, but they were not controlled. At 6 months, in the intervention group >50% relief was achieved in 27% and 100% relief was achieved by 15%. The sample size was small and did not reach statistical significance.[78]
Intra-articular sacroiliac joint prolotherapy has also been studied as a precision treatment. For 48 patients with sacroiliac joint pain (pain below PSIS, positive Patrick or Gaenslens test, and single positive fluoroscopic block with a pain decrease of 50%), fluoroscopic injection of prolotherapy was compared to steroid. The exposure group had 2.5mL of 25% dextrose injected fluoroscopically every two weeks up to three times until relief of at least 90%. The control had the same but with triamcinolone 40mg. The outcomes were the same at 3 months, but the results of the prolotherapy group were durable up to 15 months.[79]
Surgery
- Main article: Lumbar Spine Surgery Overview
Unlike trials in most other treatment categories, there are no placebo controlled trials for any spinal surgery.
Radicular Pain
For radicular pain of 4-12 months duration, microdiscectomy is superior to non-operative care (included epidural injection)[80] Microdiscectomy outside of this time frame is not supported by the evidence. If it is done early, there is possibly more rapid recovery but no difference by 6 weeks.[81][82]
Fusion for Undifferentiated Pain
For undifferentiated chronic low back pain, fusion has been studied in four non-placebo controlled RCTs. A review of 33 meta-analyses of these four RCTs found that fusion is not more effective than intensive rehabilitation, and complications are common at 16%.[83] Another review looked at long term follow up of patients in these trials, and found that surgery was no better than CBT and exercise in both intention-to-treat and as-treated. Only 50-60% of patients in each group felt their back was better or much better.[84]
There has not been any RCT trials looking at fusion for diagnosed causes of chronic low back pain (i.e. discogenic pain or facet joint pain).
Disc Replacement
Lumbar disc replacement is a newer technique, and compared to active control there is a 12/100 point difference favouring surgery, but less than clinically significant benefit for disability. There are significant biases with industry sponsorship.[85][86]
References
- ↑ 1.0 1.1 1.2 DePalma MJ, Ketchum JM, Saullo TR. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain Med. 2012 Apr;13(4):498-506. doi: 10.1111/j.1526-4637.2012.01339.x. Epub 2012 Mar 5. PMID: 22390231.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 Wade King and Nikolai Bogduk. Chronic Low Back Pain In: Bonica's Management of Pain. 2018
- ↑ 3.0 3.1 DePalma MJ. Diagnostic Nihilism Toward Low Back Pain: What Once Was Accepted, Should No Longer Be. Pain Med. 2015 Aug;16(8):1453-4. doi: 10.1111/pme.12850. Epub 2015 Jul 27. PMID: 26218010.
- ↑ Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995 Jan 1;20(1):31-7. doi: 10.1097/00007632-199501000-00007. PMID: 7709277.
- ↑ Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976). 1996 Nov 15;21(22):2594-602. doi: 10.1097/00007632-199611150-00009. PMID: 8961447.
- ↑ Bogduk. Diagnostic Procedures in Chronic Pain In: Wilson's Chronic Pain. 2008
- ↑ Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976). 2008 Oct 15;33(22):2464-72. doi: 10.1097/BRS.0b013e318183a4a2. PMID: 18923325.
- ↑ 8.0 8.1 Bogduk N. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain. 2009 Dec 15;147(1-3):17-9. doi: 10.1016/j.pain.2009.08.020. Epub 2009 Sep 16. PMID: 19762151.
- ↑ Bogduk et al. Medical Management of Acute and Chronic Low Back Pain: An Evidence Based Approach. Elsevier Science. 2002
- ↑ 10.0 10.1 Bogduk and McGuirk. Assessment In: Medical Management of Acute and Chronic Low Back Pain. Elsevier 2002.
- ↑ Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49(2):89-97. doi: 10.1016/s0004-9514(14)60125-2. PMID: 12775204.
- ↑ Laslett M, Oberg B, Aprill CN, McDonald B. Centralization as a predictor of provocation discography results in chronic low back pain, and the influence of disability and distress on diagnostic power. Spine J. 2005 Jul-Aug;5(4):370-80. doi: 10.1016/j.spinee.2004.11.007. PMID: 15996606.
- ↑ May S, Aina A. Centralization and directional preference: a systematic review. Man Ther. 2012 Dec;17(6):497-506. doi: 10.1016/j.math.2012.05.003. Epub 2012 Jun 12. PMID: 22695365.
- ↑ Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms--a systematic review. Man Ther. 2004 Aug;9(3):134-43. doi: 10.1016/j.math.2004.03.004. PMID: 15245707.
- ↑ Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine (Phila Pa 1976). 1997 May 15;22(10):1115-22. doi: 10.1097/00007632-199705150-00011. PMID: 9160470.
- ↑ Revel M, Poiraudeau S, Auleley GR, Payan C, Denke A, Nguyen M, Chevrot A, Fermanian J. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine (Phila Pa 1976). 1998 Sep 15;23(18):1972-6; discussion 1977. doi: 10.1097/00007632-199809150-00011. PMID: 9779530.
- ↑ 17.0 17.1 17.2 Bogduk N, Aprill C, Derby R. Lumbar discogenic pain: state-of-the-art review. Pain Med. 2013 Jun;14(6):813-36. doi: 10.1111/pme.12082. Epub 2013 Apr 8. PMID: 23566298.
- ↑ 18.0 18.1 Fischgrund JS, et al. Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: 2-Year Results From a Prospective Randomized Double-Blind Sham-Controlled Multicenter Study. Int J Spine Surg. 2019 Apr 30;13(2):110-119. doi: 10.14444/6015. PMID: 31131209; PMCID: PMC6510180.
- ↑ Bogduk. Low back pain In: Clinical and Radiological Anatomy of the Lumbar Spine. 5th Edition. Elsevier 2012
- ↑ 20.0 20.1 Kapural L, Vrooman B, Sarwar S, Krizanac-Bengez L, Rauck R, Gilmore C, North J, Mekhail N. Radiofrequency intradiscal biacuplasty for treatment of discogenic lower back pain: a 12-month follow-up. Pain Med. 2015 Mar;16(3):425-31. doi: 10.1111/pme.12595. Epub 2014 Oct 23. PMID: 25339501.
- ↑ 21.0 21.1 Yelland MJ, Schluter PJ. Defining worthwhile and desired responses to treatment of chronic low back pain. Pain Med. 2006 Jan-Feb;7(1):38-45. doi: 10.1111/j.1526-4637.2006.00087.x. PMID: 16533195.
- ↑ 22.0 22.1 Moore A, Derry S, Eccleston C, Kalso E. Expect analgesic failure; pursue analgesic success. BMJ. 2013 May 3;346:f2690. doi: 10.1136/bmj.f2690. PMID: 23645858.
- ↑ 23.0 23.1 Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J. 2010 Sep;19(9):1484-94. doi: 10.1007/s00586-010-1353-6. Epub 2010 Apr 17. PMID: 20397032; PMCID: PMC2989277.
- ↑ Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005 Jun 1;30(11):1331-4. doi: 10.1097/01.brs.0000164099.92112.29. PMID: 15928561.
- ↑ Laerum E, Indahl A, Skouen JS. What is "the good back-consultation"? A combined qualitative and quantitative study of chronic low back pain patients' interaction with and perceptions of consultations with specialists. J Rehabil Med. 2006 Jul;38(4):255-62. doi: 10.1080/16501970600613461. PMID: 16801209.
- ↑ Chou R, Deyo R, Friedly J, Skelly A, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S. Systemic Pharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017 Apr 4;166(7):480-492. doi: 10.7326/M16-2458. Epub 2017 Feb 14. PMID: 28192790.
- ↑ Moore RA, Straube S, Wiffen PJ, Derry S, McQuay HJ. Pregabalin for acute and chronic pain in adults. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD007076. doi: 10.1002/14651858.CD007076.pub2. Update in: Cochrane Database Syst Rev. 2019 Jan 23;1:CD007076. PMID: 19588419; PMCID: PMC4167351.
- ↑ Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, Kroenke K, Bair MJ, Noorbaloochi S. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA. 2018 Mar 6;319(9):872-882. doi: 10.1001/jama.2018.0899. PMID: 29509867; PMCID: PMC5885909.
- ↑ McPherson S, Lederhos Smith C, Dobscha SK, Morasco BJ, Demidenko MI, Meath THA, Lovejoy TI. Changes in pain intensity after discontinuation of long-term opioid therapy for chronic noncancer pain. Pain. 2018 Oct;159(10):2097-2104. doi: 10.1097/j.pain.0000000000001315. PMID: 29905648; PMCID: PMC6993952.
- ↑ Malanga G, Wolff E. Evidence-informed management of chronic low back pain with trigger point injections. Spine J. 2008 Jan-Feb;8(1):243-52. doi: 10.1016/j.spinee.2007.10.029. PMID: 18164472.
- ↑ Garvey TA, Marks MR, Wiesel SW. A prospective, randomized, double-blind evaluation of trigger-point injection therapy for low-back pain. Spine (Phila Pa 1976). 1989 Sep;14(9):962-4. doi: 10.1097/00007632-198909000-00008. PMID: 2528826.
- ↑ Kocak AO, Ahiskalioglu A, Sengun E, Gur STA, Akbas I. Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: A prospective randomized study. Am J Emerg Med. 2019 Oct;37(10):1927-1931. doi: 10.1016/j.ajem.2019.01.015. Epub 2019 Jan 15. PMID: 30660342.
- ↑ Miyakoshi N, Shimada Y, Kasukawa Y, Saito H, Kodama H, Itoi E. Total dorsal ramus block for the treatment of chronic low back pain: a preliminary study. Joint Bone Spine. 2007 May;74(3):270-4. doi: 10.1016/j.jbspin.2006.07.006. Epub 2007 Mar 7. PMID: 17383923.
- ↑ Dagenais S, Yelland MJ, Del Mar C, Schoene ML. Prolotherapy injections for chronic low-back pain. Cochrane Database Syst Rev. 2007 Apr 18;2007(2):CD004059. doi: 10.1002/14651858.CD004059.pub3. PMID: 17443537; PMCID: PMC6986690.
- ↑ 35.0 35.1 Yelland MJ, Glasziou PP, Bogduk N, Schluter PJ, McKernon M. Prolotherapy injections, saline injections, and exercises for chronic low-back pain: a randomized trial. Spine (Phila Pa 1976). 2004 Jan 1;29(1):9-16; discussion 16. doi: 10.1097/01.BRS.0000105529.07222.5B. PMID: 14699269.
- ↑ FurlanAD, van TulderMW, CherkinD, TsukayamaH, LaoL, KoesBW, BermanBM. Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No.: CD001351. DOI: 10.1002/14651858.CD001351.pub2.
- ↑ Xiang Y, He JY, Tian HH, Cao BY, Li R. Evidence of efficacy of acupuncture in the management of low back pain: a systematic review and meta-analysis of randomised placebo- or sham-controlled trials. Acupunct Med. 2020;38(1):15-24. doi:10.1136/acupmed-2017-011445
- ↑ 38.0 38.1 38.2 38.3 38.4 Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S, Brodt ED. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017 Apr 4;166(7):493-505. doi: 10.7326/M16-2459. Epub 2017 Feb 14. PMID: 28192793.
- ↑ Waseem Z, Boulias C, Gordon A, Ismail F, Sheean G, Furlan AD. Botulinum toxin injections for low-back pain and sciatica. Cochrane Database Syst Rev. 2011 Jan 19;(1):CD008257. doi: 10.1002/14651858.CD008257.pub2. PMID: 21249702.
- ↑ Oliveira CB, Maher CG, Ferreira ML, Hancock MJ, Oliveira VC, McLachlan AJ, Koes BW, Ferreira PH, Cohen SP, Pinto RZ. Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst Rev. 2020 Apr 9;4(4):CD013577. doi: 10.1002/14651858.CD013577. PMID: 32271952; PMCID: PMC7145384.
- ↑ Kirketeig T, Schultheis C, Zuidema X, Hunter CW, Deer T. Burst Spinal Cord Stimulation: A Clinical Review. Pain Med. 2019 Jun 1;20(Suppl 1):S31-S40. doi: 10.1093/pm/pnz003. PMID: 31152175; PMCID: PMC6544556.
- ↑ GeneenLJ, MooreRA, ClarkeC, MartinD, ColvinLA, SmithBH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database of Systematic Reviews 2017, Issue 4. Art. No.: CD011279. DOI: 10.1002/14651858.CD011279.pub3.
- ↑ 43.0 43.1 Owen et al.. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. British journal of sports medicine 2020. 54:1279-1287. PMID: 31666220. DOI. Full Text.
- ↑ Vanti C, Andreatta S, Borghi S, Guccione AA, Pillastrini P, Bertozzi L. The effectiveness of walking versus exercise on pain and function in chronic low back pain: a systematic review and meta-analysis of randomized trials. Disabil Rehabil. 2019 Mar;41(6):622-632. doi: 10.1080/09638288.2017.1410730. Epub 2017 Dec 5. PMID: 29207885.
- ↑ ParreiraP, HeymansMW, van TulderMW, EsmailR, KoesBW, PoquetN, LinCWC, MaherCG. Back Schools for chronic non-specific low back pain. Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD011674. DOI: 10.1002/14651858.CD011674.pub2.
- ↑ O'Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976). 1997 Dec 15;22(24):2959-67. doi: 10.1097/00007632-199712150-00020. PMID: 9431633.
- ↑ Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J. 2008 Jan-Feb;8(1):213-25. doi: 10.1016/j.spinee.2007.10.023. PMID: 18164469.
- ↑ Machado LA, de Souza Mv, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine (Phila Pa 1976). 2006 Apr 20;31(9):E254-62. doi: 10.1097/01.brs.0000214884.18502.93. PMID: 16641766.
- ↑ Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004;50(4):209-16. doi: 10.1016/s0004-9514(14)60110-0. PMID: 15574109.
- ↑ Lam OT, Strenger DM, Chan-Fee M, Pham PT, Preuss RA, Robbins SM. Effectiveness of the McKenzie Method of Mechanical Diagnosis and Therapy for Treating Low Back Pain: Literature Review With Meta-analysis. J Orthop Sports Phys Ther. 2018 Jun;48(6):476-490. doi: 10.2519/jospt.2018.7562. Epub 2018 Mar 30. PMID: 29602304.
- ↑ Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M. Massage for low-back pain. Cochrane Database Syst Rev. 2015 Sep 1;(9):CD001929. doi: 10.1002/14651858.CD001929.pub3. PMID: 26329399.
- ↑ Oleske DM, Lavender SA, Andersson GB, Kwasny MM. Are back supports plus education more effective than education alone in promoting recovery from low back pain?: Results from a randomized clinical trial. Spine (Phila Pa 1976). 2007 Sep 1;32(19):2050-7. doi: 10.1097/BRS.0b013e3181453fcc. PMID: 17762804.
- ↑ James McKivigan, Brittany Krisak, Brittni Vogel, Ashley Harrington, Van Nguyen. Evaluating the Efficacy of Vertebral Axial Decompression Therapy in Treatment of Patients with Chronic Lower Back Pain: A Systematic Review. Rehabilitation Science. Vol. 4, No. 2, 2019, pp. 25-34. doi: 10.11648/j.rs.20190402.12
- ↑ Cochrane: WegnerI, WidyaheningIS, van TulderMW, BlombergSEI, de VetHCW, BrønfortG, BouterLM, van der HeijdenGJ.Traction for low-back pain with or without sciatica. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD003010. DOI: 10.1002/14651858.CD003010.pub5.
- ↑ Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst Rev. 2008 Oct 8;2008(4):CD003008. doi: 10.1002/14651858.CD003008.pub3. PMID: 18843638; PMCID: PMC7138213.
- ↑ Williams ACC, Fisher E, Hearn L, Eccleston C. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2020 Aug 12;8(8):CD007407. doi: 10.1002/14651858.CD007407.pub4. PMID: 32794606; PMCID: PMC7437545.
- ↑ Henschke N, Ostelo RW, van Tulder MW, Vlaeyen JW, Morley S, Assendelft WJ, Main CJ. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev. 2010 Jul 7;2010(7):CD002014. doi: 10.1002/14651858.CD002014.pub3. PMID: 20614428; PMCID: PMC7065591.
- ↑ Vibe Fersum K, Smith A, Kvåle A, Skouen JS, O'Sullivan P. Cognitive functional therapy in patients with non-specific chronic low back pain-a randomized controlled trial 3-year follow-up. Eur J Pain. 2019 Sep;23(8):1416-1424. doi: 10.1002/ejp.1399. Epub 2019 May 14. PMID: 30974479.
- ↑ Cohen M, Quintner J, Buchanan D. Is chronic pain a disease? Pain Med. 2013 Sep;14(9):1284-8. doi: 10.1111/pme.12025. Epub 2013 Jan 7. PMID: 23294511.
- ↑ Curatolo M, Arendt-Nielsen L, Petersen-Felix S. Central hypersensitivity in chronic pain: mechanisms and clinical implications. Phys Med Rehabil Clin N Am. 2006 May;17(2):287-302. doi: 10.1016/j.pmr.2005.12.010. PMID: 16616268.
- ↑ 61.0 61.1 Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ.E.M., Ostelo RWJG, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database of Systematic Reviews 2014, Issue 9. Art. No.: CD000963. DOI: 10.1002/14651858.CD000963.pub3
- ↑ Julien N, Goffaux P, Arsenault P, Marchand S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain. 2005 Mar;114(1-2):295-302. doi: 10.1016/j.pain.2004.12.032. PMID: 15733656.
- ↑ Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, Latulippe M. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991 Oct 3;325(14):1002-7. doi: 10.1056/NEJM199110033251405. PMID: 1832209.
- ↑ Lilius G, Laasonen EM, Myllynen P, Harilainen A, Grönlund G. Lumbar facet joint syndrome. A randomised clinical trial. J Bone Joint Surg Br. 1989 Aug;71(4):681-4. doi: 10.1302/0301-620X.71B4.2527856. PMID: 2527856.
- ↑ Lilius G, Harilainen A, Laasonen EM, Myllynen P. Chronic unilateral low-back pain. Predictors of outcome of facet joint injections. Spine (Phila Pa 1976). 1990 Aug;15(8):780-2. PMID: 2146756.
- ↑ Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V. Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up. Int J Med Sci. 2010 May 28;7(3):124-35. doi: 10.7150/ijms.7.124. PMID: 20567613; PMCID: PMC2880841.
- ↑ Cohen SP, Williams KA, Kurihara C, Nguyen C, Shields C, Kim P, Griffith SR, Larkin TM, Crooks M, Williams N, Morlando B, Strassels SA. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010 Aug;113(2):395-405. doi: 10.1097/ALN.0b013e3181e33ae5. PMID: 20613471.
- ↑ Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine (Phila Pa 1976). 2008 May 20;33(12):1291-7; discussion 1298. doi: 10.1097/BRS.0b013e31817329f0. PMID: 18496338.
- ↑ Moussa WM, Khedr W. Percutaneous radiofrequency facet capsule denervation as an alternative target in lumbar facet syndrome. Clin Neurol Neurosurg. 2016 Nov;150:96-104. doi: 10.1016/j.clineuro.2016.09.004. Epub 2016 Sep 5. PMID: 27618781.
- ↑ 70.0 70.1 MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2013 May;14(5):639-45. doi: 10.1111/pme.12000. Epub 2012 Dec 28. PMID: 23279154.
- ↑ Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R. 2016 Jan;8(1):1-10; quiz 10. doi: 10.1016/j.pmrj.2015.08.010. Epub 2015 Aug 24. PMID: 26314234.
- ↑ Fischgrund JS, et al. Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: 2-Year Results From a Prospective Randomized Double-Blind Sham-Controlled Multicenter Study. Int J Spine Surg. 2019 Apr 30;13(2):110-119. doi: 10.14444/6015. PMID: 31131209; PMCID: PMC6510180.
- ↑ Fischgrund JS, Rhyne A, Macadaeg K, Moore G, Kamrava E, Yeung C, Truumees E, Schaufele M, Yuan P, DePalma M, Anderson DG, Buxton D, Reynolds J, Sikorsky M. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020 Aug;29(8):1925-1934. doi: 10.1007/s00586-020-06448-x. Epub 2020 May 25. PMID: 32451777.
- ↑ Liliang PC, Lu K, Weng HC, Liang CL, Tsai YD, Chen HJ. The therapeutic efficacy of sacroiliac joint blocks with triamcinolone acetonide in the treatment of sacroiliac joint dysfunction without spondyloarthropathy. Spine (Phila Pa 1976). 2009 Apr 20;34(9):896-900. doi: 10.1097/BRS.0b013e31819e2c78. PMID: 19531998.
- ↑ Polly DW, et al. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg. 2016 Aug 23;10:28. doi: 10.14444/3028. PMID: 27652199; PMCID: PMC5027818.
- ↑ Dengler J, et al. Randomized Trial of Sacroiliac Joint Arthrodesis Compared with Conservative Management for Chronic Low Back Pain Attributed to the Sacroiliac Joint. J Bone Joint Surg Am. 2019 Mar 6;101(5):400-411. doi: 10.2106/JBJS.18.00022. PMID: 30845034; PMCID: PMC6467578.
- ↑ Cohen SP, Hurley RW, Buckenmaier CC 3rd, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008 Aug;109(2):279-88. doi: 10.1097/ALN.0b013e31817f4c7c. PMID: 18648237; PMCID: PMC2666931.
- ↑ 78.0 78.1 Patel N. Twelve-Month Follow-Up of a Randomized Trial Assessing Cooled Radiofrequency Denervation as a Treatment for Sacroiliac Region Pain. Pain Pract. 2016 Feb;16(2):154-67. doi: 10.1111/papr.12269. Epub 2015 Jan 7. PMID: 25565322.
- ↑ Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16(12):1285‐1290. doi:10.1089/acm.2010.0031
- ↑ Bailey CS, Rasoulinejad P, Taylor D, Sequeira K, Miller T, Watson J, Rosedale R, Bailey SI, Gurr KR, Siddiqi F, Glennie A, Urquhart JC. Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months. N Engl J Med. 2020 Mar 19;382(12):1093-1102. doi: 10.1056/NEJMoa1912658. PMID: 32187469
- ↑ Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008 Jun 14;336(7657):1355-8. doi: 10.1136/bmj.a143. Epub 2008 May 23. PMID: 18502911; PMCID: PMC2427077.
- ↑ Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine (Phila Pa 1976). 2006 Oct 1;31(21):2409-14. doi: 10.1097/01.brs.0000239178.08796.52. PMID: 17023847.
- ↑ Harris IA, Traeger A, Stanford R, Maher CG, Buchbinder R. Lumbar spine fusion: what is the evidence? Intern Med J. 2018 Dec;48(12):1430-1434. doi: 10.1111/imj.14120. PMID: 30517997.
- ↑ Mannion AF, Brox JI, Fairbank JC. Comparison of spinal fusion and nonoperative treatment in patients with chronic low back pain: long-term follow-up of three randomized controlled trials. Spine J. 2013 Nov;13(11):1438-48. doi: 10.1016/j.spinee.2013.06.101. Epub 2013 Nov 5. PMID: 24200413.
- ↑ Hellum C, Johnsen LG, Storheim K, Nygaard OP, Brox JI, Rossvoll I, Rø M, Sandvik L, Grundnes O; Norwegian Spine Study Group. Surgery with disc prosthesis versus rehabilitation in patients with low back pain and degenerative disc: two year follow-up of randomised study. BMJ. 2011 May 19;342:d2786. doi: 10.1136/bmj.d2786. PMID: 21596740; PMCID: PMC3100911.
- ↑ Jacobs WC, van der Gaag NA, Kruyt MC, Tuschel A, de Kleuver M, Peul WC, Verbout AJ, Oner FC. Total disc replacement for chronic discogenic low back pain: a Cochrane review. Spine (Phila Pa 1976). 2013 Jan 1;38(1):24-36. doi: 10.1097/BRS.0b013e3182741b21. PMID: 22996268.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,