Dermatomes: Difference between revisions
No edit summary |
No edit summary |
||
| Line 52: | Line 52: | ||
*Prefixed brachial plexus (large contribution from C4 with or without a small T1 contribution){{#pmid:20087592|pellerin}} | *Prefixed brachial plexus (large contribution from C4 with or without a small T1 contribution){{#pmid:20087592|pellerin}} | ||
*The [[Furcal Nerve|furcal nerve]]. Furcal means forked. This is an independent nerve with its own ventral and dorsal branches (rootlets) and it forms a link between the lumbar and sacral plexuses. It is most commonly found at L4, with L3 being the next most common site. This can cause an atypical presentation of sciatica. | *The [[Furcal Nerve|furcal nerve]]. Furcal means forked. This is an independent nerve with its own ventral and dorsal branches (rootlets) and it forms a link between the lumbar and sacral plexuses. It is most commonly found at L4, with L3 being the next most common site. This can cause an atypical presentation of sciatica. | ||
*[[Transitional Vertebral Anatomy|Transitional lumbosacral anatomy]] may result in the L4 nerve root serving the usual function of L5 in L5 sacralisation, and the S1 nerve root serving the usual function of L5 in S1 lumbarisation.<ref>{{#pmid:29363131}}</ref> | |||
Some people with [[Lumbar Radicular Pain|sciatica]] have a band like pain and others only have distal pain. Buttock pain in those with a band-like pain is common in sciatica. The lumbosacral region and buttock share a similar segmental nerve supply (L4-S1). The low back is innervated by the dorsal rami of L4-S1 and the deep buttock by the ventral rami. Stimulation of the sinuvertebral nerves that innervate the dural sleeve may be a source of somatic referred pain. As an alternative or additional explanation, the lateral thigh is innervated by the lateral femoral cutaneous nerve of the thigh. This is innervated by L2-3, and it can overlap with the L4 and L5 dermatomes. In individuals with dense overlap, they may not report anaesthesia over the thigh with an L4 or L5 lesion.<ref name="Nitta"/><ref>Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Edinburgh: Elsevier/Churchill Livingstone, 2012</ref> | Some people with [[Lumbar Radicular Pain|sciatica]] have a band like pain and others only have distal pain. Buttock pain in those with a band-like pain is common in sciatica. The lumbosacral region and buttock share a similar segmental nerve supply (L4-S1). The low back is innervated by the dorsal rami of L4-S1 and the deep buttock by the ventral rami. Stimulation of the sinuvertebral nerves that innervate the dural sleeve may be a source of somatic referred pain. As an alternative or additional explanation, the lateral thigh is innervated by the lateral femoral cutaneous nerve of the thigh. This is innervated by L2-3, and it can overlap with the L4 and L5 dermatomes. In individuals with dense overlap, they may not report anaesthesia over the thigh with an L4 or L5 lesion.<ref name="Nitta"/><ref>Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Edinburgh: Elsevier/Churchill Livingstone, 2012</ref> | ||
Revision as of 08:20, 2 May 2021
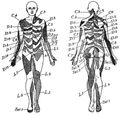
The term dermatome generally refers to an area of skin innervated by a particular neural element, specifically nerve root, dorsal root ganglion or spinal segment. These are distinct from the cutaneous nerve distributions. Dermatomes are dynamic, and can expand and shrink, and vary depending on the precise structure being tested and the method of testing.
Dermatome Maps
Historically, there are two major types of dermatome maps. There is the Haymaker type which originates from Foerster, and the Keegan type. The Haymaker type presents regions of spinal segments having an insular form. The Keegan type shows regions with continuous bandlike zones from proximal to distal. These difference relate to differences in opinion regarding the embryology of dermatomes in the extremities. Bolk's theory was that the dermatomes shift in an insular form to the periphery as the extremities grow. Keegan's theory was that they expand to form a band-like zone.[1]
The most up to date dermatome map is probably that published by Lee et al. They created a composite image taken from published data that they thought was the most reliable. [2] The winding band like dermatomal map seen in some textbooks was from Keegan and Garrett is the most flawed of all dermatomal maps and was not included. Lee et al's map is most consistent tactile dermatomal regions for each spinal dorsal nerve root. The midline has minimal overlap, but otherwise there is extensive and variable overlap. Blank areas on the map represent areas where there is very large degree of variability and overlap. The S3, S4, and S5 cutaneous supply is not shown.
Radicular pain does not necessarily follow dermatomal distribution.[3] See Lumbar Radicular Pain and Cervical Radicular Pain.
Other Maps
See Downs et al on the history of dermatome maps.[4]
| Authors | Year | Basis of Map | Findings | Weaknesses |
|---|---|---|---|---|
| Herringham | 1886 | The first account of the distribution of segmental nerve fibres into the upper limb based on dissection | Axial line. The dermatomes in the preaxial area (C5-6) are higher than those in the post axial area (C8-T1). In the preaxial area the forearm (C6) is supplied by a lower nerve than the arm (C5), in the post axial area the forearm (C8) is supplied by a higher nerve than the arm (T1-2) | Only based on dissection and theory. |
| Sherington | 1893 | Severing dorsal nerve roots in monkeys and testing sensation, distributions drawn on a plaster cast of a monkey. | Adjacent dermatomes overlap, except for proximal aspects of the limbs. Nerve fibre density is lower towards the periphery of a dermatome | Animal based study |
| Head and Campbell | 1900 | Zoster eruptions in 450 patients, with histological confirmation in some subjects. | Noted some overlap, changed with body shape and age. Uniquely studied the thoracic dermatomes. | Histological confirmation in only 16 cases. No recorded examples of C5-C8 or root levels below L1. Assumptions were made about the exact dorsal root involved. Herpetic eruptions can affect several adjacent levels. Not all cutaneous fibres will necessarily be infected. |
| Fender and Foerster | 1933 and 1936 | Residual area of sensation after surgically isolating single dorsal nerve roots. L1 to S2 isolated by dividing nerve roots above and below the target level. Cervical dermatomes mostly assessed by dividing nerve roots either above or below thus obtaining proximal and distal boundaries only. Vasodilation following electrical stimulation supplemented the data. Population those with spasticity (mostly those with tabes dorsalis). | Areas vary between individuals, except in the midline. Tactile dermatomes are larger than those determined by pain and temperature. With the exception of C2 there is no sensory loss if only one nerve root is sectioned. | Relatively few subjects, poorly documented methods and testing protocol, no information about time interval between sectioning and testing. |
| Keegan and Garrett | 1948 | Diminished cutaneous sensitivity of "light pin-scratch" from disc prolapse causing nerve root compression, majority confirmed by myelography, some confirmed surgically. 165 prolapses at C5-T1. 1264 prolapses at L3-S2. Supplemented with nerve root sectioning in 13, and radiologically guided local anaesthetic injection into lower cervical nerve roots in 10 medical students. | Neat nonoverlapping bands running down the limbs from the posterior midline. They acknowledged that the mapping did not represent the complete distribution and dermatomes do overlap. They disputed Foerster on the findings of division of a single nerve root not causing diminished sensation. | The most flawed of the three core maps. Their findings have never been replicated. Some dermatomes not assessed but appear in chart (e.g. L1 and L2, and truncal dermatomes). They reported that the area of hypoalgesia was reproducible and non-variable which differs from other reports. Does not fit with our embryological understanding. Predates our understanding of how disc prolapse in one segment can cause compression of the traversing nerve root, this will not have been picked up on myelography. Doesn't take into account compression of multiple nerve roots. |
| Davis et al | 1952 | 500 patients with disc prolapse mostly L4-5 and L5-S1, verified by myelography and surgery. Sensory changes mapped by independent assessors with light touch and pin prick. | Areas of sensory loss of L5 and S1 very variable between subjects, and there was also variation between assessors. They did not find narrow bands of hypo-aesthesia like Keegan and Garrett. Half of the patients had sensory changes of the foot and leg only. Thought variability related to extent and location of herniated disc | |
| Nitta et al[5] | 1993 | 71 patients suffering lumbosacral radicular symptoms had 86 fluoroscopically guided lumbar spinal nerve blocks. Sensory deficits were mapped for L4-S1. | Distinctive regions: L4 is medial side of the lower leg in 88%. L5 is first dorsal digit in 82%. S1 is lateral side of 5th digit in 83%. Band like deficits: L4 was 42%, L5 was 44%, S1 was 92%. See Lumbar Radicular Pain | Cases of lumbosacral transitional vertebrae were not included. |
| Lee et al[2] | 2008 | Redrew the Head and Campbell, and Foerster maps from the original photographs onto a figure outline. The figures were overlaid, and the areas that did not overlap were deleted. This new template was then modified in the light of other good category evidence data for C6, C7, and C8 (Inouye and Buchthal, 1977) and L4, L5, and S1 (Cole et al., 1968; Nitta et al., 1993). | The lumbosacral variability is greater than cervical. Adjacent dermatomes overlap to a variable degree. Dermatomes in the hand overlap to a large degree. Variability may be explained by the following reasons. Almost all areas of the skin are supplied by two or more spinal nerve roots. Intrathecal intersegmental anastamoses are common. The distribution of a dorsal root is slightly different to that of a dorsal root ganglion, and these areas are influenced by spinal cord processing. Dermatomes vary based on the method of assessment, the type of sensation tested, and the precise neural element being tested | No independent data |
Dermatome Concept Validity
The dermatome concept is based on the assumption that there is a direct and static correlation between nerve supply and skin sensation. Nerve signals are in fact highly dynamic. Nerve fibres are less dense towards the periphery of a dermatome, so dermatome maps may actually reflect maximum innervation. Cutaneous innervation of the dorsal root ganglia is different to that of the dorsal root as discovered through sectioning monkey nerves proximal and distal to the dorsal root ganglion. The Lissaeur tract can facilitate and suppress sensory impulses, corresponding to dermatomal expansion or reduction.[6]
There are many very common anatomical variations that will also affect dermatomal mapping.
- Intrathecal intersegmental anastamoses between the dorsal spinal rootlets [7], with the greatest variation in upper limb dermatomes
- Postfixed brachial plexus (large contribution from T2 with or without a small C5 contribution)[8]
- Prefixed brachial plexus (large contribution from C4 with or without a small T1 contribution)[8]
- The furcal nerve. Furcal means forked. This is an independent nerve with its own ventral and dorsal branches (rootlets) and it forms a link between the lumbar and sacral plexuses. It is most commonly found at L4, with L3 being the next most common site. This can cause an atypical presentation of sciatica.
- Transitional lumbosacral anatomy may result in the L4 nerve root serving the usual function of L5 in L5 sacralisation, and the S1 nerve root serving the usual function of L5 in S1 lumbarisation.[9]
Some people with sciatica have a band like pain and others only have distal pain. Buttock pain in those with a band-like pain is common in sciatica. The lumbosacral region and buttock share a similar segmental nerve supply (L4-S1). The low back is innervated by the dorsal rami of L4-S1 and the deep buttock by the ventral rami. Stimulation of the sinuvertebral nerves that innervate the dural sleeve may be a source of somatic referred pain. As an alternative or additional explanation, the lateral thigh is innervated by the lateral femoral cutaneous nerve of the thigh. This is innervated by L2-3, and it can overlap with the L4 and L5 dermatomes. In individuals with dense overlap, they may not report anaesthesia over the thigh with an L4 or L5 lesion.[1][10]
Testing Dermatomes
The area of testing will be determined by history. It is not necessary normally to test all dermatomes. Ask the patient where they have altered sensation and its borders. Dermatomes can be sampled by moving distal to proximal. Move along the long axis of the medial and lateral aspects of the upper and lower limbs, and caudal to cranial along both sides of the trunk.
Test for pin prick sensation in the dermatomes. Temperature sensation can be tested, but this is usually omitted if pinprick sensation is normal. Cold sensation can be tested by using the metal of a tuning fork. Light touch adds little additional information, and is usually tested with a wisp of cotton wool or a light finger touch to the skin. The area of deficit to light touch is often larger than that of pin prick.
If an area of sensory deficit is detected to pinprick, then examine from the centre of maximum deficit and move outwards to define the borders. If there is an area of increased sensation (e.g. hyperalgesia), then the mapping should be done in the reverse direction outwards to inwards.
ASIA Landmarks
Dermatomal landmarks are commonly used and are based on ASIA's publication, called "key sensory points." The landmarks are highly questionable as it is not actually apparent how ASIA determined them, and whether there is even such a thing as an autonomous area. The supposed unique landmarks for T3-T12 are especially dubious as this was only studied by Head and Campbell in 1900.
| Nerve root | ASIA | Comment |
|---|---|---|
| C2 | At least one cm lateral to the occipital protuberance at the base of the skull. Alternately, a point at least 3 cm behind the ear. | |
| C3 | In the supraclavicular fossa, at the midclavicular line. | |
| C4 | Over the acromioclavicular joint. | |
| C5 | On the lateral (radial) side of the antecubital fossa, just proximally to the elbow. | This is C6-C7 based on Lee. Autonomous region should be regimental badge area |
| C6 | On the dorsal surface of the proximal phalanx of the thumb. | Considerable overlap with C7 |
| C7 | On the dorsal surface of the proximal phalanx of the middle finger. | Considerable overlap with C6 and C8 |
| C8 | On the dorsal surface of the proximal phalanx of the little finger. | Considerable overlap with T1 |
| T1 | On the medial (ulnar) side of the antecubital fossa, just proximally to the medial epicondyle of the humerus. | dubious |
| T2 | At the apex of the axilla. | dubious |
| T3 | Intersection of the midclavicular line and the third intercostal space | dubious |
| T4 | Intersection of the midclavicular line and the fourth intercostal space, located at the level of the nipples. | dubious |
| T5 | Intersection of the midclavicular line and the fifth intercostal space, horizontally located midway between the level of the nipples and the level of the xiphoid process. | dubious |
| T6 | Intersection of the midclavicular line and the horizontal level of the xiphoid process. | dubious |
| T7 | Intersection of the midclavicular line and the horizontal level at one quarter the distance between the level of the xiphoid process and the level of the umbilicus. | dubious |
| T8 | Intersection of the midclavicular line and the horizontal level at one half the distance between the level of the xiphoid process and the level of the umbilicus. | dubious |
| T9 | Intersection of the midclavicular line and the horizontal level at three quarters of the distance between the level of the xiphoid process and the level of the umbilicus. | dubious |
| T10 | Intersection of the midclavicular line, at the horizontal level of the umbilicus. | dubious |
| T11 | Intersection of the midclavicular line, at the horizontal level midway between the level of the umbilicus and the inguinal ligament. | dubious |
| T12 | Intersection of the midclavicular line and the midpoint of the inguinal ligament. | dubious |
| L1 | Midway between the key sensory points for T12 and L2. | |
| L2 | On the anterior medial thigh, at the midpoint of a line connecting the midpoint of the inguinal ligament and the medial epicondyle of the femur. | |
| L3 | At the medial epicondyle of the femur. | |
| L4 | Over the medial malleolus. | Medial side of the lower leg in 88%.[1] |
| L5 | On the dorsum of the foot at the third metatarsophalangeal joint. (Note hallux can be supplied by L4) | First dorsal digit in 82%[1] |
| S1 | On the lateral aspect of the calcaneus. | lateral side of 5th digit in 83%.[1] Overlaps with S2 |
| S2 | At the midpoint of the popliteal fossa. | |
| S3 | Over the tuberosity of the ischium or infragluteal fold | |
| S4 and S5 | In the perianal area, less than one cm lateral to the mucocutaneous zone | |
| V1 | ||
| V2 | ||
| V3 |
Videos
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Nitta et al.. Study on dermatomes by means of selective lumbar spinal nerve block. Spine 1993. 18:1782-6. PMID: 8235861. DOI.
- ↑ 2.0 2.1 Lee et al.. An evidence-based approach to human dermatomes. Clinical anatomy (New York, N.Y.) 2008. 21:363-73. PMID: 18470936. DOI.
- ↑ Furman & Johnson. Induced lumbosacral radicular symptom referral patterns: a descriptive study. The spine journal : official journal of the North American Spine Society 2019. 19:163-170. PMID: 29800710. DOI.
- ↑ Downs & Laporte. Conflicting dermatome maps: educational and clinical implications. The Journal of orthopaedic and sports physical therapy 2011. 41:427-34. PMID: 21628826. DOI.
- ↑ Nitta et al.. Study on dermatomes by means of selective lumbar spinal nerve block. Spine 1993. 18:1782-6. PMID: 8235861. DOI.
- ↑ Denny-Brown & Kirk. Hyperesthesia from spinal and root lesions. Transactions of the American Neurological Association 1968. 93:116-20. PMID: 4974855.
- ↑ Moriishi et al.. The intersegmental anastomoses between spinal nerve roots. The Anatomical record 1989. 224:110-6. PMID: 2729613. DOI.
- ↑ 8.0 8.1 Pellerin et al.. The prefixed and postfixed brachial plexus: a review with surgical implications. Surgical and radiologic anatomy : SRA 2010. 32:251-60. PMID: 20087592. DOI.
- ↑ Du Plessis et al.. Differentiation and classification of thoracolumbar transitional vertebrae. Journal of anatomy 2018. 232:850-856. PMID: 29363131. DOI. Full Text.
- ↑ Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Edinburgh: Elsevier/Churchill Livingstone, 2012
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,