Ganglion Impar Injection
| Ganglion Impar Injection | |
|---|---|
| Indication | Coccydynia, chronic prostatitis, chronic proctitis, pelvic malignancies, and chronic perineal pain |
| Syringe | 10mL |
| Needle | Transsacrococcygeal: 38mm 23g needle. Or 25-gauge 50mm needle inserted through a 22-gauge 38mm needle (needle inside needle) |
| Steroid | 40mg optional |
| Local | 1% lidocaine or 0.25% bupivacaine |
| Volume | 3-5mL of 1% lidocaine for a diagnostic block, or 10mL of 0.25% bupivacaine +/- 40mg of methylprednisolone for treatment. |
Injection treatment of the ganglion impar with local anaesthetic with or without corticosteroid is a procedure to treat Coccydynia, chronic perineal pain, and other conditions. Needle placement is generally done by piercing through the sacrococcygeal disc space. A single injection can provide long lasting relief of pain.
Radiofrequency treatments such as pulsed radiofrequency is a newer technique and may provide better results than blockade.[1]
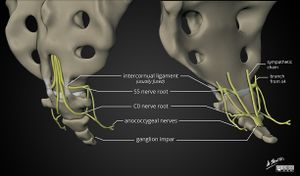
Anatomy
- Main article: Coccyx Anatomy
The ganglion impair is a midline sympathetic ganglion anterior to the upper coccyx, formed by the caudal termination of paired sympathetic chains. The ganglion provides both sympathetic and visceral innervation to the coccyx, perineum, and anal regions. The size and location can vary, and in some people the ventral ramus of the sacral nerve roots run close by. It is classically at the level of the sacrococcygeal junction.
Indications
Recalcitrant Coccydynia, chronic prostatitis, chronic proctitis, pelvic malignancies, and chronic perineal pain
Contraindications
Pregnancy if performing under ionising radiation and fluoroscopy.
Technique
There are two general techniques. The older trans-anococcygeal ligament approach, and the transsacrococcygeal/trans-discal approach.
- Trans-anococcygeal ligament approach
A curved needle is inserted through the midline anococcygeal ligament, and then advanced to the ventral coccyx at the midline concavity.
- Trans-sacrococcygeal / Trans-discal approach
In this technique the needle is inserted through the sacrococcygeal joint, but insertion through the intercoccygeal joints has also been described. The optimum technique uses a combination of ultrasound and fluoroscopy. Ultrasound uses loss of resistance as the modality can't alone accurately assess needle depth, while fluroscopy alone cannot accurately identify the sacrococcygeal junction nor its angulation due to bowel gas. In the combined technique the needle is first inserted under ultrasound guidance, and then the depth verified by fluoroscopy. This provides optimum accuracy and safety.[2] The sacrococcygeal joint or overlying ligament may become ossified with age.
A needle inside needle technique had been described. This uses an initial 22-gauge 38mm needle inserted through the sacrococcygeal junction. A 25-gauge 50mm needle is placed through the 22 gauge needle. This approach is theorised to reduce the risk of discitis and reduce the risk of needle breakage. Needle breakage risk may be reduced from using a shorter needle. Withdrawal of the 25-gauge needle at the end of the procedure decreases the risk that further injectate will spill into the surrounding tissues and disc. This may reduce the risk of discitis and fistula formation. Flushing the needle with preservative free saline and re-styleting the needle may also reduce percutaneous injectate spillage.
Ultrasound Guided Trans-sacrococcygeal Injection
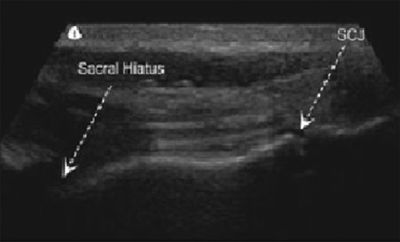
Ultrasound guided techniques have been described such as by Ghai et Al.[3] Loss of resistance is used and this appears to be patient and operator dependent.
- Position: prone, lower limbs internally rotated, toes pointing to the opposite foot. Optional pillow under the abdomen to reduce lumbar lordosis. This all helps to separate the buttocks and provide a flatter sacral hiatus site.
- Place the transducer in the transverse position and visualise the sacral hiatus, the two sacral cornuae, and the sacrococcygeal ligament which traverses the sacral hiatus above the epidural space
- Obtain a longitudinal position of the sacral hiatus, the proximal portion of the transducer resting between the two cranial sacral cornuae. The first cleft caudal to the sacral hiatus is the sacrococcygeal junction.
- Confirm the location of the sacrococcygeal junction by pressing with a long forceps under sonographic monitoring.
- Anaesthetised the overlying skin
- Needle advancement
- Advance a 23 gauge needle through the sacrococcygeal junction using an out of plane technique.
- Advance the needle until a loss of resistance is felt, which indicates that the needle tip is ventral to the sacrococcygeal ligament. Note that this is not always felt, hence the ideal use of combined imaging with fluoroscopy to confirm needle depth. Ultrasound cannot visualise the ventral coccyx
- Inject 3-5mL of 1% lidocaine or 10mL of 0.25% bupivacaine and 40mg of methylprednisolone.
Fluoroscopic Guidance
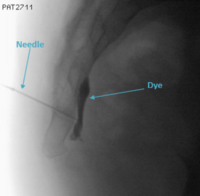
A true lateral fluoroscopic image is obtained by superimposing the two greater sciatic notches.
- Transsacrococcygeal Technique
This is the preferred method
- Original Plancarte Technique
Uses a per rectal finger during the injection.
- Paramedian Approach
Using a curved needle
Non-ultrasound Guided
This is not recommended
Neurolysis
In the event of a positive diagnostic block, neurolysis can be performed. A neurolytic agent such as 99% alcohol is injected on both sides, 20 to 30 minutes after the diagnostic block. If the patient complains of pain at any time during injection then abort the procedure immediately.[4]
Radioiofrequency lesioning
Bipolar strip lesioning is done at 70 to 80 degrees C for 90 seconds.
Complications
- General: Neuritis, inadvertant injection into the rectum, infection (including discitis), fistula formation.
- Trans-anococcygeal: rectal perforation, bleeding due to the longer needle course.
- Trans-sacrococcygeal: Increased risk of discitis and needle breakage which may be reduced by the needle through needle technique.
Aftercare
May be repeated with a long acting anaesthetic of successful, or neurolysis can be done.
After injection of a neurolytic agent, it is imperative that the patient has absolute bed rest for 3 to 4 hours without change of position. This is to prevent spread of the neurolytic agent to adjacent structures.[4]
Videos
See Also
External Links
References
- ↑ 1.0 1.1 Sir & Eksert. Comparison of block and pulsed radiofrequency of the ganglion impar in coccygodynia. Turkish journal of medical sciences 2019. 49:1555-1559. PMID: 31652036. DOI. Full Text.
- ↑ Lin et al.. Ultrasound-guided ganglion impar block: a technical report. Pain medicine (Malden, Mass.) 2010. 11:390-4. PMID: 20447308. DOI.
- ↑ 3.0 3.1 Ghai et al.. A prospective study to evaluate the efficacy of ultrasound-guided ganglion impar block in patients with chronic perineal pain. Saudi journal of anaesthesia 2019. 13:126-130. PMID: 31007658. DOI. Full Text.
- ↑ 4.0 4.1 Practical Management of Pain. 5th edition. 2014
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,