Hip Osteoarthritis
Hip osteoarthritis is a degenerative joint disease, and is the second most common joint affected by osteoarthritis after the knee. The condition imposes an increasing burden on the healthcare system, yet research has not kept pace with knee specific research. Clinical guidelines for hip osteoarthritis tend to extrapolate from knee osteoarthritis research, despite these conditions being distinct.
Epidemiology
A US study of mostly Caucasian people aged over 50, the prevalence of radiographic hip OA was 19.6%, and the prevalence of symptomatic disease was 4.2%, with the prevalence increasing with higher age. The authors found a male predominance of symptomatic OA, especially in older individuals, unlike other studies which have found a female predominance. There is generally a male predominance of radiographic OA.[1] A Japanese study found the prevalence of radiographic hip osteoarthritis to be 18.2% in men and 14.3% in women[2] Overall the relationship between sex and hip OA isn't clear.[3]
The prevalence of hip OA in patients with hip and/or groin pain presenting to primary care is 35%.[4]
| Radiographic Hip OA | Symptomatic Hip OA | |
|---|---|---|
| Men (n=434) | 24.7% (20.6%-28.7%) | 5.2% (3.3%-7.8%) |
| Women (n=544) | 13.6% (10.7%-16.5%) | 3.0% (1.7%-4.8%) |
| Age 50-59 (n=390) | 14.6% (11.1%-18.1%) | 3.4% (1.8%-5.8%) |
| Age 60-69 (n=337) | 16.6% (12.6%-20.6%) | 2.7% (1.3%-5.1%) |
| Age 70-79 (n=197) | 25.9% (19.8%-32.0%) | 6.3% (3.3%-10.7%) |
| Age ≥ 80 (n=54) | 31.5% (19.1%-43.9%) | 7.4% (0.2%-17.9%) |
| Crude Prevalence | 18.5% (16.1%-20.9%) | 4.0% (2.8%-5.4%) |
| Age-standardized Prevalence | 19.6% (16.7%-23.0%) | 4.2% (2.9%-6.1%) |
Aetiology and Risk Factors
Hip osteoarthritis is usually caused by a series of different risk factors which can be categorised into those at the joint level and whole person level.[3] The risk factors lead to instability, malalignment, increased joint load, and microtrauma, which subsequently leads to disruption of the homeostatic equilibrium between joint synthesis and degradation, resulting in a final common pathway of osteoarthritic change.
There are several structures around the hip that are richly innervated by sensory nerve fibres. These include the periosteum, subchondral bone, synovium, and surrounding soft tissues. In the presence of Central Sensitisation there may be an additional central physiological process. Hip osteoarthritis can also lead to changes in gait which can lead to pain in the knees and lumbar spine.[4]
Joint Level Risk Factors
Abnormal joint morphology is the most important risk factor. This includes the cam form of Femoroacetabular Impingement (FAI) and the less common Developmental Dysplasia of the Hip (DDH), which are both associated with early-onset OA. One proposition is that abnormal joint morphology exists on a spectrum, with more subtle abnormalities being associated with late-onset or "primary" OA.[3]
Developmental Dysplasia of the Hip
- Main article: Developmental Dysplasia of the Hip
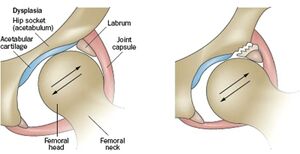
Abnormal joint morphology causes abnormal loading on the joint and accelerates articular degeneration. In DDH, a shallow and often maloriented acetabulum with excessive anteversion causes decreased femoroacetabular contact surface area, subluxation of the femoral head, and greatly increased load onto the joint. The distribution of shear forces are most commonly directed anterosuperiorly onto the acetabular rim, and this results in labral and cartilage damage. More severe forms of DDH result in whole joint failure early in life, while in milder dysplasia this can occur later.[3]
Femoroacetabular Impingement
- Main article: Femoroacetabular Impingement

FAI is probably a more common cause of the development of hip OA, however FAI is also common in asymptomatic individuals and so it is not a sufficient cause.
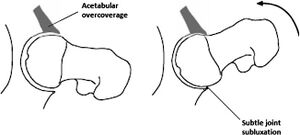
There are two patterns, cam and pincer, as well as a combination of both types. In cam FAI there is a thickened, aspherical femoral head-neck junction, which abuts against the anterosuperior labrum with hip flexion, and results in compression of the labrum and acetabular cartilage. This leads to separation of the labrum from the acetabular cartilage and delamination of the acetabular cartilage from the subchondral bone.
In pincer FAI, there is an overcoverage of the acetabulum with a deepened acetabular on the femoral head. The femoral neck abuts against the acetabular labrum and compresses it, damaging both the labrum and underlying cartilage. Lesions usually occur anterosuperiorly from hip flexion like with cam lesions, but also posteroinferiorly from posterior subluxation due to continued flexion causing a contre-coup lesion.[3]
The CHECK study assessed 1002 patients aged 45–65 years with early symptoms of hip OA but without definite radiographic evidence of the same over 5 years. At baseline, 76% of the included hips had no radiographic signs of osteoarthritis and 24% doubtful osteoarthritis. Cam deformities and acetabular dysplasia were shown to be associated with an increased odds ratio for progression to early onset osteoarthritis.[5] While pincer changes were actually associated with a reduced risk.[6]
Muscle Dysfunction
Another possible risk factors that warrants further study is muscle dysfunction of the deep hip stabilisers, which is commonly found in FAI. The deep stabilising muscles may play a role in shock absorption. Muscle weakness may be due to pain inhibition, muscle disuse atrophy, or aberrant joint mechanics.[3]
Joint Injury and Labral Tears
Joint injury is well-established as a risk factor for OA development in other joints, such as ACL tears in knee osteoarthritis. Labral tears are associated with chondral damage and it is thought that they may contribute to the development of osteoarthritis. However isolated labral tears are very common in the asymptomatic population and this area needs further study.[3]
Whole Person Risk Factors
These include age, sex, weight, genetics, ethnicity, and occupation. There is no high-quality evidence that implicate any dietary risk factors.[3]
Age and Sex
Age and sex has been discussed in the epidemiology section. In short, the risk increases with age, and the relationship between sex and hip OA isn't clear.
Weight
Increased weight is associated with an increased risk of hip OA, but with a less marked relationship than with knee OA. There are two proposed mechanisms for weight being a risk factor. One possible cause is increased biomechanical loading on the joint. Another cause is the metabolic theory, where the development of OA is spurred on by pro-inflammatory factors. This theory is supported by the fact that there is a relationship between obesity and OA in the non-weight bearing hand.[3]
Genetics
Genetic factors account for around 60% of hip OA risk, with several candidate genes being identified, often related to synovial joint development. This may be related to the spectrum model of hip joint morphology abnormalities.[3]
Ethnicity
There is marked variation of hip OA development between different ethnicities. hip OA is 80-90% less prevalent in Chinese than USA Caucasians. A postulated cause is differences in joint morphology, with Caucasians having higher rates of femoral head asphericity and pincer impingement morphology. There may be genetic factors at play.[3]
Occupation
Occupations that require heavy manual work confers an increased risk of hip OA development. Farming is a particularly strong risk factor, with a three fold greater relative risk. Athletes may be predisposed to hip OA. This may be due to joint injury, increased load, and a higher prevalence of cam morphology (due to high levels of physical activity in adolescence). In the general population there is no good evidence that exercise is a risk factor for hip OA, and joint loading is required for joint homeostasis.[3]
Clinical Features
- Sudden onset of acute pain
- Trauma
- Pain not improved by rest
- Pain so severe that weight bearing isn't possible
History
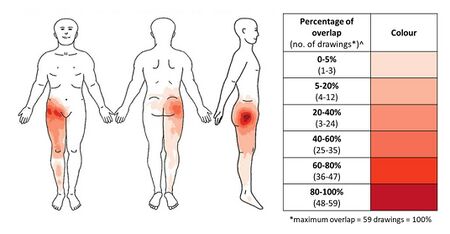
The pain is often poorly localised. Patients can have pain over quite a large area. In a study of 109 patients, pain was present in the greater trochanter (77%), groin (53%), anterior/lateral thigh (42%), buttock (38%), knee (17%), and lower leg (15%). Less than 20% had pain in only one area, most commonly the greater trochanter. [7]
Patients with neural sensitisation can have unusual distributions of pain at a surprising distance from the hip such as below the knee.
There is no clear association between pain levels and radiographic severity of hip osteoarthritis. Up to 40% of patients with hip osteoarthritis have no pain. Patients with higher pain levels showed differences in sensitisation as measured by quantitative sensory testing.[8]
None of the features on history are particularly helpful on their own for identifying hip OA. Medial thigh pain is highly suggestive of hip OA but is only present in 2.7% of patients. The presence of morning stiffness, pain on walking, and relief of pain on sitting all have positive likelihood ratios of <2.0, but their negative likelihood ratios are more helpful, i.e. the absence of these factors.[4]
| Feature on History | Sensitivity | Specificity | LR+ (95% CI) | LR- (95% CI) |
|---|---|---|---|---|
| Family history of OA | 34% | 84% | 2.1 (1.2-3.6) |
0.79 (0.67-0.93) |
| Personal history of knee OA | 33% | 84% | 2.1 (1.1-3.8) |
0.80 (0.68-0.95) |
| Age > 60 | 96% | 25% | 1.5 (1.3-1.7) |
0.11 (0.02-0.78] |
| Age < 50 | 91% | 28% | 1.3 (1.1-1.5) |
0.32 (0.16-0.62) |
| Worst pain in medial thigh | 12% | 98% | 7.8 (1.7-37) |
0.89 (0.77-1.0) |
| Worst pain in buttock | 12-67% | 57-69% | 0.38-2.0 | 0.38-0.76 |
| Pain on climbing stairs or walking down slopes | 68% | 68% | 2.1 (1.6-2.8) |
0.47 (0.35-0.63) |
| Morning stiffness <60 min | 56-91% | 41-67% | 1.5-1.7 | 0.22-0.65 |
| Pain on initial steps after rest | 92% | 26% | 1.2 (1.1-1.4) |
0.31 (0.08-1.2) |
| Pain on walking | 80-97% | 12-34% | 1.1-1.2 | 0.25-0.58 |
| Pain relieved by sitting | 92% | 33% | 1.4 (0.2-1.6) |
0.24 (0.06-0.92) |
Examination
- Main article: Hip Examination
Physical examination findings are in general more useful than historical features for identifying hip OA. Posterior hip pain with squat is the test with the highest likelihood ratio, but some patients may not be very excited about trying this. Groin pain on hip abduction or adduction, abductor weakness, decreased hip adduction, and decreased hip internal rotation are all findings with positive likelihood ratios above 3. For identifying those who do not have hip OA, normal hip passive adduction or abduction are the most helpful.[4]
Extension is examined with the patient prone and lifting the leg off the table. Flexion is examined with the patient supine, and the examiner lifts the knee to the abdomen. In this position the foot can be kept in the same position, and the knee moved towards the midline, causing internal rotation. The hip can then be moved away from the midline, which causes external rotation. Adduction and abduction are assessed by putting the feet together. The foot is then moved across or away from the midline respectively. Normal ranges of motion are below. Goniometers are sometimes used, but usually estimates are sufficient. The examiner should compare range to the other side, but keeping in mind that osteoarthritis is often bilateral.[4]
| Passive Movement | Normal ROM |
|---|---|
| Flexion | 0 - 140° |
| Internal rotation | 0 - 30° |
| External rotation | 0 - 40° |
| Abduction | 0 - 50° |
| Adduction | 0 - 30° |
| Extension | 0 - 20° |
| Feature on Exam | Sensitivity | Specificity | LR+ (95% CI) | LR-(95% CI) |
|---|---|---|---|---|
| Abductor weakness | 44 | 90 | 4.5
(2.4-8.4) |
0.62
(0.43-0.88) |
| Limp | 85 | 43 | 1.5
(1.2-1.9) |
0.35
(0.20-0.61) |
| Inguinal ligament tenderness | 60 | 75 | 2.4
(1.6-3.8) |
0.53
(0.33-0.87) |
| Tensor fascia lata tenderness | 40 | 80 | 2.0
(1.1-3.4) |
0.75
(0.54-1.1) |
| Squat causing posterior pain | 24 | 96 | 6.1
(1.3-29) |
0.79
(0.62-1.0) |
| Groin pain on abduction or adduction | 33 | 94 | 5.7
(1.6-20) |
0.71
(0.52-0.97) |
| Scour test | 62 | 74 | 2.4
(1.4-4.3) |
0.51
(0.29-0.90) |
| Pain on hip adduction | 68-80 | 46-54 | 1.5 - 1.5 | 0.43-0.59 |
| Pain on hip internal rotation | 82-88 | 38-39 | 1.4 - 1.4 | 0.31-0.45 |
| Restricted movement in 3 planes | NA | NA | 4.4
(2.4-8.3) |
NA |
| Restricted movement in 2 planes | NA | NA | 1.5
(0.90-2.6) |
NA |
| Restricted movement in 1 plane | NA | NA | 1.3
(0.85-2.0) |
NA |
| Restricted movement in 0 planes | NA | NA | 0.91
(0.78-1.1) |
NA |
| Decreased hip adduction | 80 | 81 | 4.2
(3.0-6.0) |
0.25
(0.11-0.54) |
| Decreased hip internal rotation | 66 | 79 | 3.2
(1.7-6.0) |
0.43
(0.31-0.60) |
| Decreased hip range of movement | 75 | 74 | 2.9
(2.1-4.0) |
0.34
(0.25-0.47) |
| Decreased hip extension | 76 | 68 | 2.4
(1.8-3.2) |
0.35
(0.17-0.71) |
| Decreased hip external rotation | 76 | 64 | 2.1
(1.6-2.8) |
0.37
(0.19-0.76) |
| Decreased hip abduction | 88 | 46 | 1.6
(1.3-2.1) |
0.26
(0.09-0.77) |
Combinations of findings have also been studied.
| Findings | Number of findings | LR+ (95% CI) |
|---|---|---|
|
5 or more | 35 (13-95) |
| 4 | 2.0 (0.88-4.3) | |
| 3 or fewer | 0.05 (0.01-0.32) | |
|
4 or more | 4.9 (2.8-8.7) |
| 2-3 | 0.72 (0.57-0.93) | |
| 0 or 1 | 0.24 (0.09-0.64) |
Investigations
Imaging
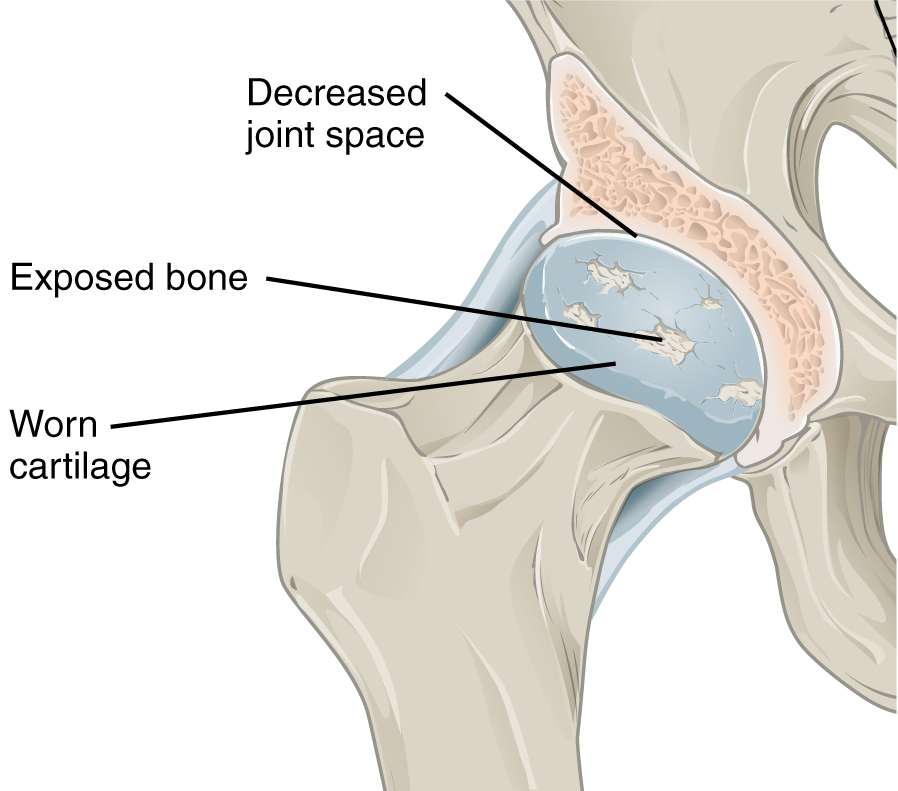
Plain radiographs can demonstrate joint space narrowing, osteophytes, subchondral sclerosis, and subchondral cysts. They may also show alternative causes for pain such as pelvic bone tumours. The Kellgren and Lawrence classification is most commonly used to assess OA severity, however this system relies on the presence of osteophytes, which doesn't correlate well to pain.
- Grade 1, doubtful OA with possible joint space narrowing medially and subtle osteophyte formation around the femoral head.
- Grade 2, mild OA with definite joint space narrowing inferiorly with definite osteophyte formation and slight subchondral sclerosis.
- Grade 3, moderate OA with marked narrowing of the joint space, small osteophytes, some sclerosis and cyst formation, and deformity of the femoral head and acetabulum.
- Grade 4, obliterated joint space with features seen in grades 1 to 3, large osteophytes, and gross deformity of the femoral head and acetabulum.
See Radiopaedia for a collection of x-ray cases.
MRI is more specific, and much more sensitive for detecting hip osteoarthritis than plain films, and can also visualise the labrum, cartilage, bone marrow, ligaments, and synovium. It also visualises other possible causes of pain such as gluteal tendinopathy.
Ultrasound is useful for detecting effusions and synovitis, and can also be used for guided injections.
CT can be used for surgical planning.
Laboratory Tests
Depending on the clinical context, rheumatological blood tests may need to be performed.
Diagnostic Injection
A significant minority of patients are a diagnostic dilemma due to clinical and radiographic features that could be consistent with alternative causes of pain (especially spinal). In these cases, a commonly performed procedure in Musculoskeletal Medicine in New Zealand is the diagnostic intra-articular hip joint injection. Under either ultrasound or fluoroscopic guidance, local anaesthetic is infiltrated into the hip joint. An appreciable reduction in pain post-procedure is consistent with nociception arising from the hip joint. A long acting or combination of short and long acting anaesthetic is usually used, to allow the patient ample time to test out provocative movements and positions.
This practice is well supported by the literature and predicts response to total hip arthroplasty to a very high degree. The main limitation to these studies is that patients with a negative response didn't tend to have surgery (as you'd expect), and so we only really can comment on the sensitivity (TP / TP + FN), rather than the specificity (TN / TN + FP). The true negative rate is not well known: we don't know whether we are completely excluding the possibility of response to surgery with a negative injection. The studies have tended to call true negatives those that improved with treatment of the alternative cause of pain (usually spinal), or not commented at all.
| Study | Injectate (+/- contrast) | Image Guidance | Cut-off | Number | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Crawford et al 1998[9] | 10mL Bupivacaine 0.5% | Fluoroscopy | Not clear | 42 | 87-100% | 80-100% |
| Faraj et al 2003[10] | bupivacaine 0.5%
+/- triamcinolone |
Fluoroscpy | Complete or "significant" relief of pain | 47 | 88% | 100% |
| Illgen et al 2006[11] | 3.5mL lidocaine 2%
3.5mL bupivacaine 0.5% |
Fluoroscopy | >50% relief of pain | 34 | 95.2% | 87.5% |
| Pateder et al 2007[12] | 9mL lidocaine 1%
40mg triamcinolone |
Fluoroscopy | Unable to access full article | 83 | 100% | 81% |
| Ashock et al 2009[13] | Up to 10mL bupivacaine 0.5% | Fluoroscopy | >70% relief of pain | 48 | 97% | 91% |
| Deshmukh et al 2010[14] | 5mL bupivacaine 0.5% 80mg methylprednisolone |
Fluoroscopy | >50% pain relief after 30 minutes Or delayed response within 2 weeks |
204 | 91.5% | 100% |
| Yoong et al 2012[15] | Up to 10mL bupivacaine 0.25% | Ultrasound | Complete relief of pain | 138 | 91.5% | 91.5% |
It is suggested to avoid co-injection of corticosteroid if total hip arthroplasty is being considered due to the risk of deep infection.
Diagnosis
The diagnosis can be made clinically in those with mild to moderate symptoms, with examination findings being more useful than historical factors. In those with more severe symptoms then plain radiographs are performed. If the radiographs are normal then there should be a search for other causes of pain.
Plain radiographs are cheap, however because most patients with radiographic OA have asymptomatic disease, there is a risk of incorrectly attributing the pain to osteoarthritis, and subsequently having incorrect treatment. Therefore it is as important as ever to consider the pre-test probability, and consider other diagnoses.
In cases where the diagnosis is uncertain, a positive response to a diagnostic intra-articular local anaesthetic injection lends credence to the diagnosis. In the authors experience, hip surgeons in New Zealand may not to consider buttock dominant pain to consistent with hip osteoarthritis, and so a positive diagnostic injection may support the decision to have total hip arthroplasty in atypical cases.
Differential Diagnosis
- Anterior pain
- Hip Osteoarthritis
- Femoroacetabular Impingement
- Iliopsoas Tendionopathy
- Inflammatory arthritis
- Avascular necrosis/osteonecrosis of the femoral head
- Hip Labral Tear
- Nerve Entrapments: Genitofemoral Nerve Entrapment, Ilioinguinal Nerve Entrapment
- Developmental Dysplasia of the Hip
- Transient Osteoporosis of the Hip
- Inguinal or femoral hernia
- Gynaecological causes
- Gonadal tumours
- Inguinal lymphadenopathy
- Posterior pain
- Lateral pain
- Medial pain
- Other
- Septic Arthritis
- Hip Fracture
- Hip chondral defects
- Ligamentum teres injury
- Pelvic bone tumours
- Pelvic insufficiency fractures
- Stress fracture
- Peripheral Vascular Disease
- Fibromyalgia
- Leaking abdominal aortic aneurysm
Treatment
Research into hip OA has lagged far behind knee OA, and treatment recommendations for hip OA are often extrapolated from knee OA.
Non-pharmacological
Education, exercise, and weight loss are the mainstays of non-pharmacological management of hip and knee osteoarthritis. However long-term compliance is generally challenging, [16] and there appears to be less benefit than for knee OA.[3]
Some exercise options include aerobic exercise, flexibility exercises, strengthening exercises, water-based exercises, and tai chi. Exercise results in a modest reduction in pain (8 points more than control in a 0-100 scale) and improvement of function (7 points more than control in a 24 point scale).[17] Water-based exercises may be helpful for those with particularly severe symptoms that limit engagement with land-based exercises.
The current evidence does not support physiotherapy as being more effective than home-exercises.[18]
The recommendation for weight loss has been extrapolated from knee osteoarthritis and the fact that obesity is a known risk factor for hip osteoarthritis.[19] There are no data on weight loss specifically for reducing symptoms of hip osteoarthritis.
Medication
NSAIDs are effective for managing hip osteoarthritis, with greater effect with higher doses. Diclofenac 150mg/day is the most effective NSAID available.[20] However, the safety profile needs to be considered for the patient in question, and the lowest dose and shortest duration possible should be used in those with considerable symptoms and poor response to nonpharmacological treatments.
There is no evidence to support single-agent paracetamol.[20]
In a landmark study, opioids were not superior to treatment with nonopioid medications in a study of patients with severe chronic back pain, hip OA, or knee OA.[21] Due to both poor efficacy and safety concerns, opioids should not generally be used for hip osteoarthritis.
Injections
- Main article: Hip Joint Injection
There are a variety of injection options which can can be done under ultrasound or fluoroscopic guidance. Ultrasound is preferred over fluoroscopy due to it causing less pain, being more convenient, and being cheaper.[22]
Steroid: Steroid injections for hip osteoarthritis is controversial, but may be an option for short term partial relief of pain in those unsuitable for surgery or those who wish to delay surgery.
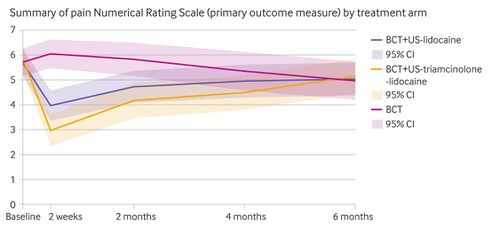
A 2016 meta-analysis of five small trials found that they confer a moderate short term effect for up to 8 weeks and are generally well tolerated.[24] The HIT trial was a 2022 three arm single blind RCT of 199 adults with at least moderate hip osteoarthritis that compared advice and education (best current treatment - BCT), with BCT plus ultrasound guided steroid (40mg triamcinolone) and lidocaine injection, and with BCT plus ultrasound guided lidocaine injection. The steroid group was superior but most benefits occurred within two months for pain and function and four months for function only, with no differences at six months. The proportion that reported being completely recovered or much better at two months for the steroid group vs the BCT group was 56% vs 0% at two weeks, 45% vs 7% at two months, 27% vs 17% at four months, and 22% vs 22% at six months. The presence of synovitis or effusion was associated with favouring the steroid group.[23]
Another RCT of 107 patients found that intramuscular steroid (40mg triamcinolone) was superior to placebo injection (difference difference −1.3, 95% CI −2.3 to −0.3) with the benefit persisting for the entire 12 week follow up period.[25] This is not routinely done due to concern about systemic side effects.
There have been concerns of causing rapid progression of osteoarthritis and infection following arthroplasty.
- One study found an alarming odds ratio of 8.5 for rapidly destructive hip disease with a dose-response curve. The overall rate was 5.4%, and occurred on average 5 months following injection. Rapidly destructive hip disease is characterised by rapidly progressive joint-space narrowing, osteolysis, and collapse of the femoral head.[26]
- One retrospective study of patients who had total hip arthroplasty found an alarming deep infection rate of 10% in 40 patients who had a previous steroid injection compared to no infections in 40 matched controls. The overall revision rate was also much higher at 12.5% vs 1.02%. The study was underpowered for looking at the time interval between injection and surgery.[27]
PRP: The evidence does not support the use of platelet-rich plasma injections.[28] In recalcitrant disease with the next step being surgery, the author will offer PRP injections into both the hip joint and gluteal tendons, but appreciating that the evidence is poor.
Hyaluronic acid: Intra-articular hyaluronic acid injections are no more effective than placebo. The cost of one vial of hyaluronic acid in New Zealand is around $500, and so this treatment has extremely poor cost-effectiveness.[29][30]
Saline: Saline appears to be as effective as other options. One systematic review and meta-analysis evaluated saline, glucocorticoids, hyaluronic acid, and PRP, and found that all (except HA+PRP) led to a clinically important improvement in pain.[31]
Surgery
Total hip joint replacement is usually effective for reducing pain. However 10% of patients have chronic postsurgical pain, and preoperative central sensitisation has been thought to be a risk factor for this.[8]Aseptic loosening accounts for about half of revisions. This presents as thigh or groin pain, and can be diagnosed on plain films.
The lifetime risk of undergoing a total hip replacement continues to grow. In the UK between 1991 and 2006 the lifetime risk rose from 4% to 11%.[32] It is surprising that despite the lack of placebo controlled trials, we spent an increasing amount of money on this procedure.
Longevity of impacts are typically good. Revision rates are 0.5% per year for the first 20 years. There are slight increases of revision rates in younger more active patients. At 15 years over 90% of patients are pain-free. Almost 60% of hip replacements last 25 years.[33]
Abnormal joint morphology may be the most important risk factor for development of OA. Surgical alteration of joint shape is sometimes used early in the disease course of FAI, as it appears that this confers a greater benefit than waiting until the development until advanced OA. It is not known whether asymptomatic but radiologically severe FAI should have surgical intervention.[3] At the point of the development of osteoarthritis, there may not be any benefit in head morphology alteration surgery, and if surgery is required these patients are generally offered hip arthroplasty.
Hip resurfacing procedures have a high rate of revision surgery compared to total hip arthroplasty. This procedure is probably only suitable in very carefully selected patients. Good prognostic factors are being young, active, male, having primary OA, and a sufficiently large femoral head size.
Prognosis
A minority have clear cut clinical and radiological recovery, especially with marked osteophytosis and concentric disease. Superolateral migration of the femoral head is correlated with more rapid osteoarthritis progression, also with atrophic bone response
Resources
- Dieppe PA is a good author to read
Summary
- The diagnosis of hip osteoarthritis is usually straightforward but examination findings are more useful than historical features for diagnosis.[Level 2]
- In cases where there is a diagnostic dilemma, a positive response (>70% relief of pain) to an intra-articular local anaesthetic hip joint injection supports the diagnosis and response to total hip arthroplasty.[Level 2]
- Saline, corticosteroid, PRP, and hyaluronic acid all seem to be equally effective for obtaining a moderate reduction in pain for up to 8 weeks. Steroid injections should be avoided if total hip arthroplasty is being considered.[Level 2]
- Total hip arthroplasty is an effective treatment for those with severe symptoms and inadequate response to non-surgical treatments.[Level 3]
References
- ↑ 1.0 1.1 Kim et al.. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis & rheumatology (Hoboken, N.J.) 2014. 66:3013-7. PMID: 25103598. DOI. Full Text.
- ↑ Iidaka et al.. Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthritis and cartilage 2016. 24:117-23. PMID: 26241774. DOI.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Murphy et al.. Hip Osteoarthritis: Etiopathogenesis and Implications for Management. Advances in therapy 2016. 33:1921-1946. PMID: 27671326. DOI. Full Text.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Metcalfe et al.. Does This Patient Have Hip Osteoarthritis?: The Rational Clinical Examination Systematic Review. JAMA 2019. 322:2323-2333. PMID: 31846019. DOI. Full Text.
- ↑ Agricola et al.. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Annals of the rheumatic diseases 2013. 72:918-23. PMID: 22730371. DOI.
- ↑ Agricola et al.. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis and cartilage 2013. 21:1514-21. PMID: 23850552. DOI.
- ↑ 7.0 7.1 Poulsen, E.; Overgaard, S.; Vestergaard, J.T.; Christensen, H.W.; Hartvigsen, J. (2015-04). "Pain distribution in primary care patients with hip osteoarthritis – A descriptive study". Osteoarthritis and Cartilage. 23: A334–A335. doi:10.1016/j.joca.2015.02.610. ISSN 1063-4584. Check date values in:
|date=(help) - ↑ 8.0 8.1 Hattori T, Shimo K, Niwa Y, Tokiwa Y, Matsubara T. Association of Chronic Pain with Radiologic Severity and Central Sensitization in Hip Osteoarthritis Patients. J Pain Res. 2021;14:1153-1160 DOI
- ↑ Crawford et al.. Diagnostic value of intra-articular anaesthetic in primary osteoarthritis of the hip. The Journal of bone and joint surgery. British volume 1998. 80:279-81. PMID: 9546460. DOI.
- ↑ Faraj et al.. Intra-articular bupivacaine hip injection in differentiation of coxarthrosis from referred thigh pain: a 10 year study. Acta orthopaedica Belgica 2003. 69:518-21. PMID: 14748108.
- ↑ Illgen et al.. The diagnostic and predictive value of hip anesthetic arthrograms in selected patients before total hip arthroplasty. The Journal of arthroplasty 2006. 21:724-30. PMID: 16877160. DOI.
- ↑ Pateder & Hungerford. Use of fluoroscopically guided intra-articular hip injection in differentiating the pain source in concomitant hip and lumbar spine arthritis. American journal of orthopedics (Belle Mead, N.J.) 2007. 36:591-3. PMID: 18075606.
- ↑ Ashok, N., Sivan, M., Tafazal, S. et al. The diagnostic value of anaesthetic hip injection in differentiating between hip and spinal pain. Eur J Orthop Surg Traumatol 19, 167–171 (2009). DOI
- ↑ Deshmukh et al.. Accuracy of diagnostic injection in differentiating source of atypical hip pain. The Journal of arthroplasty 2010. 25:129-33. PMID: 20570105. DOI.
- ↑ Crawford et al.. Diagnostic value of intra-articular anaesthetic in primary osteoarthritis of the hip. The Journal of bone and joint surgery. British volume 1998. 80:279-81. PMID: 9546460. DOI.
- ↑ Gay et al.. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of physical and rehabilitation medicine 2016. 59:174-183. PMID: 27053003. DOI.
- ↑ Fransen et al.. Exercise for osteoarthritis of the hip. The Cochrane database of systematic reviews 2014. CD007912. PMID: 24756895. DOI.
- ↑ Bennell et al.. Physical therapies in the management of osteoarthritis: current state of the evidence. Current opinion in rheumatology 2015. 27:304-11. PMID: 25775185. DOI.
- ↑ Jiang et al.. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint bone spine 2011. 78:150-5. PMID: 20580591. DOI.
- ↑ 20.0 20.1 da Costa et al.. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet (London, England) 2017. 390:e21-e33. PMID: 28699595. DOI.
- ↑ Krebs et al.. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA 2018. 319:872-882. PMID: 29509867. DOI. Full Text.
- ↑ Byrd et al.. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2014. 30:42-6. PMID: 24384272. DOI.
- ↑ 23.0 23.1 Paskins, Zoe; Bromley, Kieran; Lewis, Martyn; Hughes, Gemma; Hughes, Emily; Hennings, Susie; Cherrington, Andrea; Hall, Alison; Holden, Melanie A.; Stevenson, Kay; Menon, Ajit (2022-04-06). "Clinical effectiveness of one ultrasound guided intra-articular corticosteroid and local anaesthetic injection in addition to advice and education for hip osteoarthritis (HIT trial): single blind, parallel group, three arm, randomised controlled trial". BMJ (Clinical research ed.). 377: e068446. doi:10.1136/bmj-2021-068446. ISSN 1756-1833. PMC 8984871. PMID 35387783.
- ↑ McCabe et al.. The efficacy of intra-articular steroids in hip osteoarthritis: a systematic review. Osteoarthritis and cartilage 2016. 24:1509-17. PMID: 27143362. DOI.
- ↑ Dorleijn, Desirée M. J.; Luijsterburg, Pim A. J.; Reijman, Max; Kloppenburg, Margreet; Verhaar, Jan A. N.; Bindels, Patrick J. E.; Bos, Pieter Koen; Bierma-Zeinstra, Sita M. A. (2018-06). "Intramuscular glucocorticoid injection versus placebo injection in hip osteoarthritis: a 12-week blinded randomised controlled trial". Annals of the Rheumatic Diseases. 77 (6): 875–882. doi:10.1136/annrheumdis-2017-212628. ISSN 1468-2060. PMID 29514801. Check date values in:
|date=(help) - ↑ Okike K, King RK, Merchant JC, Toney EA, Lee GY, Yoon HC. Rapidly Destructive Hip Disease Following Intra-Articular Corticosteroid Injection of the Hip. J Bone Joint Surg Am. 2021 Nov 17;103(22):2070-2079. doi: 10.2106/JBJS.20.02155. PMID: 34550909.
- ↑ Kaspar & de V de Beer. Infection in hip arthroplasty after previous injection of steroid. The Journal of bone and joint surgery. British volume 2005. 87:454-7. PMID: 15795191. DOI.
- ↑ Berney M, McCarroll P, Glynn L, Lenehan B. Platelet-rich plasma injections for hip osteoarthritis: a review of the evidence. Ir J Med Sci. 2021 Aug;190(3):1021-1025. doi: 10.1007/s11845-020-02388-z. Epub 2020 Oct 5. PMID: 33015749.
- ↑ Brander et al.. Evaluating the use of intra-articular injections as a treatment for painful hip osteoarthritis: a randomized, double-blind, multicenter, parallel-group study comparing a single 6-mL injection of hylan G-F 20 with saline. Osteoarthritis and cartilage 2019. 27:59-70. PMID: 30223023. DOI.
- ↑ Wu et al.. Efficacy of intra-articular hyaluronic acid injections in hip osteoarthritis: a meta-analysis of randomized controlled trials. Oncotarget 2017. 8:86865-86876. PMID: 29156841. DOI. Full Text.
- ↑ Gazendam et al.. Intra-articular saline injection is as effective as corticosteroids, platelet-rich plasma and hyaluronic acid for hip osteoarthritis pain: a systematic review and network meta-analysis of randomised controlled trials. British journal of sports medicine 2021. 55:256-261. PMID: 32829298. DOI.
- ↑ Culliford et al.. The lifetime risk of total hip and knee arthroplasty: results from the UK general practice research database. Osteoarthritis and cartilage 2012. 20:519-24. PMID: 22395038. DOI.
- ↑ Erens et al. Total hip arthroplasty In: Uptodate. Nov 5 2021.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,