Hypermobile Ehlers Danlos Syndrome: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{stub}} | |||
==Diagnostic Criteria== | ==Diagnostic Criteria== | ||
hEDS is a clinical spectrum from asymptomatic joint hypermobility, to “non syndromic” hypermobility, to hEDS. The latest diagnostic criteria for hEDS were published in 2017 <ref>Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8-26. doi:10.1002/ajmg.c.31552</ref> | hEDS is a clinical spectrum from asymptomatic joint hypermobility, to “non syndromic” hypermobility, to hEDS. The latest diagnostic criteria for hEDS were published in 2017 <ref>Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8-26. doi:10.1002/ajmg.c.31552</ref> | ||
Revision as of 21:10, 27 June 2020
Diagnostic Criteria
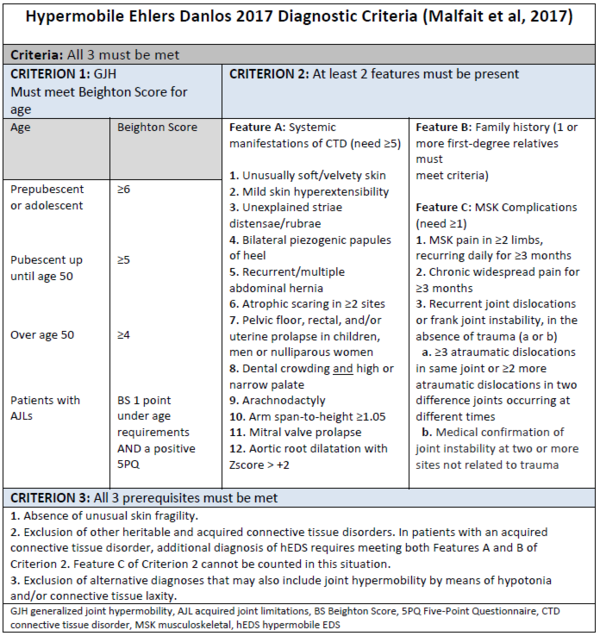
hEDS is a clinical spectrum from asymptomatic joint hypermobility, to “non syndromic” hypermobility, to hEDS. The latest diagnostic criteria for hEDS were published in 2017 [1]
Summary
Criterion 1: Generalised Joint Hypermobility
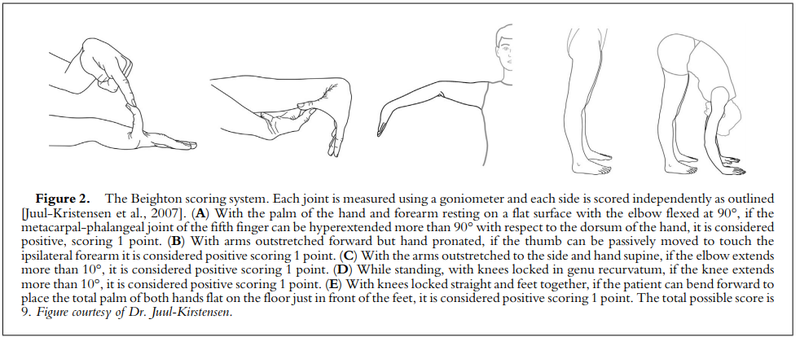
Must meet Beighton Score for age
| Age | Beighton Score |
| Prepubescent or adolescent | ≥6 |
| Pubescent up until age 50 | ≥5 |
| Over age 50 | ≥4 |
| Patients with Acquired joint limitations | BS 1 point under age requirements AND a positive 5PQ
|
| Five Point Questionnaire for identifying hypermobility (5PQ) |
| Criteria: Two or more “yes” answers suggest joint hypermobility. |
|
Criterion 2: At least 2 features must be present
Feature A: Systemic manifestations of CTD (need ≥5)'
- Unusually soft/velvety skin
- Mild skin hyperextensibility
- Unexplained striaedistensae/rubrae
- Bilateral piezogenic papules of heel
- Recurrent/multiple abdominal hernia
- Atrophic scaring in ≥2 sites
- Pelvic floor, rectal, and/or uterine prolapse in children, men or nulliparous women
- Dental crowding and high or narrow palate
- Arachnodactyly
- Arm span-to-height ≥1.05
- Mitral valve prolapse
- Aortic root dilatation with Z score > +2
Skin extensibility as measured by pinching and lifting the cutaneous and subcutaneous layers of the skin on the volar surface at the middle of the non-dominant forearm as described in Remvig et al, 2009. Skin extensibility of >1.5 cm is considered the upper end of normal. It is likely that the hyperextensibility of the skin in hEDS overlaps significantly with that of “normal” skin. Therefore, extensibility of more than 1.5 cm is “positive.” If extensibility >2.0 cm is present especially in combination with other cutaneous features, such as papyraceous scars, molluscoid pseudotumors and/or subcutaneous spheroids, consider other EDS types as possible alternative diagnoses (mainly cEDS and classical-like EDS)
Feature B: Family history (1 or more first-degree relatives must meet criteria)
Feature C: MSK Complications(need ≥1)
- MSK pain in ≥2 limbs, recurring daily for ≥3 months
- Chronic widespread pain for ≥3 months
- Recurrent joint dislocations or frank joint instability, in the absence of trauma (a or b)
- ≥3 atraumatic dislocations in same joint or ≥2 more atraumatic dislocations in two difference joints occurring at different times
- Medical confirmation of joint instability at two or more sites not related to trauma
Criterion 3: All three prerequisites must be met
- Absence of unusual skin fragility.
- Exclusion of other heritable and acquired connective tissue disorders. In patients with an acquired onnective tissue disorder, additional diagnosis of hEDS requires meeting both Features A and B of Criterion 2. Feature C of Criterion 2 cannot be counted in this situation.
- Exclusion of alternative diagnoses that may also include joint hypermobility by means of hypotonia and/or connective tissue laxity
Unproven triad of hEDS, MCAS, and POTS
Kohn et al evaluated the literature behind each of these conditions, and the relationship between them[2]. They concluded that there is no proven relationship between hypermobile Ehlers Danlos Syndrome, Mast Cell Activation Syndrome, and POTS, and no proven pathophysiological mechanism linking them. Most studies to date used the older criteria of hEDS which was much more inclusive and more vague, making analysis more difficult. They theorised that the reason that these conditions have been associated is because there is a large overlap of non-specific symptomatology, summarised in their Venn Diagram below.
Article Downloads
File:EDS classifications 2017 - malfait2017.pdf File:Kohn2019 The Relationship Between hEDS POTS and MCAS.pdf
References
- ↑ Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8-26. doi:10.1002/ajmg.c.31552
- ↑ Kohn A, Chang C. The Relationship Between Hypermobile Ehlers-Danlos Syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), and Mast Cell Activation Syndrome (MCAS). Clin Rev Allergy Immunol. 2020;58(3):273-297. doi:10.1007/s12016-019-08755-8