Idiopathic Scoliosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{partial}} | ||
{{condition | |||
|image=Scoliosis-illustration.jpg | |||
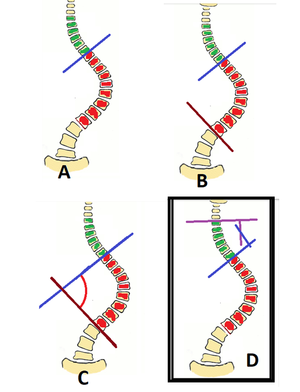
|caption=Radiographic scoliotic measurements | |||
|name= | |||
|taxonomy= | |||
|synonym= | |||
|definition=3D spinal deformity with at least 10° of curvature in the coronal plane. | |||
|epidemiology=2-4% of adolescents | |||
|causes= | |||
|pathophysiology=asymmetrical vertebral gorwth | |||
|classification=Infantile, Juvenile, Adolescent, Adult. | |||
|primaryprevention= | |||
|secondaryprevention= | |||
|riskfactors= | |||
|clinicalfeatures= | |||
|history= | |||
|examination= | |||
|diagnosis=Cobb angle greater than 10° and exclusion of other causes. | |||
|tests=Whole spine radiographs | |||
|ddx=neuromuscular, syndromic, congenital, degenerative, non-structural. | |||
|treatment=monitoring, bracing, surgery. | |||
|prognosis=depends on curve magnitude and progression. | |||
}} | |||
Idiopathic Scoliosis is a three dimensional spinal deformity in frontal, sagittal, and axial planes. It is defined as a coronal spinal curvature of at least 10° with rotation of the vertebral bodies and has unknown aetiology. | Idiopathic Scoliosis is a three dimensional spinal deformity in frontal, sagittal, and axial planes. It is defined as a coronal spinal curvature of at least 10° with rotation of the vertebral bodies and has unknown aetiology. | ||
| Line 271: | Line 295: | ||
=== Surgery === | === Surgery === | ||
The goal of surgery is prevention of curve progression and correction of the deformity. It usually involves curve correction and spinal instrumentation and fusion. The lower lumbar motion segments tend to be left unfused. | The goal of surgery is prevention of curve progression and correction of the deformity. It usually involves curve correction and spinal instrumentation and fusion. The lower lumbar motion segments tend to be left unfused. | ||
== See Also == | == See Also == | ||
Revision as of 19:29, 24 July 2021
Idiopathic Scoliosis is a three dimensional spinal deformity in frontal, sagittal, and axial planes. It is defined as a coronal spinal curvature of at least 10° with rotation of the vertebral bodies and has unknown aetiology.
Epidemiology
Idiopathic scoliosis is the most common structural spinal deformity in children and adolescents. It affects about 2-3% of adolescents, but only 0.1-0.3% for curvatures greater than 30°. The most common scoliosis is a thoracic curve to the right side. The primary age of onset is 10 to 15 years.
With small curves there is an equal prevalence of affected males and females. However there is a female predominance with increasing curve magnitude.
In the infantile form, which presents at 0-3 years of age, there is a predominance in males at 3:2. At 3-6 the female to male ratio is 1:1; at 3-10 it is 2:1 to 4:1; at 10 years the ratio is 8:1.
Aetiology
The exact aetiology is unknown. There appears to be asymmetrical growth of anterior column of the vertebrae with resulting tethering of the posterior elements. The underlying cause for this imbalance of growth is unknown.
There are thought to be genetic factors controlling for scoliosis. This has been indicated by population and twin studies. However no specific gene or genes have been found. There is variable expression and so environmental factors also contribute to the pathogenesis.
There has been interesting research done on platelets as both skeletal muscle and platelets have myosin/actin contractile systems. There is an association with scoliosis and a defective contractile system in platelets.
Calmodulin and melatonin interact with the actin/myosin system with calmodulin regulating calcium influx from the sacroplasmic reticulum and melatonin binding to calmodulin as an antagonist. Research has suggested abnormal levels of these substances in scoliotic individuals.
Classification
Age Based Classification
The Scoliosis Research Society (SRS) classifies idiopathic scoliosis based on age
- Infantile (IIS): manifests between birth and 3 years of age. It affects more boys than girls, and is related to the supine position of the baby. 70-90% resolve spontaneously
- Juvenile (JIS): manifests between 3 and 10 years of age. The incidence is equal in boys and girls, and has the same progression and AIS.
- Adolescent (AIS): manifests between 10 years and skeletal maturity. It is more common in women (70%)
- Adult: over 18 years: The adult form is differentiated from primary degenerative scoliosis. The adult idiopathic type is an idiopathic scoliosis that was present at the end of growth and has progressive secondary degenerative changes.
Radiological Classification
The SRS classifies a curve as thoracic if the apex is at the T2 to T11/12 disc, thoracolumbar if the apex is at T12 or L1, and lumbar if the apex is at the L1/2 to L4 disc.
King and Lenke are other classification systems. There is a problem with reliability of grading systems.
Clinical Assessment
- Left thoracic curve
- Apical kyphosis
- Rapid curve progression
- Structural abnormalities such as a hemivertebra
- Pathological reflexes, radicular pain, foot deformities
History
- Family history of spinal deformities or spinal disease
- Age
- Sexual maturity: Asking about age of menarche and secondary sex characteristics can help ascertain the level of skeletal maturation. Curve progression is less common after the onset of menarche.
- Pain: Most adolescents are asymptomatic. However 25% of patients have back pain as their initial presentation, and another 9% develop pain on follow up.[1] Signs of underlying pathology include constant pain, night pain, and radicular pain.
- Neurological symptoms: Enquire about bladder or bowel dysfunction, as well as intellectual or motor delay
- Previous illnesses or trauma
- Psychological distress
General Physical Examination
- Height: Serial heights helps to determine the peak growth spurt which is a predictor of the degree of curve progression. To calculate this you need to have at least 3 lots of 6 monthly regular measurements. In girls, this value is 9cm / year and peak height velocity occurs on average at 12 years of chronological age. In males it is 10cm / year and occurs on average at 14 years. The total duration of the growth spurt is about 2.5 to 3 years.
- Stage of sexual maturity: Assess the stage of sexual maturity using the Tanner stage.
- Skin and musculoskeletal system: Look for cafe au lait spots, subcutaneous nodules, and axillary freckling of neurofibromatosis; hair patches or dimples of spinal dysraphisms; hypermobility of Marfan and Ehlers-Danlos.
- Pelvic asymmetry: Assess for pelvic malalignment and leg length discrepancies as causes of pseudoscoliosis
- Neurological examination: Look for pes cavus, limb weakness, reflex asymmetry or absence including cutaneous abdominal reflexes. Patellar and/or Achilles hyperreflexia should raise suspicion of a non-idiopathic cause of scoliosis.
Spinal Examination
The patient should stand barefoot, with their legs straight, and with an uncovered back that is accessible to the examiner. Boys should be in underwear and shorts, and girls should be in underwear and a bra.
From behind observe the following:
- Shoulder heights
- Scapula heights
- Iliac crest heights
- Plumb line: drop a plumb line from the C7 spinous process. This should fall between the intergluteal cleft. If not then measure the distance from the plumb line to the intergluteal cleft.
- Symmetry of the triangular space between the medial aspect of each arm with the adjacent trunk.
- Adam's test: The patient stands and bends forward at the waist with the head as low as possible without flexing the knees until the shoulders are at hip height while holding their arms hanging straight down with palms together in a prayer position. The examiner assesses for symmetry of the back from behind and beside the patient while looking for any back or rib cage abnormalities such as a rib hump.
- Seated Adam's test: Non-structural causes can be assessed by examining the patient sitting on the bed and bending forward. Structural scoliosis persists in this position, while a non-structural scoliosis (e.g. due to leg length discrepancy) disappears.
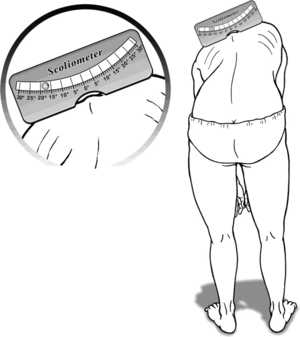
- Measurement of trunk rotation angle: Scoliometer use is ideal but not necessary in primary care. This is an instrument that is placed on the back during the Adams test and is used to provide an objective measure of the curve. A rotation of 5° correlates with a 20° Cobb angle.
- Assess the scoliotic curve direction. 90% of adolescent idiopathic scoliosis curves are right thoracic, left lumbar curves, i.e. the curve is convex towards the right.
From the side observe the following:
- Rounded shoulders
- Abdominal prominence due to poor muscular tone
From the front observe the following:
- Pectus excavatum or carinatum (Marfan)
- Asymmetry of breast development
Differential Diagnosis
Child and adolescent idiopathic scoliosis accounts for approximately 80% of cases. It is a diagnosis of exclusion and is differentiated from neuromuscular and congenital scoliosis. In adults degenerative scoliosis is a consideration. Also non-structural causes such as leg-length discrepancy occurs.
- Idiopathic Scoliosis
- Neuromuscular Scoliosis: lower or upper motor neuron diseases, myopathies
- Syndromic Scoliosis: Marfan, Ehlers-Danlos, osteogenesis imperfecta, neurofibromatosis, osteochondrodysplasia
- Congenital Scoliosis: vertebral and extraverterbral disorders
- Adult Degenerative Scoliosis
- Non-Structural Scoliosis
- Other: rheumatoid diseases, trauma, bone tumours.
Imaging
Initial radiological investigations should include whole spine radiographs from the cranium to the pelvis, including anteroposterior (or posteroanterior which dramatically reduces radiation) and lateral views.
The patient should be standing barefoot with a relaxed trunk to avoid compensating positions. If the patient has difficulty standing then they can be imaged in a semi-sitting position to maintain the effect of gravity on the curves.
If surgery is being considered, then a full length posteroanterior film is often taken of the patient side bending to the right and left. This assesses curve flexibility.
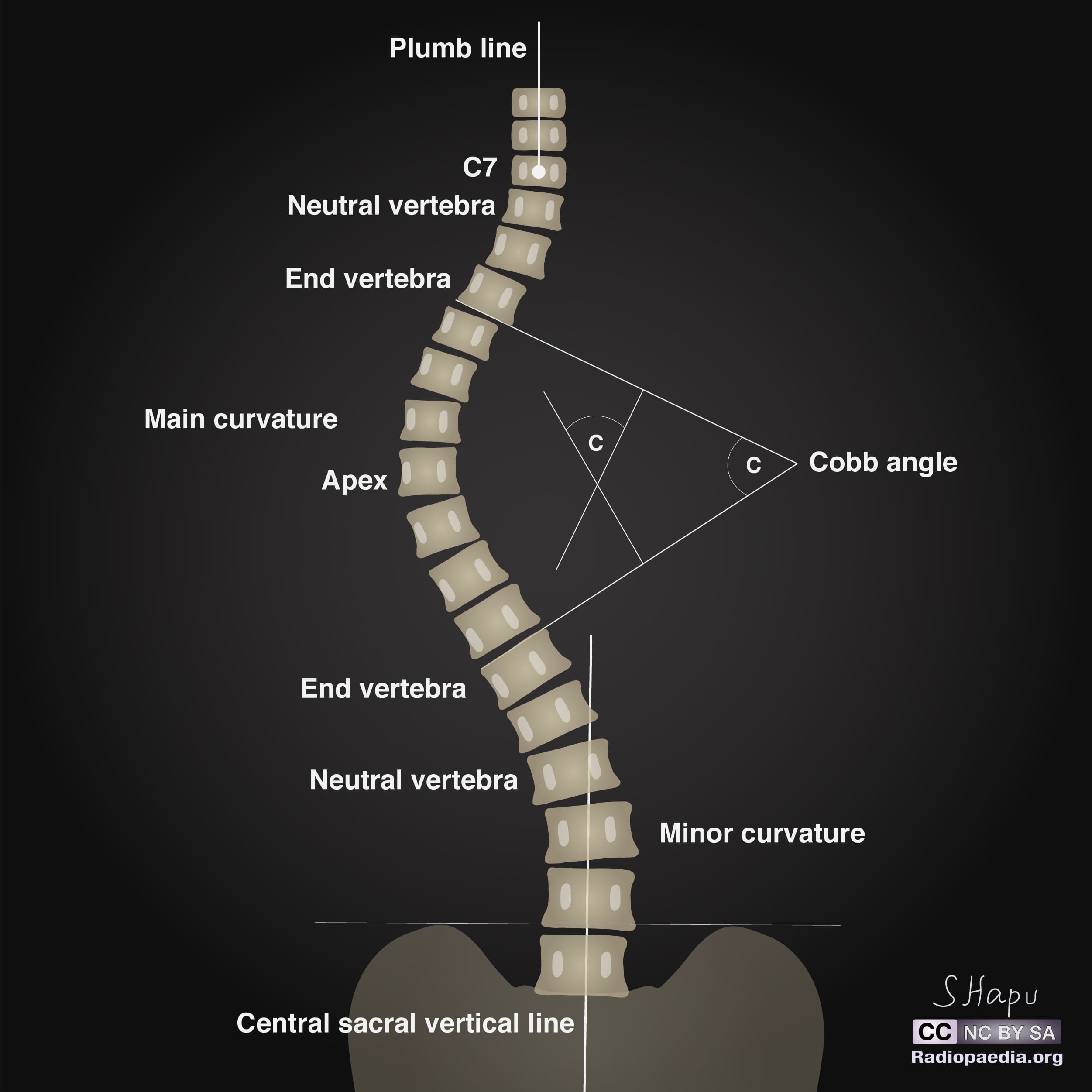
Cobb Angle
The magnitude of a scoliotic curve is determined by the Cobb angle. To measure the Cobb angle first identify the "end vertebra" which are the top and bottom-most vertebral bodies in the curve.
Lines are then drawn along the superior endplate of the highest vertebral body and inferior endplate of the lowest vertebral body. The lines are extended until they intersect, and the angle that forms is the Cobb angle.
In smaller curves the angle may be too small to allow intersection using the above method. In that situation extend the lines a short distance, then draw perpendicular lines from each line towards the other line. The angle that forms from the intersection of the perpendiculars is the Cobb angle.
Alignment
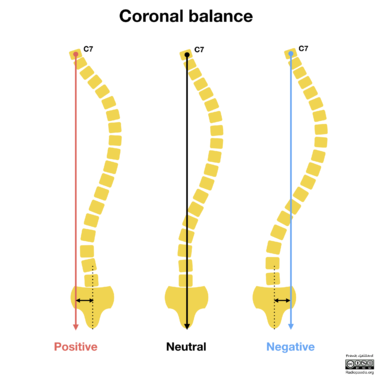
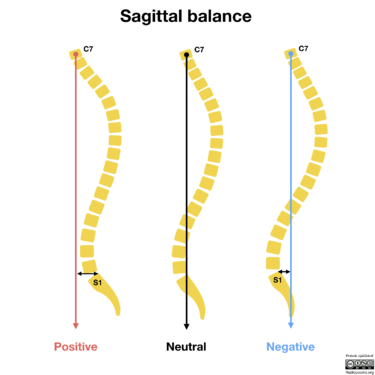
Alignment is measured in both the coronal and sagittal planes using a plumb line starting at the base of C7. This needs to be performed on erect full-length spine radiographs without lateral bending
In a neutral coronal balance the C7 plumb line lies within 2cm of the centre of the sacrum. When the C7 plumb line sits to the left of the sacrum there is a negative coronal balance, when it sits to the right there is a positive coronal balance. In the coronal plane the spine should have less than 10° of curvature.
In neutral sagittal balance the C7 plumb line lies within 2cm of the posterior-superior corner of S1. If the C7 plumb line lies anterior to S1 there is a positive sagittal balance, and if it lies posterior to S1 there is a negative sagittal balance. There is a wide range of normal curves in the sagittal plane. The thoracic kyphosis ranges from 10° to 60°, while the lumbar lordosis ranges from 20° to 60°. A positive sagittal balance is associated with worse pain and disability.
Skeletal Maturity
Including the iliac crests allows not only measurement of the pelvic tilt but also bone maturity by Risser's sign. Risser's sign refers to the appearance of the iliac apophysis on the pelvis. The stages represents the state of ossification of the iliac crests, which begins at the ASIS and progresses back towards the PSIS.
- Stage 0: no ossification centre at the level of iliac crest apophysis
- Stage 1: apophysis under 25% of the iliac crest
- Stage 2: apophysis over 25-50% of the iliac crest
- Stage 3: apophysis over 50-75% of the iliac crest
- Stage 4: apophysis over >75% of the iliac crest
- Stage 5: complete ossification and fusion of the iliac crest apophysis
The Risser sign isn't perfect. It correlates differently in boys and girls with skeletal maturity, and typically appears after the peak height velocity. Grade 5 may not match the completion of vertebral growth. Also stage 0 and stage 5 appear similar.
If there are doubts regarding skeletal maturity then request a bone age x-ray of the left hand and wrist. The scoring of the metacarpals and phalanges are more closely related to scoliosis progression than Tanner stage and Risser sign. Assessment of elbow maturation is another method and is more accurate than hand maturation.[4]
Radiation Dose
Whole spine radiographs are equivalent to 100 chest x-rays and there is an increased risk of death from breast cancer compared to the general population. The following precautions should be taken
- Wherever possible radiographs should be done form a posteroanterior projection which reduces the radiation dose to the breasts by 70-80%.
- Gonadal protection in both sexes
- In analogue equipment provide breast protection. This isn't necessary with digital equipment.
High Tech Imaging
MRI is warranted if there is a suspicion of an underlying disease such as in the presence of a left thoracic curve or abnormal neurological findings. MRI can identify pathology such as tumours, syrinx, and Chiari malformations.
Natural History and Curve Progression Risk
Long Term Natural History
One prospective case series followed up 133 patients over an average of 40.5 years (range 31-53 years). 68% of adolescent idiopathic curvatures progressed past skeletal maturity. [5]
- Thoracic curves that were greater than 50° progressed at an average rate of 1° per year. Thoracic curves under 30° did not progress.
- Thoracolumbar curves progressed at 0.5° per year
- Lumbar curves progressed at 0.24° per year.
The long term health consequences of adolescent idiopathic scoliosis was evaluated in a 50 year follow up study of 117 untreated patients with adolescent idiopathic scoliosis and compared them to controls. The authors found that while there was an increased risk of back pain (61% vs 35% in controls), there was no increased rate of mortality, nor any increased rate of cardiac or pulmonary disease. However in those with thoracic curves of more than 100° there was an increased risk of death from right heart failure.[6]
Risk Factors of Curve Progression in Scoliosis[4]
The determinants of progression are the age and sex of the individual, the stage of pubertal development, the growth potential, the curve pattern and grade at the time of diagnosis.
| Risk factor of progression | Comment |
|---|---|
| Age | The younger the age at diagnosis, the greater the possibility of progression at the onset of the adolescent growth spurt |
| Sex | Progression is more common in girls |
| Menarche | Progression is less likely in the post-menarche period |
| Remaining skeletal growth | The greater the skeletal immaturity, the greater the risk of progression. |
| Curve pattern | Double curves have a higher risk of progression compared to single curves. Left thoracic curves (convex towards the left) are also more likely to progress. |
| Curve magnitude | Greater curves have a higher risk of progression. Curves between 50-70° are most likely to progress in adulthood. |
The remaining skeletal growth is determined by rate of growth, age of telarche and menarche, Tanner's stage, Risser's sign, and/or bone age. It should take into account that the primary growth spurt occurs 6-12 months before menarche in Tanner 3 at an average age of 12 in girls, and in Tanner 4 at an average age of 14 in boys.
| Initial Curve | Girls 10-12 years | Girls 13-15 years | Girls >15 years | Boys |
|---|---|---|---|---|
| <19° | 25% | 1% | <1% | 3% |
| 20-29° | 60% | 40% | 10% | 6% |
| 30-56° | 90% | 70% | 30% | |
| >60° | 100% | 90% |
Management
Overview
Standard management options include observation, bracing, and surgery. Considerations include skeletal maturity and the grade of the curve. Generally patients are referred to a specialist clinic.
Management According to Skeletal Maturity
Skeletal immaturity
- <25º: physical examination and radiographs every 4-6 months.
- 25º-40º: bracing.
- > 40º or progression despite the orthosis: should consider surgery.
Intermediate skeletal maturity
- <20º: clinical observation.
- 20º-30º: radiographs every 6-9 months.
- > 30º: radiographs strictly every 6 months.
- > 45 °: surgery should be considered.
Skeletal maturity
- <40º: unspecified.
- > 40º: annual evaluation.
- ≥ 50º or curve in progression: surgery.
| Curve | Therapy |
|---|---|
| 10-25° | observation every 6 months until skeletally mature including sequential photographs, sitting height. |
| 25-30° | Bracing |
| 30-40° | Bracing |
| > 40° | Surgery in skeletally immature patients |
| > 50° | Surgery in skeletally mature patients. |
Restrictive lung disease may become a serious health issue with thoracic curves larger than 70°.
Bracing
Bracing is a controversial treatment modality, with divergent practices across specialist clinics. The results from research has been mixed. Bracing has been found to cause significant psychological distress unless the patient is well supported by the family.[9]
Physical Therapy
There is no scientific evidence that any form of manual therapy, manipulation, electrical stimulation, or corrective exercises can slow or stop the progression of scoliosis. There are a variety of scoliosis physical therapy philosophies around the world.
Surgery
The goal of surgery is prevention of curve progression and correction of the deformity. It usually involves curve correction and spinal instrumentation and fusion. The lower lumbar motion segments tend to be left unfused.
See Also
- Scheuermann's Disease
- Coronal Balance of the Spine
- Sagittal Balance of the Spine
- Spine Service (starship.org.nz)
References
- ↑ Ramirez N, Johnston CE, Browne RH. The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am 1997;79:364-8.
- ↑ Ma, Hsuan-Hsiao et al. “Application of two-parameter scoliometer values for predicting scoliotic Cobb angle.” Biomedical engineering online vol. 16,1 136. 4 Dec. 2017, doi:10.1186/s12938-017-0427-7
- ↑ Adolescent Idiopathic Scoliosis. Orthopaedia.com. Available from https://orthopaedia.com/page/Adolescent-Idiopathic-Scoliosis
- ↑ 4.0 4.1 Altaf F, Gibson A, Dannawi Z, Noordeen H. Adolescent idiopathic scoliosis. BMJ. 2013 Apr 30;346:f2508. doi: 10.1136/bmj.f2508. PMID: 23633006.
- ↑ Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447-55.
- ↑ Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003 Feb 5;289(5):559-67. doi: 10.1001/jama.289.5.559. PMID: 12578488.
- ↑ Bueche MJ. Scoliosis and kyphosis. Neinstein LS, Gordon CM, Katzman DK, Rosen D, et al, eds. Adolescent Health Care: a practical guide. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2007.Pages.235-42
- ↑ Bueche MJ. Scoliosis and kyphosis. En: Neinstein LS, Gordon CM, Katzman DK, Rosen D, et al, eds. Adolescent Health Care: a practical guide. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2007.Págs.235-42.
- ↑ Boos, Norbert, and M Aebi. Spinal disorders : fundamentals of diagnosis and treatment. Berlin New York: Springer, 2008.
- Comité Nacional de Adolescencia SAP, et al. Consenso de escoliosis idiopática del adolescente [Adolescent idiopathic scoliosis]. Arch Argent Pediatr. 2016 Dec 1;114(6):585-594. Spanish. doi: 10.5546/aap.2016.585. PMID: 27869435.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,