Iliotibial Band Syndrome: Difference between revisions
mNo edit summary |
m (Text replacement - "Leg length discrepancy" to "Leg length discrepancy") |
||
| (One intermediate revision by the same user not shown) | |||
| Line 36: | Line 36: | ||
* Iliopsoas muscle contracture | * Iliopsoas muscle contracture | ||
* Gastrocnemius and soleus muscle tightness | * Gastrocnemius and soleus muscle tightness | ||
* Leg length discrepancy | * [[Leg Length Discrepancy|Leg length discrepancy]] | ||
=== Extrinsic === | === Extrinsic === | ||
| Line 67: | Line 67: | ||
There may be tightness with the Ober test, or pain with the [https://www.youtube.com/watch?v=PmUGl7ryQOo Noble test]. However neither of these special tests have been properly validated. | There may be tightness with the Ober test, or pain with the [https://www.youtube.com/watch?v=PmUGl7ryQOo Noble test]. However neither of these special tests have been properly validated. | ||
Look for biomechanical variations. There may be a leg length discrepancy with ITBS occurring in the shorter leg. Forefoot varus and high knee Q angles are also associated features. | Look for biomechanical variations. There may be a [[Leg Length Discrepancy|leg length discrepancy]] with ITBS occurring in the shorter leg. Forefoot varus and high knee Q angles are also associated features. | ||
Assess ankle mobility by testing foot dorsiflexion with the hip flexed to 90 degrees and the knee extended. Normal range is dorsiflexion to neutral, and if this is not possible then the calf is tight leading to increased knee flexion and ankle pronation and thereby potentially being a contributor to ITBS. | Assess ankle mobility by testing foot dorsiflexion with the hip flexed to 90 degrees and the knee extended. Normal range is dorsiflexion to neutral, and if this is not possible then the calf is tight leading to increased knee flexion and ankle pronation and thereby potentially being a contributor to ITBS. | ||
Latest revision as of 21:16, 15 April 2022
Iliotibial band syndrome is a common cause of lateral knee pain in runners.
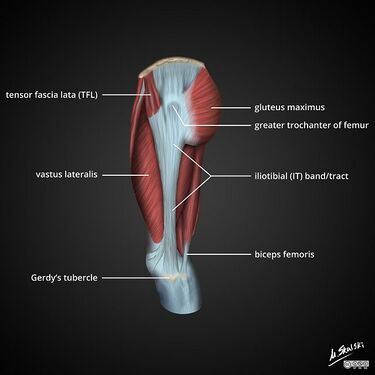
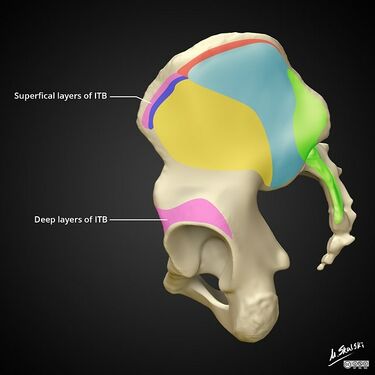
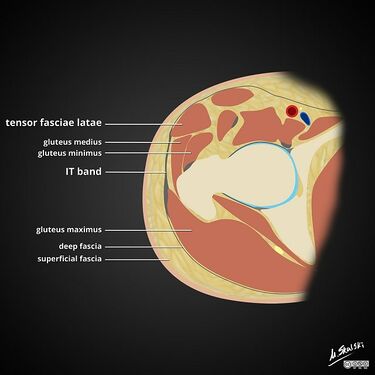
Anatomy
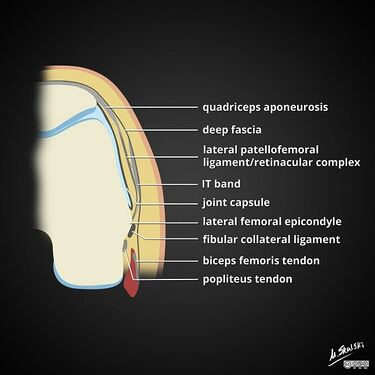
The ITB is a thickened part of the tensor fascia lata, and has some contribution from fibres of the gluteal muscles. It it connected to the linea aspera by an the intermuscular septum and to the supracondylar region of the femur by course fibrous bands. It inserts on the lateral border of the patella, the lateral retinaculum, and Gerdy's tubercle.
One view is that ITB function depends on knee position. Between full extension to 20-30° of flexion the ITB is anterior to the lateral femoral epicondyle, and so functions as an active knee extensor. At 20-30° of flexion of flexion the ITB sits posterior to the lateral femoral epicondyle and functions as an active knee flexor.[1]
However another view is that the ITB functions to tense the fascial envelope around the thigh to promote optimal muscle function. The connection between the lateral femoral distal part of the ITB (from lateral epicondyle to Gerdy's tubercle) is actually a ligament, and the proximal part (associated with TFL and gluteus maximus) is the tendinous portion. The tendinous portion therefore doesn't cross the knee and so can't have any action on the knee joint. In this view the anterior fibres are active in extension and the posterior fibres are active in flexion.[2]
Epidemiology
ITBS is common in athletes, and the most common cause of lateral knee pain in this population.
Pathophysiology
The traditional theory relates to friction in that ITBS is caused by excessive friction of the distal ITB and/or its associated bursa as it glides over the lateral femoral epicondyle with repeated flexion-extension cycles of the knee. This traditional theory has been questioned because the ITB is actually tethered at the lateral femoral epicondyle by the epicondylo-patellar ligament and patellar retinaculum, and so does not make any significant movement in the sagittal plane.
An alternative theory relates to compression. In this theory ITBS is caused by increased compression of a highly vascularised and innervated layer of fat and loose connective tissue separating the ITB from the femoral epicondyle. Proponents suggest that the underlying cause is impaired hip muscle function.[2]
The ITB is under greatest tension at 30 degrees of flexion, and so repeated motion in this angle may lead to irritation in some individuals. Runners approach 30 degrees of flexion with foot strike, while cyclists have 30 degrees of flexion in the down-pedal position.
Risk Factors
There are both intrinsic and extrinsic risk factors[3]
Intrinsic
There are two types of alignment disorders
- Weak hip abductors leading to increased hip adduction (genu valgum) and increased internal rotation at the knee. This places a rotational strain on the distal ITB, and because of its tethering from the lateral femoral epicondyle to Gerdy's tubercle it can't accomodate this rotational strain. This is most common in female or novice runners.
- Increased hip abduction, genu varum, or increased ankle supination leading to increased tension of the ITB at the femoral epicondyle. The strain here is angular rather than rotational because the genu varum causes the ITB to compress over the lateral joint line. This is more common in experienced distance runners.
Other intrinsic factors include
- Iliopsoas muscle contracture
- Gastrocnemius and soleus muscle tightness
- Leg length discrepancy
Extrinsic
- Running surface with horizontal (e.g. cambered road with running in the same direction) or vertical gradient (e.g. downhill running)
- Workouts: Sudden increase in running or cycling distance, high weekly running mileage, hill workouts in cycling.
- Footwear factors: increased heel height and width, leading to increased supination
- Excessively long strides
- Improper bike fit
- Cold weather exercise
Clinical Features
History
Iliotibial band syndrome usually presents at pain over the lateral aspect of the knee, but occasionally can become irritated proximally and present as hip pain. In the lateral knee the pain is usually located over the lateral femoral epicondyle, but this may radiate distally to Gerdy's tubercle, or proximally to the tensor fascia lata.
Common aggravating activities are those that involve repetitive flexion and extension cycles of the knee such as running and cycling, and the pain usually starts within several minutes. There is often aggravation with activity on inclined surfaces such as downhill running. The posterior fibres of the ITB are in contact with the lateral femoral epicondyle at approximately 20° to 30° of knee flexion, and during downhill running there is a reduced knee flexion angle upon foot strike, leading to the ITB fibres being in more frequent contact with the lateral femoral epicondyle. ITBS is less common in sprinters because their knees have a higher degree of flexion at foot strike.
The pain is usually diffuse initially over the whole lateral knee. The pain usually eventually localises to an area 2 to 4cm proximal to the lateral joint line.
Pain can eventually become constant even at rest with continued aggravation.
Examination
In some cases the patient may have a stiff-legged gait due to avoidance of knee flexion.
There is tenderness over the lateral femoral epicondyle.
Pain can be provoked by single-leg stance with knee flexion to 30°
There may be tightness with the Ober test, or pain with the Noble test. However neither of these special tests have been properly validated.
Look for biomechanical variations. There may be a leg length discrepancy with ITBS occurring in the shorter leg. Forefoot varus and high knee Q angles are also associated features.
Assess ankle mobility by testing foot dorsiflexion with the hip flexed to 90 degrees and the knee extended. Normal range is dorsiflexion to neutral, and if this is not possible then the calf is tight leading to increased knee flexion and ankle pronation and thereby potentially being a contributor to ITBS.
Assess hip flexor mobility by performing the modified Thomas test. Reduced hip extension may be a contributor to ITBS.
Assess hip abductor strength. This can be assessed by having the patient lie on their side and testing resisted hip abduction strength. Another method of testing is repeated single leg shallow knee bends to 20 degrees of flexion, looking for the knee to turn medially.
Assess running gait as they run towards you. Look specifically for medial movement of the knee when the foot is in contact with the ground in novice runners, and excessive genu varum in advanced runners.
Imaging
Ultrasound allows dynamic imaging of the motion of the ITB with flexion and extension, and can also assess for fluid and thicknening. Fluid associated with the iliotibial band is not a useful finding because it is present in 100% of asymptomatic recreational runners.[4]
MRI can be useful when the diagnosis is in question and to exclude other pathologies.
In the knee typical MRI findings are ITB thickening, and fluid collection deep to the ITB.
In the hip there are similar soft tissue changes but there may also be associated tendinopathies of the gluteus medius and minimus tendons, as well as marrow oedema in the affected bone.
There may be primary or secondary (adventitious) bursae. A bursa may be confused with a normal lateral recess.
Differential Diagnosis
- Lateral meniscus tear
- Posterolateral corner injury
- Patellar dislocation or subluxation
- Lateral collateral ligament tear
- Iliotibial Band Syndrome
- Osteoarthritis exacerbation
- Osteochondral lesion lateral femoral condyle
- Popliteus Tendinopathy
- Biceps Femoris Tendinoapthy
- Semimembranosus Tendinopathy/bursitis
- Fibula head fracture
- Proximal Tibiofibular Joint Instability
- Snapping Biceps Femoris and Popliteus Tendons
- Peroneal Nerve Compression/Neuritis
Treatment
There is a paucity of evidence to guide treatment. Treatment can be divided into several phases: acute, subacute, chronic, and adaptation phases.
In the acute phase provocative activities should be avoided.
Corticosteroid injections can be used to reduce inflammation, and is usually injected where the ITB crosses the lateral femoral condyle. The addition of local anaesthetic can provide diagnostic value.
Stretching is sometimes recommended once the acute inflammation has settled, however many argue that the ITB cannot be stretched because of its numerous attachments.
In the subacute phase biomechanical abnormalities should be addressed.
Strengthening is recommended after range of motion has improved. Here the hip abductors are focused on.
It may be prudent to use general principles of treatment of the tendinopathies.
Surgery is very uncommon. Approaches involve resection and incisions of the ITB to reduce tension and minimise bony contact.
There are also various experimental interventions such as prolotherapy, PRP, topical nitroglycerin, and percutaneous needle tenotomy.
Further Reading
References
- ↑ 1.0 1.1 Strauss EJ, Kim S, Calcei JG, Park D. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011 Dec;19(12):728-36. doi: 10.5435/00124635-201112000-00003. PMID: 22134205.
- ↑ 2.0 2.1 Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, Best TM, Benjamin M. Is iliotibial band syndrome really a friction syndrome? J Sci Med Sport. 2007 Apr;10(2):74-6; discussion 77-8. doi: 10.1016/j.jsams.2006.05.017. Epub 2006 Sep 22. PMID: 16996312.
- ↑ Jonathan Jackson, MD. Iliotibial Band Syndrome. Up to Date. Apr 16, 2019
- ↑ Jelsing EJ, Finnoff J, Levy B, Smith J. The prevalence of fluid associated with the iliotibial band in asymptomatic recreational runners: an ultrasonographic study. PM R. 2013 Jul;5(7):563-7. doi: 10.1016/j.pmrj.2013.02.010. Epub 2013 Feb 27. PMID: 23454446.
- ↑ Ellis R, Hing W, Reid D. Iliotibial band friction syndrome--a systematic review. Man Ther. 2007 Aug;12(3):200-8. doi: 10.1016/j.math.2006.08.004. Epub 2007 Jan 8. PMID: 17208506.