Knee Joint
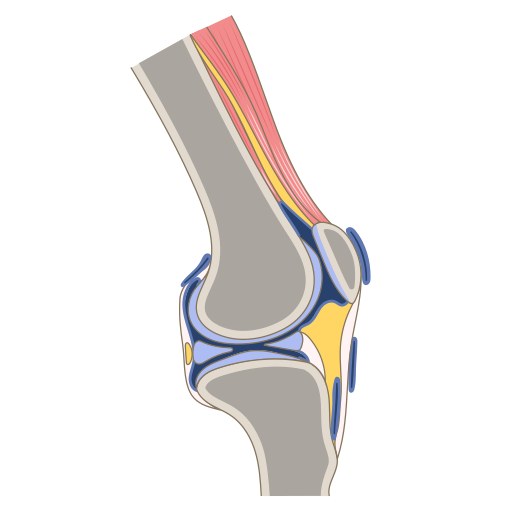
The knee is a two joint structure composed of the tibiofemoral joint (modified Hinge Joint) and the patellofemoral joint (Saddle Joint) and is the largest joint in the body. It sits between the body's two longest lever arms namely the tibia and the femur which lends it to injury.
This article discusses knee joint anatomy. For a discussion on biomechanics of the knee see Knee Biomechanics.
Bones and Articulations
The knee joint contains four bones: the femur, tibia, patella, and fibula.
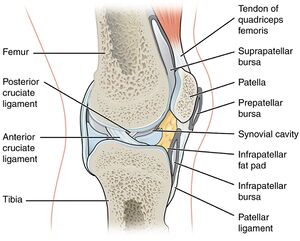
It has three compartments: the medial tibiofemoral, lateral tibiofemoral, and patellofemoral compartments. The three compartments all share a common synovial cavity.
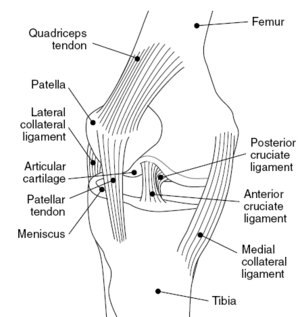
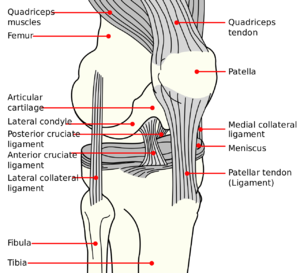
The knee has three articulations: medial and lateral tibiofemoral and patellofemoral joints. The tibiofemoral articulations connect the distal femur to the tibia. The distal femur broadens to form the medial and lateral femoral condyles. The tibia is relatively flat, but the sloped menisci permit a tight articulation with the convexity of the femoral condyles. The femoral condyles are separated by an intercondylar fossa, also known as the femoral groove, or femoral trochlea. The joint lines are formed by the femoral condyles and tibial plateaus.
The patella is sesamoid shaped and is embedded within the quadriceps tendon that articulates with the trochlear grove of the femur. It increases the mechanical advantage of the quadriceps. The fibula head is located within the knee capsule but isn't normally involved as a weight-bearing surface.
Structures Involved in Support and Stability
There are several structures that provide stability and cushioning to the knee joint.
- Hyaline cartilage lining the tibia and femur provide shock absorption
- Medial and lateral menisci provide shock absorption and distribute forces as well as play a role in joint lubrication.
- Anterior and posterior cruciate ligaments provide stability with anterior and posterior movements with flexion and extension
- Medial and lateral collateral ligaments provide support in their respective planes.
- Iliotibial band
- Posterolateral corner
Ligaments
Anterior Cruciate Ligament
The ACL arises from the posteromedial aspect of the lateral femoral condyle, runs distally in an anterior and medial direction, and inserts on the anteromedial aspect of the tibia in the intercondylar region. It has two bundles: an anteromedial bundle and posterolateral bundle. The anteromedial bundle is tight in flexion. The posterolateral bundle is tight in extension.
The ACL provides the primary resistance to anterior translation of the tibia on the femur. It also provides secondary restraint against tibial rotation, varus, and valgus forces.
Posterior Cruciate Ligament
The PCL arises from the anterolateral aspect of the medial femoral condyle. Here it traverses distally in a posterior and lateral direction inserting behind the intercondylar eminence, medial to the ACL. It is the thickest and strongest of all the knee ligaments. It is the primary structure providing resistance to posterior translation and external rotation. Resistance to posterior translation is greatest with knee flexion greater than 30 degrees. Resistance to external rotation is greatest with knee flexion greater than 90 degrees. In the setting of a deranged posterolateral corner it has maximal control of external rotation at 90 degrees of knee flexion.
Medial Collateral Ligament
This structure has both superficial and deep components.
The superficial MCL arises just proximal and posterior to the medial femoral epicondyle. There are two locations for insertion on the tibia: 1cm below the joint line and 6cm below the joint line. The superficial MCL is the primary static stabiliser of the medial knee and provides resistance against valgus and external rotation forces.
The deep MCL is a thickening of the joint capsule. It originates 1cm distal to the origin of the superficial MCL on the femur. Its insertion is on the medial meniscus and on the medial tibia slightly distal to the joint line. The deep MCL is a secondary valgus stabiliser when the superficial MCL is injured.
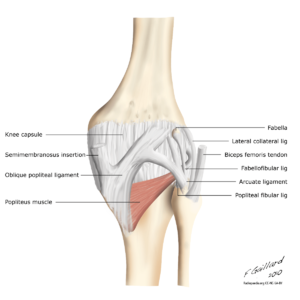
Lateral Collateral Ligament
The LCL has its origin on the lateral femoral epicondyle. It inserts on the lateral head of the fibula. It is the principal stabiliser against varus forces.
The biceps femoris splits and runs along either side of the LCL along to its attachment on the fibula head.
The popliteus muscle originates slightly inferior to the lateral femoral condyle, runs deep to the LCL, next to the biceps femoris, and inserts onto the posterosuperior aspect of the medial tibial condyle. Its has a few functions. It is an internal rotator of the tibia or external rotator of the distal femur. It has a protective effect to the posterior horn of the lateral meniscus during flexion as it pulls the posterior horn posteriorly. It also reinforces the PCL in prevention of anterior translation of the femur during deceleration and downhill running. The popliteus is reinforced by several posterolateral structures.
Anterolateral Ligament
The ALL arises from the lateral femoral epicondyle just anterior to the LCL, and inserts on the anterolateral region of the proximal tibia between Gerdy's tubercle and the fibula head. The precise role and clinical relevance of this structure are unknown, but it may help control internal tibial rotation and affect the pivot shift phenomenon.
Oblique Popliteal Ligament
The OPL is found in the posterior knee and is one of the components of the posteromedial corner. It is broad and flat and overlies the joint capsule. It courses at thirty degrees. There are variations in shape and attachments. Medially the insertions are the lateral expansion of the semimembranosus tendon and/or the posterior margin of the posteromedial tibia, as well as the posteromedial joint capsule and capsular arm of the posterior oblique ligament. Laterally the insertions are the meniscofemoral portion of the joint capsule, the fabella when present, and the lateral head of gastrocnemius and plantaris. The OPL prevents hypertension of the knee, and also excessive external rotation.
Other Structures
Menisci
Both femoral condyles have a crescent-shaped meniscus. This structure deepens the fossa where the condyles articulate with the tibia. They are thickest peripherally and attach to the rim of the tibia here. They taper down in thickness towards the inner aspect of the knee where they are unattached.
The predominant collagen is type I. Histologically menisci are developed so that the inner region is best developed to resist compression forces, and the outer region to resist tensile forces. They are much stronger (100x) in the circumferential direction than the radial direction
There are three vascular zones in the meniscus. The peripheral one third is directly supplied by blood vessels and so there is a reducing blood supply the more centrally located the tissue is. From outer to inner they are termed the red-red zone, the red-white zone, and the white-white zone. The inner part of the meniscus is supplied by diffusion from synovial fluid and so has a reduced healing capacity.
The lateral meniscus has a more circular shape and is more mobile anteriorly and posteriorly compared to the medial meniscus.
The medial meniscus is attached to the posterior oblique ligaments and the medial collateral ligament and is less mobile. This reduced mobility may be a factor in why it is more commonly injured than the lateral meniscus. The presence of an accessory iliotibialband-meniscal ligament is associated with a much greater prevalence of lateral meniscal injuries.[1]
Iliotibial Band
The ITB is a broad and thick fascial structure that runs from the tensor fascia lata, gluteus maximus, and other proximal muscles and attaches to the vastus lateralis anteriorly. It crosses the lateral femoral condyle prominence and attaches at Gerdy's tubercle which is found on the anterolateral aspect of the proximal tibia. It blends with the lateral patellar retinaculum close to the joint line.
Plica
Plica are embryological tissue remnants. They are related to the synovium and are normally thin and narrow. If irritated they become thick and fibrotic. Several plica can be found in the knee, but the medial plica is the one that most commonly becomes painful. The medial plica arises from the medial wall of the knee, traverses inferiorly around the medial femoral epicondyle, and attaches to the synovium that surrounds the infrapatellar fat pad.
Corners
Posterolateral Corner
The PLC is made up of several structures:
- Iliotibial tract
- Lateral collateral ligament
- Popliteus tendon
- Popliteofibular ligament,
- Popliteotibial and popliteomeniscal fascicles
- Middle third of the lateral capsular ligament
- Fabellofibular ligament
- Arcuate ligament
- Posterior horn of the lateral meniscus
- Lateral coronary ligament
- Posterolateral portion of the joint capsule
The PLC along with the PCL stabilise the knee against external rotation and posterior translation against a wide range of knee positions.
Posteromedial Corner
The PMC is located between the posterior margin of the MCL and medial border of the PCL. There are five structures that comprise the PMC
- Posterior oblique ligament
- Oblique popliteal ligament
- Meniscotibial ligament
- Semimembranosus tendon
- Posterior third of the medial meniscus.
Injuries, usually seen in athletes with the knee in valgus, can lead to increased stress on the cruciate ligaments and lead to anteromedial rotatory instability of the knee joint. PMC Injury is usually associated with ACL tear
Structures Involved in Knee Extension and the Anterior Knee
The extensor mechanism of the knee contains the:
- Quadriceps muscles
- Quadriceps tendon
- Patlelofemoral joint
- Patellar tendon
- Tibial tubercle
Quadriceps Tendon
The Quadriceps tendon is formed by the confluence of vastus intermedius, vastus lateralis, vastus medialis
Patella
The patella is sesamoid shaped. It lies within the quadriceps and patellar tendons and sits within the trochlear groove of the femur. The trochlear groove has a larger lateral facet and smaller medial facet, and is shallow proximally and deeper distally. The patella sits in the proximal narrow part of the groove in the knee extended position. When the knee is flexed it moves to the distal deeper part of the groove.
Other than the bony morphology, it is also stabilised by the complex medial and lateral retinaculae. The medial patellofemoral ligament is part of the medial retinaculum and originates from the medial margin of the patella and inserts onto the medial femoral epicondyle. It is the most important stabiliser of the patella.
Under the retinacula are the medial and lateral synovial recesses. These communicate with the suprapatellar pouch.
Patella Tendon
The patellar tendon is strap-like. It originates from the inferior patellar pole, runs in an oblique fashion, and inserts on the lateral aspect of the tibial tubercle.
Structures Involved in Knee Flexion and the Popliteal Fossa
Knee Flexors
The primary knee flexors are the hamstring muscles:
- Biceps femoris: originates at the ischial tuberosity, short head originates from the femoral shaft. Both insert on the fibular head
- Semitendinosus and semimembranosus: both originate from the ischial tuberosity, and insert on the medial tibia in the pes anserine.
Popliteal Fossa
The popliteal fossa has the following boundaries:
- Superior margin: distal portions of the semitendinosus and semimembranosus
- Lateral margin: biceps femoris
- Medial margin: semitendinosus and semimembranosus
- Inferior margin: medial and lateral heads of gastrocnemius
Gastrocnemius
In a knee extended position the gastrocnemius acts as an ankle plantarflexor. During knee extension, the muscle aids in prevention of anterior translation of the femur with respect to the tibia.
Bursa and Cystic Structures
Bursae of the Anterior Knee
There are four common bursae of the anterior knee:
- Suprapatellar bursa: found proximal to the knee joint capsule between the rectus femoris tendon and the femur. In most individuals it communicates with the knee joint.
- Prepatellar bursa: found directly anterior to the patella
- Superficial infrapatellar bursa: found superficial to the tibial tubercle and distal patellar tendon
- Deep infrapatellar bursa: found deep between the distal aspect of the patellar tendon and the anterior tibia.
The superficial bursae can become irritated from trauma or overuse such as with prolonged kneeling. The deep infrapatellar bursa can become irritated with repeated jumping or running where the knee extensors are overused.
Bursae of the Medial Knee
There are three common bursae of the medial knee:
- Pes anserine bursa: found between the insertion of MCL on the tibia and the conjoined distal tendon of sartorius, gracilis, and semitendinosus. It can become irritated from overuse with distance running, or with obesity and osteoarthritis.
- MCL bursa: found between the superficial and deep divisions of the MCL. Irritation can mimic meniscal tear symptoms.
- Semimembranosus-tibial collateral ligament bursa: "inverted U" shaped bursa. The superficial arm is found deep to the MCL and adjacent to the semimembranosus tendon. The deep arm is found between teh semimembranosus tendon and the medial tibial condyle.
Bursae of the Lateral Knee
There are no true lateral knee bursae. however in some individuals a secondary or adventitial bursa can develop with chronic friction between the iliotibial band and lateral femoral condyle.
Abnormal Structures
- Ganglions: abnormal benign structures that are lined by dense fibrous tissue and contain viscous fluid.
- Para-articular cysts: found in internal knee derangements such as meniscal tears
- Popliteal (Baker's) cysts: arise between the medial head of gastrocnemius and semimembranosus tendon. They usually lie in the medial aspect of the popliteal fossa, in the superior aspect of the medial femoral condyle. They can be superficial or deep, and can extend in a variety of directions. They are often seen with degenerative meniscal tears.
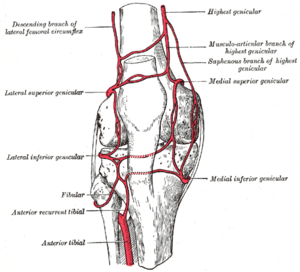
Neurovascular Structures
There is a neurovascular bundles that contains the popliteal artery, popliteal nerve, and tibial nerve (continuation of sciatic nerve). It travels directly posterior to the knee joint. Injury to the vasculature can occur in severe trauma such as in tibiofemoral dislocation.
The peroneal nerve is found laterally and is a division of the sciatic nerve. It starts its course between the medial border of the biceps femoris muscle and lateral head of gastrocnemius. It then passes laterally around the biceps femoris muscle, and dives between the peroneus longus and fibular head called the peroneal tunnel. Finally it splits into three branches: the deep peroneal, superficial peroneal, and recurrent peroneal nerves. The peroneal nerve is susceptible to trauma due to its superficial location and course through narrow spaces.
See Also
References
- Basic biomechanics of the musculoskeletal system - Nordin 4th edition 2012.
- ↑ Zimmermann SM, Njagulj V, Fritz B, Fucentese SF, Sutter R, Pfirrmann CWA. The Accessory Iliotibial Band-Meniscal Ligament of the Knee: Association With Lesions of the Lateral Meniscus. AJR Am J Roentgenol. 2019 Oct;213(4):912-917. doi: 10.2214/AJR.18.21071. Epub 2019 Jun 25. Erratum in: AJR Am J Roentgenol. 2019 Nov;213(5):1174. PMID: 31237768.