Lateral Femoral Cutaneous Nerve Entrapment: Difference between revisions
No edit summary |
No edit summary |
||
| (9 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{Authors | ||
{{ | |Authors=Jeremy | ||
| | }} | ||
| | {{Condition | ||
|synonym=Meralgia Paraesthetica | |quality=Partial | ||
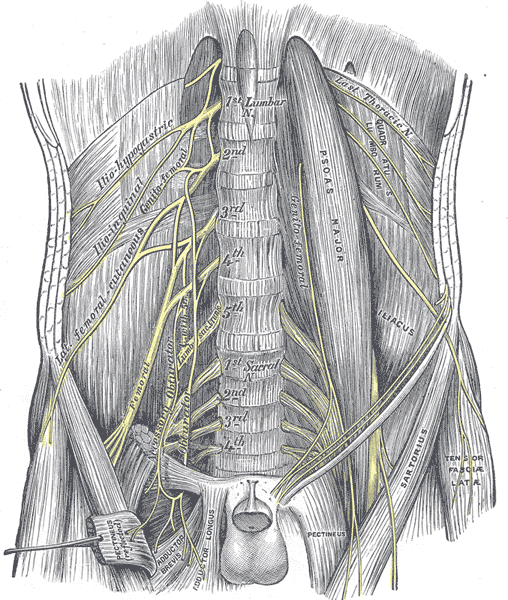
|image=lumbar-plexus-and-its-branches.png | |||
|synonym=Meralgia Paraesthetica, Bernhardt-Roth syndrome | |||
|epidemiology=3.4–4.3/10,000 person-years | |epidemiology=3.4–4.3/10,000 person-years | ||
|riskfactors=Obesity, diabetes, pregnancy. | |riskfactors=Obesity, diabetes, pregnancy. | ||
|history=Pain and/or dysaesthesia | |history=Pain and/or dysaesthesia | ||
| Line 18: | Line 14: | ||
|ddx=L2 or L3 radiculopathy, pelvic mass, superior gluteal nerve entrapment, hip joint pain, inguinal hernia, GTPS, femoral neuropathy. | |ddx=L2 or L3 radiculopathy, pelvic mass, superior gluteal nerve entrapment, hip joint pain, inguinal hernia, GTPS, femoral neuropathy. | ||
|treatment=Conservative management, injection. | |treatment=Conservative management, injection. | ||
}} | }} | ||
| Line 27: | Line 22: | ||
The LFCN can be injured anywhere along its course, either in the retroperitoneum or pelvis. Nevertheless, there are two common areas of entrapment. | The LFCN can be injured anywhere along its course, either in the retroperitoneum or pelvis. Nevertheless, there are two common areas of entrapment. | ||
*The iliopubic tract (IPT): This is a region of dense connective tissue. It is at the junction of the anterior lamina of the iliac fascia, and the transversalis fascia that invests the transversus abdominis. The LFCN always courses deep to and adjacent to the IPT. Pseudo-neuromas can form proximal to the IPT and is a clue for compression at this site. | *The iliopubic tract (IPT): This is a region of dense connective tissue. It is at the junction of the anterior lamina of the iliac fascia, and the transversalis fascia that invests the transversus abdominis. The LFCN always courses deep to and adjacent to the IPT. Pseudo-neuromas can form proximal to the IPT and is a clue for compression at this site. | ||
*Passage from pelvis to thigh: The nerve makes a 100 ± 10° turn as it passes into the thigh. This makes it susceptible to entrapment, compression, and traction injury. The angle increases with movement and hip extension. Notably, lithotomy position with hip flexion and abduction does not increase the strain on the LFCN. There is increased risk of entrapment at this site with obesity, pregnancy, ascites, tight clothing, seat belts, braces, scoliosis, direct trauma, leg length discrepancy, and muscle spasm.<ref name="trescot"/> | *Passage from pelvis to thigh: The nerve makes a 100 ± 10° turn as it passes into the thigh. This makes it susceptible to entrapment, compression, and traction injury. The angle increases with movement and hip extension. Notably, lithotomy position with hip flexion and abduction does not increase the strain on the LFCN. There is increased risk of entrapment at this site with obesity, pregnancy, ascites, tight clothing, seat belts, braces, scoliosis, direct trauma, [[Leg Length Discrepancy|leg length discrepancy]], and muscle spasm.<ref name="trescot" /> | ||
Meralgia paraesthetica has been described in all anatomical variations of the LFCN. However, it is most susceptible with the following nerve courses: posterior to the ASIS across the iliac crest, medial to the iliac crest superficial to sartorius origin, and medial to the ASIS within the sartorius. LFCN entrapment is less likely with its more medial variants. Repetitive trauma to the LFCN can be indicated by significant enlargement proximal to the inguinal ligament, or pseudo-neuromas (pseudo-ganglions) at the inguinal ligament.<ref name="trescot"/> | Meralgia paraesthetica has been described in all anatomical variations of the LFCN. However, it is most susceptible with the following nerve courses: posterior to the ASIS across the iliac crest, medial to the iliac crest superficial to sartorius origin, and medial to the ASIS within the sartorius. LFCN entrapment is less likely with its more medial variants. Repetitive trauma to the LFCN can be indicated by significant enlargement proximal to the inguinal ligament, or pseudo-neuromas (pseudo-ganglions) at the inguinal ligament.<ref name="trescot" /> | ||
==Epidemiology and Risk Factors== | ==Epidemiology and Risk Factors== | ||
Nontraumatic MP has an incidence of 3.4–4.3/10,000 person-years. It is significantly linked to carpal tunnel syndrome, pregnancy, obesity, and diabetes mellitus (DM). Diabetes mellitus confers a 7 times higher rate of MP. Conversely, for those without DM, patients with MP are twice as likely to be lateral diagnosed with DM. There is a male predominance.<ref name="trescot"/> | Nontraumatic MP has an incidence of 3.4–4.3/10,000 person-years. It is significantly linked to carpal tunnel syndrome, pregnancy, obesity, and diabetes mellitus (DM). Diabetes mellitus confers a 7 times higher rate of MP. Conversely, for those without DM, patients with MP are twice as likely to be lateral diagnosed with DM. There is a male predominance.<ref name="trescot" /> | ||
==Clinical Features== | ==Clinical Features== | ||
| Line 44: | Line 39: | ||
===History=== | ===History=== | ||
Symptoms are classically subacute on onset, and involve burning pain, dysaesthesia (paraesthesia and hypoaesthesia), or both. The affected area is the anterolateral thigh. Pain can be felt anywhere from the anterior to the lateral hip, the anterior and lateral thigh, and distally down to the anterior knee. Some patients feel a coldness, deep muscle aching, profoundly reduced sensation, or hair loss in the area due to stroking it. The symptoms are purely sensory in nature, because the LFCN doesn't have any motor fibres. Symptoms tend to be aggravated by prolonged standing and walking. Relieving factors are typically sitting down, but some patients describe sitting worsening the pain. Patients may modify their gait to reduce symptoms and develop secondary hip, knee, and calf pain.<ref name="trescot"/> | Symptoms are classically subacute on onset, and involve burning pain, dysaesthesia (paraesthesia and hypoaesthesia), or both. The affected area is the anterolateral thigh. Pain can be felt anywhere from the anterior to the lateral hip, the anterior and lateral thigh, and distally down to the anterior knee. Some patients feel a coldness, deep muscle aching, profoundly reduced sensation, or hair loss in the area due to stroking it. The symptoms are purely sensory in nature, because the LFCN doesn't have any motor fibres. Symptoms tend to be aggravated by prolonged standing and walking. Relieving factors are typically sitting down, but some patients describe sitting worsening the pain. Patients may modify their gait to reduce symptoms and develop secondary hip, knee, and calf pain.<ref name="trescot" /> | ||
The clinician should thoroughly assess for red flag symptoms that could suggest something more sinister such as tumours and vasculitis (see differential diagnosis below). | The clinician should thoroughly assess for red flag symptoms that could suggest something more sinister such as tumours and vasculitis (see differential diagnosis below). | ||
The occupational, exercise, and trauma history that is relevant to LFCNE is below.<ref name="trescot">Trescot, Andrea. Peripheral nerve entrapments : clinical diagnosis and management. Switzerland: Springer, 2016.</ref> | The occupational, exercise, and trauma history that is relevant to LFCNE is below.<ref name="trescot">Trescot, Andrea. Peripheral nerve entrapments : clinical diagnosis and management. Switzerland: Springer, 2016.</ref> | ||
{| class=" | {| class="plaintable" | ||
|- | |- | ||
! Category !! History | !Category!!History | ||
|- | |- | ||
|rowspan="8"| Compression | | rowspan="8" |Compression | ||
|| Obesity | ||Obesity | ||
|- | |- | ||
|| Pregnancy | ||Pregnancy | ||
|- | |- | ||
|| Abdominal masses (uterine myoma, retroperitoneal lipofibrosarcoma) | ||Abdominal masses (uterine myoma, retroperitoneal lipofibrosarcoma) | ||
|- | |- | ||
|| Ascites, large abdomen | ||Ascites, large abdomen | ||
|- | |- | ||
|| Tight garments or seat belts, especially in thin individuals | ||Tight garments or seat belts, especially in thin individuals | ||
|- | |- | ||
|| Leg length discrepancy | ||[[Leg Length Discrepancy|Leg length discrepancy]] | ||
|- | |- | ||
|| Lumbar herniated disk | ||Lumbar herniated disk | ||
|- | |- | ||
|| Psoas tumor/infection/spasm | ||Psoas tumor/infection/spasm | ||
|- | |- | ||
|rowspan="1"|Trauma | | rowspan="1" |Trauma | ||
||“Hip-checked” | ||“Hip-checked” | ||
|- | |- | ||
|rowspan="7"|Surgery | | rowspan="7" |Surgery | ||
||Laparoscopic appendectomy, cholecystectomy, hernia repair | ||Laparoscopic appendectomy, cholecystectomy, hernia repair | ||
|- | |- | ||
| Line 88: | Line 83: | ||
||Ilioinguinal repair of a pelvic fracture | ||Ilioinguinal repair of a pelvic fracture | ||
|- | |- | ||
|rowspan="4"|Infection/inflammation | | rowspan="4" |Infection/inflammation | ||
||Diabetes mellitus | ||Diabetes mellitus | ||
|- | |- | ||
| Line 97: | Line 92: | ||
||Appendicitis | ||Appendicitis | ||
|- | |- | ||
|rowspan="1"|Exercise | | rowspan="1" |Exercise | ||
||Strenuous abdominal or lower body exercise | ||Strenuous abdominal or lower body exercise | ||
|} | |} | ||
===Examination=== | ===Examination=== | ||
The patient should have characteristic sensory changes over the anterolateral thigh, without any motor findings or reflex abnormalities. There may be reduced sensation to cold and pin prick over the affected area. Due to anatomical variations, abnormalities may be present only over the lateral thigh. There may be tenderness and a positive Tinel's sign adjacent to the ASIS. The most reliable physical finding is ASIS tenderness. Standing, lying straight, and hip extension may be provocative. Sitting or lateral pelvic compression may relieve the pain. Screening hip, lumbar, and sacroiliac joint examinations should be performed.<ref name="trescot"/> | [[File:Lateral femoral cutaneous nerve skin innervation.png|thumb|right|100px|Cutaneous distribution of the LFCN]] | ||
The patient should have characteristic sensory changes over the anterolateral thigh, without any motor findings or reflex abnormalities. There may be reduced sensation to cold and pin prick over the affected area. Due to anatomical variations, abnormalities may be present only over the lateral thigh. There may be tenderness and a positive Tinel's sign adjacent to the ASIS. The most reliable physical finding is ASIS tenderness. Standing, lying straight, and hip extension may be provocative. Sitting or lateral pelvic compression may relieve the pain. Screening hip, lumbar, and sacroiliac joint examinations should be performed.<ref name="trescot" /> | |||
==Investigations== | ==Investigations== | ||
===Imaging=== | ===Imaging=== | ||
;Radiographs | ;Radiographs | ||
:Usually unnecessary when symptoms and signs are classical and there are no red flags. X-rays can be helpful in detecting spondylolisthesis, spinal stenosis, and disc disease. | :Usually unnecessary when symptoms and signs are classical and there are no red flags. X-rays can be helpful in detecting [[spondylolisthesis]], spinal stenosis, and disc disease. | ||
;MRI | ;MRI | ||
:Can evaluate for space-occupying lesions compressing the LFCN, and showing peripheral nerve changes in clinically uncertain cases. It is rare to see the LFCN on axial views because it has a nearly horizontal intrapelvic course where it runs along the anterior surface of the iliacus. Once it leaves the pelvis it can be seen on axial views. 3T MRI has a 94% predictive value in diagnosing meralgia paraesthetica. | :Can evaluate for space-occupying lesions compressing the LFCN, and showing peripheral nerve changes in clinically uncertain cases. It is rare to see the LFCN on axial views because it has a nearly horizontal intrapelvic course where it runs along the anterior surface of the iliacus. Once it leaves the pelvis it can be seen on axial views. 3T MRI has a 94% predictive value in diagnosing meralgia paraesthetica. | ||
| Line 116: | Line 112: | ||
==Diagnosis== | ==Diagnosis== | ||
The diagnosis can usually be made on classical history and examination findings. If there is doubt a diagnostic ultrasound guided [[Lateral Femoral Cutaneous Nerve Injection|LFCN injection]] can be done. | The diagnosis can usually be made on classical history and examination findings. If there is doubt then a diagnostic ultrasound guided [[Lateral Femoral Cutaneous Nerve Injection|LFCN injection]] and/or MRI can be done. | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
! Differential !! Features | !Differential!!Features | ||
|- | |- | ||
| L2 or L3 radiculopathy || Low back pain, sensory and/or motor abnormalities below the knee, MRI findings of disc herniation. | |L2 or L3 radiculopathy||Low back pain, sensory and/or motor abnormalities below the knee, MRI findings of disc herniation. | ||
|- | |- | ||
| Pelvic or iliac crest mass || Tumour history, genetic risk (HNPCC, BRCA), bloating, constitutional symptoms, palpable pelvic mass, MRI or US findings | |Pelvic or iliac crest mass||Tumour history, genetic risk (HNPCC, BRCA), bloating, constitutional symptoms, palpable pelvic mass, MRI or US findings | ||
|- | |- | ||
| Chronic appendicitis || RLQ pain, constitutional symptoms, CT or US findings | |Chronic appendicitis||RLQ pain, constitutional symptoms, CT or US findings | ||
|- | |- | ||
| Superior gluteal nerve entrapment || Pain from the lateral buttock down to the knee, tender mid-lateral buttock; no sensory abnormalities | |Superior gluteal nerve entrapment||Pain from the lateral buttock down to the knee, tender mid-lateral buttock; no sensory abnormalities | ||
|- | |- | ||
| Femoral neuropathy || Quadriceps weakness | |Femoral neuropathy||Quadriceps weakness | ||
|- | |- | ||
| Hemangioma of pelvis || Seen on imaging | |Hemangioma of pelvis||Seen on imaging | ||
|- | |- | ||
| Inguinal hernia | |Inguinal hernia||Detected on examination, seen on standing if small, positive cough impulse | ||
|- | |- | ||
| Hip joint pain || Restricted range of motion, pain referred to medial thigh, x-ray findings of osteoarthritis. | |Hip joint pain||Restricted range of motion, pain referred to medial thigh, x-ray findings of osteoarthritis. | ||
|- | |- | ||
| Greater trochanteric pain syndrome || Lateral thigh pain, Greater trochanteric or hip abductor tenderness, pain relief after local anaesthetic injection, | |Greater trochanteric pain syndrome||Lateral thigh pain, Greater trochanteric or hip abductor tenderness, pain relief after local anaesthetic injection, | ||
|} | |} | ||
The clinician must consider other pathologies such as those in the abdomen, lumbar spine, pelvis, and hip. There are also a variety of different peripheral nerve entrapments that can cause thigh pain. Red flag conditions to consider include pelvic masses, chronic appendicitis, caecal tumours, and retroperitoneal sarcomas. These can all cause pain and dysaesthesia in the LFCN distribution. Other conditions that can cause symptoms are haemangiomas, uterine myomas, periostitis, and traction during retroperitoneal procedures.<ref name="trescot"/> | The clinician must consider other pathologies such as those in the abdomen, lumbar spine, pelvis, and hip. There are also a variety of different peripheral nerve entrapments that can cause thigh pain. Red flag conditions to consider include pelvic masses, chronic appendicitis, caecal tumours, and retroperitoneal sarcomas. These can all cause pain and dysaesthesia in the LFCN distribution. Other conditions that can cause symptoms are haemangiomas, uterine myomas, periostitis, and traction during retroperitoneal procedures.<ref name="trescot" /> | ||
Any entrapment neuropathy must be differentiated from other mononeuropathies especially vasculitis where the nerve can become ischaemic or infarct. Vasculitis is usually acute in onset and is usually self-resolves over 6 weeks. Entrapment neuropathies generally start slowly, are gradually progressive, and persistent.<ref name="trescot"/> | Any entrapment neuropathy must be differentiated from other mononeuropathies especially vasculitis where the nerve can become ischaemic or infarct. Vasculitis is usually acute in onset and is usually self-resolves over 6 weeks. Entrapment neuropathies generally start slowly, are gradually progressive, and persistent.<ref name="trescot" /> | ||
Lumbar radiculopathy can cause leg numbness, but it is very unusual for it to cause sensory changes such a localised area seen in LFCN entrapment. Also back/buttock pain are often present. However, LFCN irritation can refer pain both distally, and proximally into the buttock, which could lead to an incorrect diagnosis of lumbar radiculopathy.<ref name="trescot"/> | Lumbar radiculopathy can cause leg numbness, but it is very unusual for it to cause sensory changes such a localised area seen in LFCN entrapment. Also back/buttock pain are often present. However, LFCN irritation can refer pain both distally, and proximally into the buttock, which could lead to an incorrect diagnosis of lumbar radiculopathy.<ref name="trescot" /> | ||
==Treatment== | ==Treatment== | ||
Assuming there is no red flag condition, then modifiable factors should be addressed. Most patients can achieve good pain relief from non-interventional treatment and NSAIDs. The most important modifiable factor is weight loss in those with large abdomens. The patient should be instructed to avoid tight belts or clothes around the waist. Good glucose control should be achieved in diabetes. Alcohol intake should be minimised. If the patient does a lot of long-distance walking or cycling then this could be stopped for a short period. Neuromodulatory such as TCAs drugs can be considered. Topical local anaesthetics and TENS are sometimes helpful.<ref name="trescot"/> | Assuming there is no red flag condition, then modifiable factors should be addressed. Most patients can achieve good pain relief from non-interventional treatment and NSAIDs. The most important modifiable factor is weight loss in those with large abdomens. The patient should be instructed to avoid tight belts or clothes around the waist. Good glucose control should be achieved in diabetes. Alcohol intake should be minimised. If the patient does a lot of long-distance walking or cycling then this could be stopped for a short period. Neuromodulatory such as TCAs drugs can be considered. Topical local anaesthetics and TENS are sometimes helpful.<ref name="trescot" /> | ||
;Injections | ;Injections | ||
:[[Lateral Femoral Cutaneous Nerve Injection|Lateral femoral cutaneous nerve injection]] can be performed as both a diagnostic and therapeutic intervention. Injection can be considered for symptoms that persist for 1-2 months in spite of conservative measures.<ref name="trescot"/> | :[[Lateral Femoral Cutaneous Nerve Injection|Lateral femoral cutaneous nerve injection]] can be performed as both a diagnostic and therapeutic intervention. Injection can be considered for symptoms that persist for 1-2 months in spite of conservative measures. In some cases repeated injections are required.<ref name="trescot" /> | ||
;Neurolysis | ;Neurolysis | ||
:More invasive procedures such as radiofrequency neurotomy has been described but is not done in NZ to the authors knowledge. Neurolysis causes persistent numbness and has a risk of anaeesthesia dolorosa. There is also a risk of damage to the surrounding femoral and obturator nerves.<ref name="trescot"/> | :More invasive procedures such as radiofrequency neurotomy has been described but is not done in NZ to the authors knowledge. Neurolysis causes persistent numbness and has a risk of anaeesthesia dolorosa. There is also a risk of damage to the surrounding femoral and obturator nerves.<ref name="trescot" /> | ||
;Surgery | ;Surgery | ||
:Surgical decompression has been described but it is not universally successful and recurrence can still occur.<ref name="trescot"/> | :Surgical decompression has been described but it is not universally successful and recurrence can still occur.<ref name="trescot" /> | ||
==Follow Up and Prognosis== | ==Follow Up and Prognosis== | ||
Assuming there is no red flag condition, the condition is often treatable, but recurrence is common.<ref name="trescot"/> | Assuming there is no red flag condition, the condition is often treatable, but recurrence is common.<ref name="trescot" /> | ||
==Summary== | ==Summary== | ||
| Line 170: | Line 166: | ||
==References== | ==References== | ||
<references/> | <references /> | ||
[[Category:Pelvis, Hip and Thigh Conditions]] | |||
{{References}} | |||
[[Category:Pelvis, Hip | {{Reliable sources | ||
|synonym1="meralgia paresthetica" | |||
|synonym2="meralgia paraesthetica" | |||
}} | |||
Latest revision as of 09:58, 17 April 2022
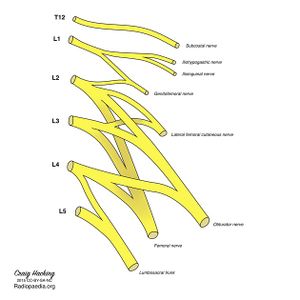
The lateral femoral cutaneous nerve (LFCN) is a pure sensory nerve that is vulnerable to compression. Its course begins at the lumbosacral plexus, travels down through the retroperitoneum, under the inguinal ligament, and into the subcutaneous tissue of the thigh. Meralgia paraesthetica (MP), also known as Bernhardt-Roth syndrome refers to nerve compression causing the clinical syndrome of pain, dysaesthesia, or both in the anterolateral thigh. MP was first described by Werner Hager in 1885. It was later named "meralgia," with the etymology stemming from the Greek words "meros" (thigh), and "algos" (pain). This article deals with the clinical syndrome of LFCN entrapment. Full discussion of injection treatments and the anatomy are discussed elsewhere (See Lateral Femoral Cutaneous Nerve Injection and Lateral Femoral Cutaneous Nerve.)
Aetiopathophysiology
The LFCN can be injured anywhere along its course, either in the retroperitoneum or pelvis. Nevertheless, there are two common areas of entrapment.
- The iliopubic tract (IPT): This is a region of dense connective tissue. It is at the junction of the anterior lamina of the iliac fascia, and the transversalis fascia that invests the transversus abdominis. The LFCN always courses deep to and adjacent to the IPT. Pseudo-neuromas can form proximal to the IPT and is a clue for compression at this site.
- Passage from pelvis to thigh: The nerve makes a 100 ± 10° turn as it passes into the thigh. This makes it susceptible to entrapment, compression, and traction injury. The angle increases with movement and hip extension. Notably, lithotomy position with hip flexion and abduction does not increase the strain on the LFCN. There is increased risk of entrapment at this site with obesity, pregnancy, ascites, tight clothing, seat belts, braces, scoliosis, direct trauma, leg length discrepancy, and muscle spasm.[1]
Meralgia paraesthetica has been described in all anatomical variations of the LFCN. However, it is most susceptible with the following nerve courses: posterior to the ASIS across the iliac crest, medial to the iliac crest superficial to sartorius origin, and medial to the ASIS within the sartorius. LFCN entrapment is less likely with its more medial variants. Repetitive trauma to the LFCN can be indicated by significant enlargement proximal to the inguinal ligament, or pseudo-neuromas (pseudo-ganglions) at the inguinal ligament.[1]
Epidemiology and Risk Factors
Nontraumatic MP has an incidence of 3.4–4.3/10,000 person-years. It is significantly linked to carpal tunnel syndrome, pregnancy, obesity, and diabetes mellitus (DM). Diabetes mellitus confers a 7 times higher rate of MP. Conversely, for those without DM, patients with MP are twice as likely to be lateral diagnosed with DM. There is a male predominance.[1]
Clinical Features
- Genetic risk - strong family history of HNPCC or BRCA mutation
- Pelvic mass
- Unexplained weight loss and/or constitutional symptoms
- Onset of pain after menopause
- Irregular vaginal bleeding after age 40 years and/or postcoital bleeding
History
Symptoms are classically subacute on onset, and involve burning pain, dysaesthesia (paraesthesia and hypoaesthesia), or both. The affected area is the anterolateral thigh. Pain can be felt anywhere from the anterior to the lateral hip, the anterior and lateral thigh, and distally down to the anterior knee. Some patients feel a coldness, deep muscle aching, profoundly reduced sensation, or hair loss in the area due to stroking it. The symptoms are purely sensory in nature, because the LFCN doesn't have any motor fibres. Symptoms tend to be aggravated by prolonged standing and walking. Relieving factors are typically sitting down, but some patients describe sitting worsening the pain. Patients may modify their gait to reduce symptoms and develop secondary hip, knee, and calf pain.[1]
The clinician should thoroughly assess for red flag symptoms that could suggest something more sinister such as tumours and vasculitis (see differential diagnosis below).
The occupational, exercise, and trauma history that is relevant to LFCNE is below.[1]
| Category | History |
|---|---|
| Compression | Obesity |
| Pregnancy | |
| Abdominal masses (uterine myoma, retroperitoneal lipofibrosarcoma) | |
| Ascites, large abdomen | |
| Tight garments or seat belts, especially in thin individuals | |
| Leg length discrepancy | |
| Lumbar herniated disk | |
| Psoas tumor/infection/spasm | |
| Trauma | “Hip-checked” |
| Surgery | Laparoscopic appendectomy, cholecystectomy, hernia repair |
| Iliac crest graft | |
| Lumbar sympathetic block or neurolysis | |
| Femoral artery catheterization | |
| Occurs in 20 % of spinal surgeries | |
| Total hip arthroplasty | |
| Ilioinguinal repair of a pelvic fracture | |
| Infection/inflammation | Diabetes mellitus |
| Periostitis of the ilium | |
| Retrocecal tumor | |
| Appendicitis | |
| Exercise | Strenuous abdominal or lower body exercise |
Examination
The patient should have characteristic sensory changes over the anterolateral thigh, without any motor findings or reflex abnormalities. There may be reduced sensation to cold and pin prick over the affected area. Due to anatomical variations, abnormalities may be present only over the lateral thigh. There may be tenderness and a positive Tinel's sign adjacent to the ASIS. The most reliable physical finding is ASIS tenderness. Standing, lying straight, and hip extension may be provocative. Sitting or lateral pelvic compression may relieve the pain. Screening hip, lumbar, and sacroiliac joint examinations should be performed.[1]
Investigations
Imaging
- Radiographs
- Usually unnecessary when symptoms and signs are classical and there are no red flags. X-rays can be helpful in detecting spondylolisthesis, spinal stenosis, and disc disease.
- MRI
- Can evaluate for space-occupying lesions compressing the LFCN, and showing peripheral nerve changes in clinically uncertain cases. It is rare to see the LFCN on axial views because it has a nearly horizontal intrapelvic course where it runs along the anterior surface of the iliacus. Once it leaves the pelvis it can be seen on axial views. 3T MRI has a 94% predictive value in diagnosing meralgia paraesthetica.
Nerve Conduction Studies
Sensory nerve conduction study results are highly variable. They are also technically difficult due to the variation in location of the LFCN, and the increased body habitus of the typical patient. Electromyography is not generally indicated because there are no motor fibres, however combined EMG and NCS can be used on occasion to evaluate for radiculopathy and plexopathy.
Diagnosis
The diagnosis can usually be made on classical history and examination findings. If there is doubt then a diagnostic ultrasound guided LFCN injection and/or MRI can be done.
Differential Diagnosis
| Differential | Features |
|---|---|
| L2 or L3 radiculopathy | Low back pain, sensory and/or motor abnormalities below the knee, MRI findings of disc herniation. |
| Pelvic or iliac crest mass | Tumour history, genetic risk (HNPCC, BRCA), bloating, constitutional symptoms, palpable pelvic mass, MRI or US findings |
| Chronic appendicitis | RLQ pain, constitutional symptoms, CT or US findings |
| Superior gluteal nerve entrapment | Pain from the lateral buttock down to the knee, tender mid-lateral buttock; no sensory abnormalities |
| Femoral neuropathy | Quadriceps weakness |
| Hemangioma of pelvis | Seen on imaging |
| Inguinal hernia | Detected on examination, seen on standing if small, positive cough impulse |
| Hip joint pain | Restricted range of motion, pain referred to medial thigh, x-ray findings of osteoarthritis. |
| Greater trochanteric pain syndrome | Lateral thigh pain, Greater trochanteric or hip abductor tenderness, pain relief after local anaesthetic injection, |
The clinician must consider other pathologies such as those in the abdomen, lumbar spine, pelvis, and hip. There are also a variety of different peripheral nerve entrapments that can cause thigh pain. Red flag conditions to consider include pelvic masses, chronic appendicitis, caecal tumours, and retroperitoneal sarcomas. These can all cause pain and dysaesthesia in the LFCN distribution. Other conditions that can cause symptoms are haemangiomas, uterine myomas, periostitis, and traction during retroperitoneal procedures.[1]
Any entrapment neuropathy must be differentiated from other mononeuropathies especially vasculitis where the nerve can become ischaemic or infarct. Vasculitis is usually acute in onset and is usually self-resolves over 6 weeks. Entrapment neuropathies generally start slowly, are gradually progressive, and persistent.[1]
Lumbar radiculopathy can cause leg numbness, but it is very unusual for it to cause sensory changes such a localised area seen in LFCN entrapment. Also back/buttock pain are often present. However, LFCN irritation can refer pain both distally, and proximally into the buttock, which could lead to an incorrect diagnosis of lumbar radiculopathy.[1]
Treatment
Assuming there is no red flag condition, then modifiable factors should be addressed. Most patients can achieve good pain relief from non-interventional treatment and NSAIDs. The most important modifiable factor is weight loss in those with large abdomens. The patient should be instructed to avoid tight belts or clothes around the waist. Good glucose control should be achieved in diabetes. Alcohol intake should be minimised. If the patient does a lot of long-distance walking or cycling then this could be stopped for a short period. Neuromodulatory such as TCAs drugs can be considered. Topical local anaesthetics and TENS are sometimes helpful.[1]
- Injections
- Lateral femoral cutaneous nerve injection can be performed as both a diagnostic and therapeutic intervention. Injection can be considered for symptoms that persist for 1-2 months in spite of conservative measures. In some cases repeated injections are required.[1]
- Neurolysis
- More invasive procedures such as radiofrequency neurotomy has been described but is not done in NZ to the authors knowledge. Neurolysis causes persistent numbness and has a risk of anaeesthesia dolorosa. There is also a risk of damage to the surrounding femoral and obturator nerves.[1]
- Surgery
- Surgical decompression has been described but it is not universally successful and recurrence can still occur.[1]
Follow Up and Prognosis
Assuming there is no red flag condition, the condition is often treatable, but recurrence is common.[1]
Summary
- The LFCN has variable anatomy and therefore clinical presentation
- Symptoms may be classic - pain and/or dysaesthesia affecting the cutaneous distribution of the LFCN.
- There is a strong association with diabetes mellitus
- Most cases can be managed with conservative management.
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,