Lateral Femoral Cutaneous Nerve Entrapment
| Lateral Femoral Cutaneous Nerve Entrapment |
|---|
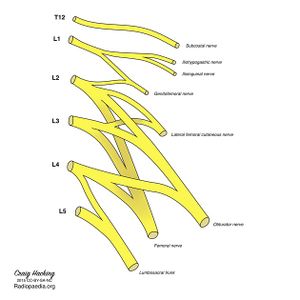
The lateral femoral cutaneous nerve (LFCN) is a pure sensory nerve that is vulnerable to compression. Its course begins at the lumbosacral plexus, travels down through the retroperitoneum, under the inguinal ligament, and into the subcutaneous tissue of the thigh. Meralgia paraesthetica (MP), also known as Bernhardt-Roth syndrome refers to nerve compression causing the clinical syndrome of pain, dysaesthesia, or both in the anterolateral thigh. MP was first described by Werner Hager in 1885. It was later named "meralgia," with the etymology stemming from the Greek words "meros" (thigh), and "algos" (pain). This article deals with the clinical syndrome of LFCN entrapment. Full discussion of injection treatments and the anatomy are discussed elsewhere (See Lateral Femoral Cutaneous Nerve Injection and Lateral Femoral Cutaneous Nerve.)
Aetiopathophysiology
The LFCN can be injured anywhere along its course, either in the retroperitoneum or pelvis. Nevertheless, there are two common areas of entrapment.
- The iliopubic tract (IPT): This is a region of dense connective tissue. It is at the junction of the anterior lamina of the iliac fascia, and the transversalis fascia that invests the transversus abdominis. The LFCN always courses deep to and adjacent to the IPT. Pseudo-neuromas can form proximal to the IPT and is a clue for compression at this site.
- Passage from pelvis to thigh: The nerve makes a 100 ± 10° turn as it passes into the thigh. This makes it susceptible to entrapment, compression, and traction injury. The angle increases with movement and hip extension. Notably, lithotomy position with hip flexion and abduction does not increase the strain on the LFCN. There is increased risk of entrapment at this site with obesity, pregnancy, ascites, tight clothing, seat belts, braces, scoliosis, direct trauma, leg length discrepancy, and muscle spasm.[1]
Meralgia paraesthetica has been described in all anatomical variations of the LFCN. However, it is most susceptible with the following nerve courses: posterior to the ASIS across the iliac crest, medial to the iliac crest superficial to sartorius origin, and medial to the ASIS within the sartorius. LFCN entrapment is less likely with its more medial variants. Repetitive trauma to the LFCN can be indicated by significant enlargement proximal to the inguinal ligament, or pseudo-neuromas (pseudo-ganglions) at the inguinal ligament.[1]
Epidemiology and Risk Factors
Nontraumatic MP has an incidence of 3.4–4.3/10,000 person-years. It is significantly linked to carpal tunnel syndrome, pregnancy, obesity, and diabetes mellitus (DM). Diabetes mellitus confers a 7 times higher rate of MP. Conversely, for those without DM, patients with MP are twice as likely to be lateral diagnosed with DM. There is a male predominance.[1]
Clinical Features
History
Symptoms are classically subacute on onset, and involve burning pain, dysaesthesia (paraesthesia and hypoaesthesia), or both. The affected area is the anterolateral thigh. Pain can be felt anywhere from the anterior to the lateral hip, the anterior and lateral thigh, and distally down to the anterior knee. Some patients feel a coldness, deep muscle aching, profoundly reduced sensation, or hair loss in the area due to stroking it. The symptoms are purely sensory in nature, because the LFCN doesn't have any motor fibres. Symptoms tend to be aggravated by prolonged standing and walking. Relieving factors are typically sitting down, but some patients describe sitting worsening the pain. Patients may modify their gait to reduce symptoms and develop secondary hip, knee, and calf pain.[1]
The clinician should thoroughly assess for red flag symptoms that could suggest something more sinister such as tumours and vasculitis (see differential diagnosis below).
The occupational, exercise, and trauma history that is relevant to LFCNE is below.[1]
- Compression
- Obesity
- Pregnancy
- Abdominal masses (uterine myoma, retroperitoneal lipofibrosarcoma)
- Ascites, large abdomen
- Tight garments or seat belts, especially in thin individuals
- Leg length discrepancy
- Lumbar herniated disk
- Psoas tumor/infection/spasm
- Trauma
- “Hip-checked”
- Surgery
- Laparoscopic appendectomy, cholecystectomy, hernia repair
- Iliac crest graft
- Lumbar sympathetic block or neurolysis
- Femoral artery catheterization
- Occurs in 20 % of spinal surgeries
- Total hip arthroplasty
- Ilioinguinal repair of a pelvic fracture
- Infection/inflammation
- Diabetes mellitus
- Periostitis of the ilium
- Retrocecal tumor
- Appendicitis
- Exercise
- Strenuous abdominal or lower body exercise
Examination
The patient should have characteristic sensory changes over the anterolateral thigh, without any motor findings or reflex abnormalities. There may be reduced sensation to cold and pin prick over the affected area. Due to anatomical variations, abnormalities may be present only over the lateral thigh. There may be tenderness and a positive Tinel's sign adjacent to the ASIS. The most reliable physical finding is ASIS tenderness. Standing, lying straight, and hip extension may be provocative. Sitting or lateral pelvic compression may relieve the pain. Screening hip, lumbar, and sacroiliac joint examinations should be performed.[1]
Investigations
- Radiographs
- Usually unnecessary when symptoms and signs are classical and there are no red flags. X-rays can be helpful in detecting spondylolisthesis, spinal stenosis, and disc disease.
- MRI
- Can evaluate for space-occupying lesions compressing the LFCN, and showing peripheral nerve changes in clinically uncertain cases. It is rare to see the LFCN on axial views because it has a nearly horizontal intrapelvic course where it runs along the anterior surface of the iliacus. Once it leaves the pelvis it can be seen on axial views. 3T MRI has a 94% predictive value in diagnosing meralgia paraesthetica.
Imaging Findings
Other Investigations
Diagnosis
Differential Diagnosis
Treatment
Lateral Femoral Cutaneous Nerve Injection
Follow Up and Prognosis
Summary
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,