Lateral Femoral Cutaneous Nerve Injection
| |
| Lateral Femoral Cutaneous Nerve Injection | |
|---|---|
| Indication | Lateral femoral cutaneous nerve entrapment or meralgia paraesthetica |
| Needle | 21-22 gauge 40mm if using landmark guidance "pop" technique |
| Injectate | dextrose 5%, steroid. |
| Steroid | 20mg triamcinolone optional |
| Local | Less for landmark guided. |
The lateral femoral cutaneous nerve (LFCN) of the thigh has a variable anatomical course. The clinical presentation with a pathological nerve can be varied. There is a strong association with LFCN entrapment and meralgia paraesthetica with diabetes mellitus. If clinically necessary, injection under ultrasound guidance is recommended over landmark guidance if available. This article deals with the the injection treatment of LFCN entrapment (meralgia paraesthetica). Full discussion of the clinical syndrome and the anatomy are discussed elsewhere (See Lateral Femoral Cutaneous Nerve Entrapment and Lateral Femoral Cutaneous Nerve.
Anatomy
- Main article: Lateral Femoral Cutaneous Nerve
The LFCN has a highly variable course. This is especially true as it moves from the pelvis into the thigh. It originates from L2 and L3, and is part of the lumbar plexus. It courses obliquely between the superficial and deep parts of the psoas muscle, and between the two layers of fascia over the surface of the iliacus muscle. It then passes through an aponeuroticofascial tunnel that runs from the iliopubic tract down to the inguinal ligament, under the inguinal ligament, or through a split in its lateral aspect at the ASIS. It travels under the deep circumflex iliac vessels as it approaches the ASIS. It then exits into the thigh.[1]
The LFCN can cross into the thigh at a point 6cm medial to the ASIS to 2cm lateral to the ASIS. It can run superficial or through the sartorius muscle. Or it can cross over the iliac crest lateral and posterior to the ASIS. In this position it is particularly susceptible to external pressure from clothing.[1]
The LFCN typically has two branches. There is the smaller posterior branch which supplies the greater trochanter area. There is secondly the larger anterior branch which supplies the anterolateral thigh to the knee. It can exit the pelvis in up to five branches. Entrapment of any one of these branches can cause entrapment symptoms.[1]
Indications
- Main article: Lateral Femoral Cutaneous Nerve Entrapment
Patients where symptoms have persisted for 1-2 months despite conservative treatment. It can also be helpful in confirming the diagnosis. If neurotomy is being considered it is an important step for both diagnostic confirmation and for the patient to experience the expected result.
Contraindications
Pre-procedural Evaluation
Full clinical assessment should be performed. On history the patient may be able to trace the affected area, and may use neuropathic pain descriptors when describing the sensation. The patient should have characteristic sensory changes over the anterolateral thigh, without any motor findings. There may be tenderness and a positive Tinel's sign adjacent to the ASIS. Hip extension may be provocative. There may be reduced sensation to cold and pin prick over the affected area.
Equipment
Technique
Ultrasound Guided
Ultrasound allows direct visualisation of the LFCN thereby surmounting the problem of anatomical variability. The nerve can be traced from the ASIS down to the inguinal region to identify the best transverse view. It allows safe injection avoiding needle trauma and can confirm injection location around the nerve. Ultrasound reduces patient discomfort. It reduces the amount of local anaesthetic required. It reduces the risk of inadvertent blockade of all three of the femoral, obturator, and LFC nerves (3-in-1 block).[1]
- Position: Patient supine.
- Palpate the ASIS.
- Use a high frequency linear probe (the nerve is very superficial).
- Place the lateral end of the probe on the ASIS, and the medial end angled slightly caudally. The probe should be parallel with the inguinal ligament.
- Visualise the ASIS as a hyperechoic bony structure with shadowing.
- Move the probe inferiorly to the ASIS at the sartorius insertion site.
- Move the probe medially and inferiorly below the inguinal ligament, and visualise two continuous hyperechoic lines under the subcutaneous tissue. These are the fascia lata, and fascia iliaca. They are generally 0.5-1cm apart.
- The LFCN is seen axially between these two fascial layers. It looks hyperechoic, elliptical, fibrillar, and looks like an "eye."
- Alternatively, place the medial end of the probe angled slightly caudally, so the probe is parallel to the inguinal ligament. Here the LFCN looks oval on short axes, and tubular longitudinally.
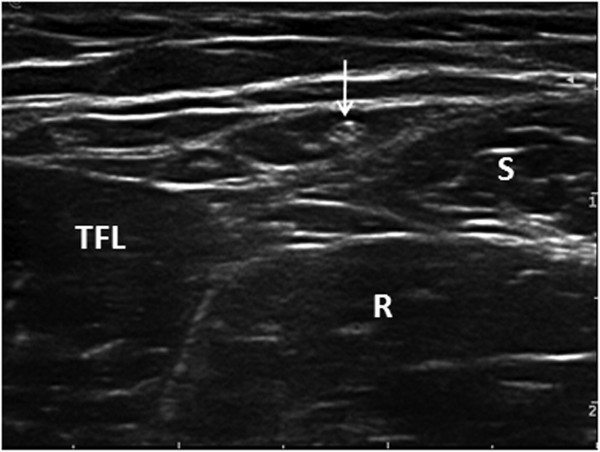
- If there is difficulty locating the nerve, try locating the tensor fascia lata and sartorius muscles. The LFCN lies between them in this intermuscular hypoechoic space.[2]
- Trace the course by scanning proximally and distally to confirm its appropriate anatomical course extending to the lateral thigh.
- Follow the nerve proximally to find a suitable inject site at the most proximal location possible.
- Advance the needle medially to to laterally, in-plane.
- Hydro-dissect between the fascia lata and fascia iliaca with 5% dextrose to better visualise the nerve.
- Advance the needle targeting the nerve in-plane or out-of-plane depending on its position relative to the ASIS.
Transverse ultrasound image of the LFCN lying within the intermuscular space between the tensor fasciae latae muscle and the sartorius.
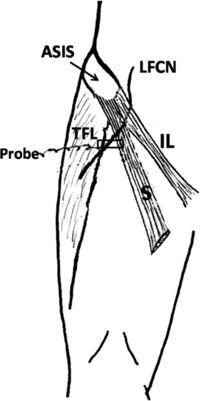
LFCN: lateral femoral cutaneous nerve; TFL: tensor fasciae latae muscle; S: Sartorius; R: rectus femoris.[2]Transverse ultrasound image shows the nerve passing under the inguinal ligament.
ASIS: anterior superior iliac spine; LFCN: lateral femoral cutaneous nerve; IL: inguinal ligament.[2]Transverse ultrasound image shows the nerve passing through the inguinal ligament.
ASIS: anterior superior iliac spine; LFCN: lateral femoral cutaneous nerve; IL: inguinal ligament.[2]
Fluoroscopy Guided
Fluoroscopy is only rarely done for several reasons. Ultrasound is superior for visualising anatomical variations, and the ASIS is generally palpable. In patients where the ASIS is not palpable, fluoroscopy may be considered.
Landmark Guided
The traditional technique is a fanned-out injection through the fascia lata along the inguinal ligament without eliciting paraesthesia. The fascia iliaca block is elegant in its solution to addressing the anatomical variability of the LFCN. The landmark guidance has several disadvantages to ultrasound guided injection. Failure rates have been reported up to 60%, and slow onset can occur. There have been reports of inadvertent blockage of all three of the obturator, femoral, and LFC nerves. There is also the risk for needle trauma to the LFCN.[1]
- Identify 2-3cm inferior to and 2-3cm medial to the ASIS.
- Inject local anaesthetic under the skin making a wheal.
- Insert a short bevel 22-gauge 4cm needle perpendicularly.
- Advance until a "pop" occurs. This signifies passage through the fascia lata.
- Aspirate confirming no blood.
- Inject 2/3 of the injectate.
- Withdraw slightly above the fascia lata.
- Inject the last 1/3 of the injectate in a fan medially and laterally.
Examine for evidence of femoral and obturator nerve blockage prior to release.
Complications
Bleeding, infection, injury to surrounding structures including vessels and nerves (femoral and obturator), inadvertent 3-in-1 block (LFCN, femoral, obturator), failure to relieve pain.[1]
Aftercare
Weight loss if of vital importance if it is a relevant causative factor. Also avoid tight clothing. If the patient is pregnant then symptoms usually resolve after delivery of the fetus.
Videos
See Also
External Links
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Trescot, Andrea. Peripheral nerve entrapments : clinical diagnosis and management. Switzerland: Springer, 2016.
- ↑ 2.0 2.1 2.2 2.3 2.4 Zhu et al.. Ultrasound of the lateral femoral cutaneous nerve in asymptomatic adults. BMC musculoskeletal disorders 2012. 13:227. PMID: 23171132. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,
![Transverse ultrasound image of the LFCN lying within the intermuscular space between the tensor fasciae latae muscle and the sartorius. LFCN: lateral femoral cutaneous nerve; TFL: tensor fasciae latae muscle; S: Sartorius; R: rectus femoris.[2]](/w/img_auth.php/thumb/e/e8/LFCN_ultrasound.jpg/266px-LFCN_ultrasound.jpg)
![Transverse ultrasound image shows the nerve passing under the inguinal ligament. ASIS: anterior superior iliac spine; LFCN: lateral femoral cutaneous nerve; IL: inguinal ligament.[2]](/w/img_auth.php/thumb/2/20/LFCN_ultrasound2.jpg/264px-LFCN_ultrasound2.jpg)
![Transverse ultrasound image shows the nerve passing through the inguinal ligament. ASIS: anterior superior iliac spine; LFCN: lateral femoral cutaneous nerve; IL: inguinal ligament.[2]](/w/img_auth.php/thumb/4/46/LFCN_ultrasound3.jpg/281px-LFCN_ultrasound3.jpg)


