Low Back Pain Definitions
The definition of low back pain should not be ignored, and a topographical description is preferred. Starting with the wrong topographical area can lead to the wrong diagnosis. A topographical definition makes no assumption as to cause of the pain, only its location.
The importance of having clear definition has been demonstrated in a 1989 study. They found the interobserver reliability of defining a patients pain pattern as being in the "back" to be very poor (Kappa 0.16). Defining the pain pattern as "buttock pain" had moderate agreement (Kappa 0.44); foot pain, leg pain, and thigh pain all had good agreement (Kappa 0.73, Kappa 0.96, and Kappa 0.78 respectively)[1]
It is important to get the patient to show you exactly where they feel the pain rather than simply take what they say for granted. Anecdotally, there are a wide array of terms that are used by patients to describe what taxonomically is lumbar spine pain. For example I have commonly heard patients call the lumbar spinal area the hip. I'm not sure if this is a New Zealand specific language pattern.
Low Back Pain
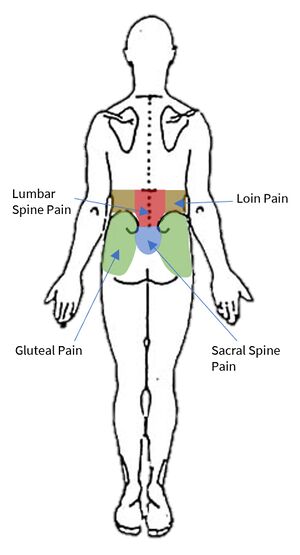
The IASP taxonomy does not recognise the term "back pain," rather it categorises it into lumbar spinal pain and sacral spinal pain. There is also an overlapping definition called lumbosacral pain. These three categories constitute the colloquial term "low back pain." Another overlapping definition is thoraco-lumbar pain, but this is not low back pain. The IASP taxonomy are periodically updated, so to get the latest definition go to IASP and in part I (topics and codes) click on "spinal pain, section1: spinal and radicular pain syndromes." The definitions here are up to date as of August 2021.[2]
Lumbar Spinal pain
"Pain perceived as arising from anywhere within a region bounded superiorly by an imaginary transverse line through the tip of the last thoracic spinous process, inferiorly by an imaginary transverse line through the tip of the first sacral spinous process, and laterally by vertical lines tangential to the lateral borders of the lumbar erectores spinae...If required, lumbar spinal pain can be divided into upper lumbar spinal pain and lower lumbar spinal pain by subdividing the above region into equal halves by an imaginary transverse line."
Sacral Spinal Pain
"Pain perceived as arising from anywhere within a region bounded superiorly by an imaginary transverse line through the tip of the first sacral spinous process, inferiorly by an imaginary transverse line through the posterior sacrococcygeal joints, and laterally by imaginary lines passing through the posterior superior and posterior inferior iliac spines."
Lumbosacral Pain:
"Pain perceived as arising from a region encompassing or centred over the lower third of the lumbar region as described above and the upper third of the sacral region as described above."
Not Low Back Pain
Pain in regions adjacent to the above topographical areas are not low back pain. There are a variety of other taxonomical definitions to describe pain in other areas.
Gluteal Pain:
"Referred pain over the lower limb girdle posteriorly may be described as gluteal pain. For this purpose the gluteal region may be defined as a sector central on the greater trochanter and spanning from the posterior inferior iliac spine to the anterior superior iliac spine. "
This is very commonly mistaken for back pain. Local causes of gluteal pain should be considered first before lumbar referred conditions.
Posterior Hip Pain
"Referred pain immediately below [the gluteal pain region[ posteriorly should be qualified as posterior hip pain"
Anterior Hip Pain
"Pain immediately below [the gluteal pain region anteriorly[ should be qualified as anterior hip pain."
Groin Pain
"Pain focused over the inguinal ligament may be qualified as groin pain."
Loin Pain:
"Pain located over the posterior region of the trunk but lateral to the erectores spinae is best described as loin pain to distinguish it from lumbar spinal pain."
The identification of loin pain is important because it is more likely to be due to a visceral disorder, for example it could lead to missing a diagnosis of pyelonephritis or renal colic.
Thoracic Spinal Pain:
"Pain perceived as arising from anywhere within the region bounded superiorly by an imaginary transverse line through the tip of first thoracic spinous process, inferiorly by an imaginary transverse line through the tip of the last thoracic spinous process, and laterally by vertical lines tangential to the most lateral margins of the erectores spinae muscles. "
Posterior Chest Wall Pain:
"Pain located over the posterior chest wall but lateral to the above region [for thoracic spinal pain] is best described as posterior chest wall pain to distinguish it from thoracic spinal pain. If required, thoracic spinal pain can be further qualified by dividing the above region into thirds from the top down, to establish regions of upper thoracic, mid thoracic, and lower thoracic spinal pain"
Thoraco-Lumbar Pain:
"Pain perceived as arising from a region encompassing or centred over the lower quarter of the thoracic region as described above and the upper third of the lumbar region as described above."
Sciatica:
"This term is an anachronism and should be abandoned. It stems from an era when the mechanisms of referred pain and radicular pain were poorly understood. It was used to describe pain that appeared to travel along the course of the sciatic nerve. The unfortunate legacy of this term is that it has been applied erroneously to any or all pain of spinal origin perceived in the lower limb. Furthermore, because nerve root compression has been believed to be the cause of sciatica, many forms of referred pain in the lower limb have been erroneously ascribed to this cause. Clinical experiments have shown that the only type of pain that is evoked by stimulating nerve roots is radicular pain as described above (Norlen 1944; Smyth and Wright 1959; McCulloch and Waddell 1980). Consequently, at the most, sciatica and radicular pain can be considered as synonymous. However, there is no justification on physiological grounds for equating sciatica and referred pain. The two are distinct in mechanism and quality. Pain in the lower limb should be described specifically as either referred pain or radicular pain. In cases of doubt no implication should be made and the pain should be described as pain in the lower limb."
Other Lower Limb:
"Referred pain in the lower limb may be qualified using standard anatomical terms that describe its topographic location, viz., thigh, leg, foot, digits I-V, anterior, posterior, medial, lateral, dorsal, plantar. Descriptors based on the course or distribution of nerves, such as “sciatica” and “anterior sciatica” should not be used because they convey an unjustified implication of the involvement of the said nerve. The term “calf’ can substitute for “posterior leg.”
Acute, Subacute, and Chronic
The pathophysiology, natural history, and treatment response are different for each category. Certain investigations may only be appropriate for different time periods. The temporal pattern is part of the problem representation.
The standard temporal definitions are as follows:
Acute low back pain: Low back pain that has been present for less than 3 months
Subacute low back pain: Low back pain that has been present for longer than 5 to 7 weeks but not longer than 12 weeks.
Chronic low back pain: Low back pain that has been present for at least 3 months.
More difficult to define are those with "recurrent" low back pain, or "acute on chronic" low back pain. For recurrent low back pain, if there is a pain-free period of at least 3 months, then each episode is termed acute low back pain. If the patient has continuous low level back pain with episodes of exacerbations, this is termed chronic low bakc pain.
Referred Pain
- Main article: Referred Pain
Referred pain is best described in neurological terms as "pain perceived as arising or occurring in a region of the body innervated by nerves or branches of nerves other than those that innervate the actual source of pain". In topographical terms it is perceived in a region that is topographically distinct from the actual source of the pain. The topographical definition becomes ambiguous in cases where it is unclear where one region of the body ends and an adjacent region begins.
The IASP continues: "Referred pain may thus occur in a region that is either remote from or directly contiguous with the source of pain, but the two locations are distinguishable on the basis of their different nerve supply. In the context of spinal pain, referred pain may occur in the head, the upper limb girdle and upper limb, the posterior or anterior chest wall, the abdominal wall, the lower limb girdle and the lower limb. The distribution of referred pain in the head can be described in terms of the region encompassed based on the underlying bones of the skull or regions of the skull, viz., occipital, parietal, frontal, temporal, orbital, auricular, maxillary, and mandibular. Referred pain to the upper limb girdle may encompass all or only part of the girdle."
The descriptors in the above section may be used for the referred pain regions. If a patient has both spinal pain and referred pain, then both pains should be explicitly stated e.g. "lower cervical spinal pain and referred pain to the shoulder," or "lumbosacral pain with referred pain to the gluteal region and posterior thigh"
There are two mechanisms for referred pain: one arising from convergence (visceral and somatic referred pain), and one from stimulation of a nerve (neuropathic pain). In both somatic and visceral referred pain, the physiological mechanism is that of convergence of afferent pathways into the central nervous system.
Visceral Referred Pain
Visceral referred pain is referred pain where the source lies in an organ or blood vessel of the body. With low back pain, the uterus and abdominal aorta are important considerations. Other viscera with higher segmental supply may cause back pain such as pancreatitis, but this may be due to irritation of the posterior abdominal wall, in which case the pain is not truly referred in nature.[3]
Somatic Referred Pain
- See also: Lumbar Pain Maps, Sacroiliac Pain Maps
Somatic referred pain is referred pain where the source originates in a tissue or structure of the body wall or limbs. A number of structures in the lumbar spine and sacrum have been shown to capable of producing somatic referred pain in experiments of asymptomatic individuals with injection of noxious substances.
With noxious stimulation of the lower lumbar zygapophyseal joints, pain can be referred to the gluteal region, thigh, and even the leg and foot. The intervertebral discs can refer pain to the gluteal region, thigh, and leg; even the thigh and leg without the buttock. Previously it was not known whether the sacroiliac joint can refer pain past the gluteal region[3], but there is now evidence showing that it can.[4][5][6] (see Lumbar Pain Maps and Sacroiliac Pain Maps).
Each of these examples is caused by stimulation of nerve endings in a lumbar or sacral structure, and so each is an example of somatic referred pain. Each also on the surface resembles "sciatica" in terms of the pain extending into the lower limb. Incorrectly distinguishing radicular pain from somatic referred pain is a common pitfall in diagnosis and with incorrect diagnosis this frequently leads to incorrect treatment. Somatic referred pain is in fact more common than radicular pain.
It is uncommon for somatic referred pain to occur without any back pain. If there is somatic type pain in the lower limb, then local causes should be assessed for. This includes gluteal pain in the absence of low back pain.
Radicular Pain
Neuropathic pain sits in contrast to visceral and somatic referred pain. Radicular pain is a subset of neuropathic pain, and refers to pain that is evoked with stimulation of the nerve roots or dorsal root ganglion of a spinal nerve - i.e. the peripheral axons or cell bodies rather than the peripheral nerve endings. In radicular pain, the pain is felt in the peripheral innervation of the affected nerve. Therefore it is a form of referred pain, but doesn't involve the convergence mechanism. The pain is felt in the periphery because of stimulation to the nerve proximal to the peripheral distribution. The older now obsolete term for neuropathic pain was "neurogenic pain."
Radicular pain is commonly confused with radiculopathy. Radiculopathy is distinct, it is not defined by pain, but rather refers to conduction block along a spinal nerve or its roots with some combination of weakness, numbness, and hyporeflexia. With sensory fibre block numbness develops in a dermatomal distribution. With motor fibre block weakness develops in a myotomal distribution. Reduced reflexes can occur through either sensory or motor blockade.
Distinguishing Somatic Referred From Radicular Pain
The following table can serve as a guide. It is important to note that patients may have a combined state, experiencing both somatic referred and radicular pain. For example a prolapsed disc may irritate the dura of the nerve root (somatic) as well as the nerve root itself (radicular).
| Somatic Referred | Radicular | |
|---|---|---|
| Pain quality | Dull, deep ache, or pressure-like, perhaps like an expanding pressure | Shooting, lancinating, or electric-shocks |
| Relation to back pain | Referred pain is always concurrent with back pain. If the back pain ceases then so does the referred pain. If the back pain flares then so does the leg pain intensity and spatial spread. | Not always concurrent with back pain. |
| Distribution | Anywhere in the lower limb, fixed in location, commonly in the buttock or proximal thigh. Spread of pain distal to the knee can occur when severe even to the foot, and it can skip regions such as the thigh. It can feel like an expanding pressure into the lower limb, but remains in location once established without traveling. It can wax and wane, but does so in the same location. | Entire length of lower limb, but below knee > above knee. In mild cases the pain may be restricted proximally. |
| Pattern | Felt in a wide area, with difficult to perceive boundaries, often demonstrated with an open hand rather than pointing finger. The centres in contrast can be confidently indicated. | Travels along a narrow band no more than 5-8 cm wide in a quasi-segmental fashion but not related to dermatomes (dynatomal). |
| Depth | Deep only, lacks any cutaneous quality | Deep as well as superficial |
| Neurological signs | Not characteristic | Favours radicular pain, but not required. |
| Neuroanatomical basis | Discharge of the peripheral nerve endings of Aδ and C fibres from the lower back converge onto second order neurons in the dorsal horn that also receive input from from the lower limb, and so the frontal lobe has no way of knowing where the pain came from. | Heterotopic discharge of Aδ, Aβ, and C fibres through stimulation of a dorsal root or dorsal root ganglion of a spinal nerve, typically in the presence of inflammation, with pain being felt in the peripheral innervation of the affected nerve |
See Also
References
- ↑ McCombe PF, Fairbank JC, Cockersole BC, Pynsent PB. 1989 Volvo Award in clinical sciences. Reproducibility of physical signs in low-back pain. Spine (Phila Pa 1976). 1989 Sep;14(9):908-18. doi: 10.1097/00007632-198909000-00002. PMID: 2528822.
- ↑ Classification of Chronic Pain, Second Edition (Revised) | International Association for the Study of Pain (IASP) (iasp-pain.org)
- ↑ 3.0 3.1 Bogduk et al. Medical Management of Acute and Chronic Low Back Pain: An Evidence Based Approach. Chapter 2. Elsevier Science. 2002
- ↑ van der Wurff P, Buijs EJ, Groen GJ. Intensity mapping of pain referral areas in sacroiliac joint pain patients. J Manipulative Physiol Ther. 2006 Mar-Apr;29(3):190-5. doi: 10.1016/j.jmpt.2006.01.007. PMID: 16584942.
- ↑ Murakami E, Tanaka Y, Aizawa T, Ishizuka M, Kokubun S. Effect of periarticular and intraarticular lidocaine injections for sacroiliac joint pain: prospective comparative study. J Orthop Sci. 2007 May;12(3):274-80. doi: 10.1007/s00776-007-1126-1. Epub 2007 May 31. PMID: 17530380.
- ↑ Kurosawa D, Murakami E, Aizawa T. Referred pain location depends on the affected section of the sacroiliac joint. Eur Spine J. 2015 Mar;24(3):521-7. doi: 10.1007/s00586-014-3604-4. Epub 2014 Oct 5. PMID: 25283251.
- ↑ Bogduk et al. Medical Management of Acute and Chronic Low Back Pain: An Evidence Based Approach. Elsevier Science. 2002