Low Back Pain Treatment Strategies
The appropriate management of chronic low back pain is a political minefield. King and Bogduk write that the treatment literature on chronic low back pain is mired in ideology and vested interests.[1] There are "camps" or "craft groups" with different ideologies, and this biases their approach.
Historical Context
Pre 1980s
- Empirical conservative treatment (drugs, traction, ultrasound, exercises, physical therapy)
- Try monotherapies one after the other, hoping next one will work
- If no improvement, referred for surgery (empirical surgery)
Post 1980s
- Around 1980s standard approach challenged
- Behavioural approach emerged: treatments weren’t working because of unaddressed psychological/behavioural issues
- High-tech treatments (spinal cord stimulation, intraspinal drug delivery) emerged when behavioural approach also found to not work
- Reductionism: precision diagnosis needed; pin-point the lesion
- Tensions between approaches; each thinks other doesn’t work. Evidence based medicine is introduced.
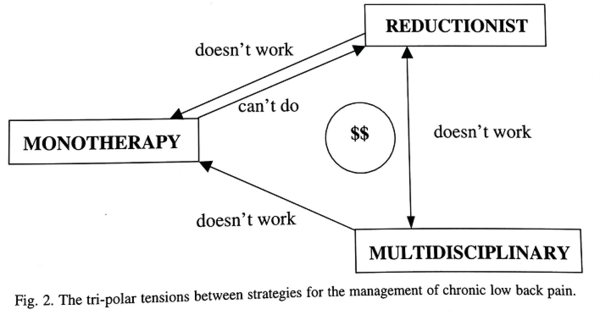
Three Poles
MDT pole. They generally make non-specific diagnoses and provide multiple non-specific treatments in a team. For example they may diagnose non-specific chronic low back pain with central sensitisation and provide psychological and behavioural therapy with the aim of enabling better coping skills, reduced fear-avoidance behaviour, reduced catastrophising, and improved psychological distress. They prioritise improving function over improving pain. They may view pain as something that must be accepted to be able to get on with life. The approach may be slightly skewed towards paternalism without aiming for patient defined outcomes such as complete relief of pain. There are rare MDT groups that also incorporate the full suite of biomedical options.
Reductionist pole. They generally make specific diagnoses and provide specific treatments, i.e. they try to pinpoint the source of the pain and stop it peripherally. For example they may diagnose right L4/5 facet joint pain based on controlled medial branch blocks and provide medial branch radiofrequency neurotomy. They prioritise improving pain and view disability and psychosocial distress as something that improves if the pain is fixed. Reductionism requires specialised skills and facilities that may not be available in all centres.
Monotherapy pole. They generally make non-specific diagnoses and provide single specific treatments (although sometimes non-specific) by a single individual. For example they may diagnose mechanical low back pain and provide lumbar fusion. The monotherapies recommended often get recommended in sequential order, i.e. they try one therapy and then move on to the next if it didn't work. If conservative management didn't work then they move on to surgery.
I propose a fourth category: nihilism. This sits outside the three poles, and views low back pain as an insoluble problem with no good treatment strategies for most affected individuals.
Tripolar Tension in the NZ Context
Each group may state that the treatments of the other groups don't work, and each have their own literature which may ignore the literature of the other groups. None of the groups deny the importance of the biopsychosocial model, however the MDT group may call it the sociopsychobiomedical model due to the different views regarding the relevant importance of each domain. The usual limitations of evidence based medicine apply[2], but it the best tool we have.
There is also a lot of overlap for individual doctors and for individual specialties. Individual specialties tend to have a "culture".
- Musculoskeletal medicine tends to have a bias towards reductionism (e.g. radiofrequency neurotomy following positive blocks) and monotherapies (e.g. corticosteroid injections, manual therapy, exercise prescriptions), but may also work in MDT.
- Pain medicine have a bias towards MDT and monotherapies, and less commonly engage in reductionism. This is the newest specialty in New Zealand.
- Orthopaedic surgeons engage in both monotherapy (e.g. fusion for sagittal imbalance) and reductionism (e.g. L4/5 microdiscectomy for L5 radicular pain, or sacroiliac joint fusion following positive blocks), however generally not MDT.
- Allied health providers generally do monotherapies with some also being involved in MDT.
The patient's General Practitioner is the most important of all specialists as they can view the biases non-objectively from the outside without vested interests and tend to know the patient the best.
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,