Lumbar Fat Herniation
| |
| Lumbar Fat Herniation | |
|---|---|
| Synonym | Episacral lipoma, sacroiliac lipoma, back mouse, fibro-fatty nodule, fibrositis, subfascial fat herniation |
| Epidemiology | present in 10–58% |
| Pathophysiology | tear in lumbosacral fascia with herniation, or discrete nodule. |
| History | Chronic low back pain |
| Examination | Focal tenderness |
| Diagnosis | Subcutaneous iliac crest nodule plus abolition of pain with local anaesthetic injection. |
| Tests | Local anaesethetic injection |
| Treatment | Local anaesthetic injections, steroid injections, excision. |
Episacral lipomata, also known as back mice, and subfascial fat herniation among other terms, are an uncommon cause of chronic low back pain with only infrequent mention in the literature. They occur over the posterior iliac crest as an ovoid, mobile, and subcutaneous small mass.[1]
Pathophysiology
There are two hypotheses regarding the pathophysiology. Some authors state that the condition is where deep fat herniates through the thoracolumbar fascia in a more superficial extramuscular, subcutaneous location. Other authors report that they are discrete lipomata or fibro-fatty nodules. It may be that these are two separate conditions with similar clinical presentations.[1]
The thoracolumbar fascia has fenestrations where cutaneous branches of the dorsal rami pass through, but it isn't clear how fat herniation can actually cause pain however.[2] The hypermobility of the mass may be a factor in the pain.[1]
They are a discrete entity from inferior lumbar hernias. Lumbar hernias are where there is herniation of intra- or retro-peritoneal structures through the inferior lumbar triangle into the soft tissues of the low back.[1]
Epidemiology
There is a wide range of reported prevalence from 10–58%, and may be bilateral. They are usually asymptomatic. They have a predilection for females.[1]
Clinical Features
The patient may report a painful subcutaneous mass in about the posterior superior iliac spine. The pain may radiate to to the buttock or thigh. Pain may radiate to the buttock or thigh. Pressure over the mass may reproduce the patients pain.
Imaging
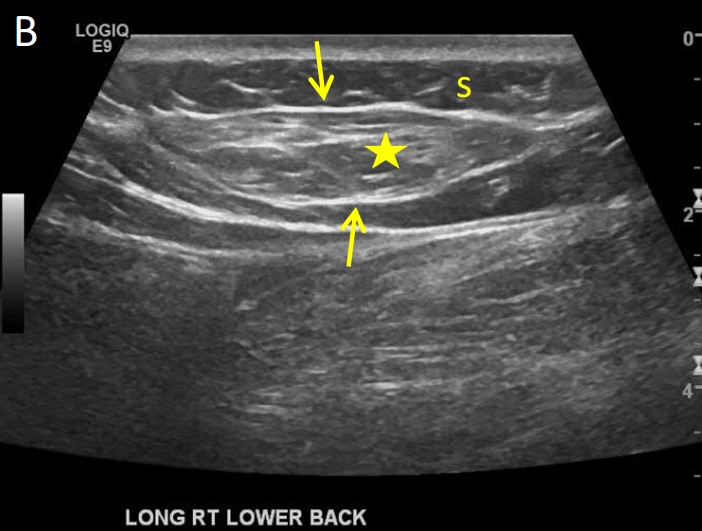
Ultrasonography may demonstrate hypermobile deep fat between the superficial and deep fascial layers in the low back near the PSIS. There may or may not be a capsule. Where there is a lack of a capsule, it is not a true lipoma, and the correct term should be subfascial herniation. There may be a lack of a distinct lateral margin.[1]
Diagnosis
The diagnosis is supported by abolition of pain with infiltration of local anaesthetic.[2]
Mechanical Low Back Pain (97%)
- Internal disc disruption
- Facet joint pain
- Sacroiliac joint pain
- Sacroiliac ligament pain
- Torsion injuries
- Vertebral or sacral insufficiency fractures
- Interspinous tissue injury
- Lamina impaction
- Scoliosis
- Spondylolysis in a sportsperson, but not the general population
- The following are disputed causes of low back pain: degenerative changes, low grade disc infection, non-specific chronic low back pain, transitional vertebrae, congenital fusion, spina bifida occulta, spondylolisthesis, instability, failed back surgery syndrome, back mice, cluneal nerve entrapment, spinal stenosis, myofascial syndrome
Nonmechanical Spine Conditions (1%)
- Neoplasia (Multiple myeloma, metastatic carcinoma, lymphoma, leukaemia, spinal cord tumours, retroperitoneal tumours, primary vertebral tumours)
- Infection (Osteomyelitis, discitis, paraspinous abscess, epidural abscess, shingles)
- Spondyloarthritis
- Scheuermann disease, especially type II
- Diffuse idiopathic skeletal hyperostosis
- Osteitis Condensans Ilii
- Paget disease
Visceral Disease (2%)
- Pelvic organ involvement (Prostatitis, endometriosis, chronic pelvic inflammatory disease)
- Renal involvement (Nephrolithiasis, pyelonephritis, perinephric abscess)
- Aortic aneurysm
- Gastrointestinal involvement (Pancreatitis, cholecystitis, ulcer)
Treatment
The prognosis is unknown, but symptoms may resolve on its own. Treatment options include local anaesthetic and/or steroid injections, and excision.[1]
External Resources
- Open access review by Bicket et al.[3]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Tiegs-Heiden et al.. Subfascial fat herniation: sonographic features of back mice. Skeletal radiology 2018. 47:137-140. PMID: 28914351. DOI.
- ↑ 2.0 2.1 Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Chapter 15. Edinburgh: Elsevier/Churchill Livingstone, 2012.
- ↑ Bicket et al.. The Best-Laid Plans of "Back Mice" and Men: A Case Report and Literature Review of Episacroiliac Lipoma. Pain physician 2016. 19:181-8. PMID: 27008292.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


