Lumbar Pseudoarthrosis
| |
| Lumbar Pseudoarthrosis |
|---|
Lumbar pseudoarthrosis (also known as lumbar pseudarthrosis) represents a potential complication of lumbar spinal fusion surgery and can have a significant impact on patient outcomes. Pseudoarthrosis, derived from the Greek words "pseudo" meaning false and "arthrosis" meaning joint, is a term used to describe the failure of a spinal fusion surgery to achieve successful bony union. In the context of the lumbar spine, pseudoarthrosis occurs when the intended fusion of vertebral segments fails to create a solid, continuous bridge of bone that effectively stabilises the spine by 1 year after surgery. This can (but not always) lead to persistent pain, loss of function, and the potential for additional surgical intervention.
Epidemiology and Risk Factors
The incidence of lumbar pseudoarthrosis varies widely, with reported rates ranging from 5% to 35%[1] depending on the specific population, surgical technique, and method of evaluation.
Several risk factors have been identified, including patient-related factors (e.g., age, smoking status, obesity), surgical factors (e.g., instrumentation type, surgical approach, number of levels fused), and biomechanical factors (e.g., spinal alignment, instability).
Pathophysiology
Lumbar pseudoarthrosis results from the disruption of the normal bone healing process, with numerous factors potentially contributing to the failure of spinal fusion.[2]
Bone Healing Process
Spinal fusion involves the placement of bone graft material between adjacent vertebral bodies, creating an environment that promotes osteogenesis, osteoinduction, and osteoconduction. Osteogenesis refers to the formation of new bone by osteoblasts, while osteoinduction involves the stimulation of osteoprogenitor cells to differentiate into osteoblasts. Osteoconduction is the process by which bone graft material provides a scaffold for new bone formation.
Lumbar pseudoarthrosis results from the disruption of the normal bone healing process, with numerous factors potentially contributing to the failure of spinal fusion. Bone healing following spinal fusion surgery typically occurs through a three-phase process: inflammatory, repair, and remodeling.
In the inflammatory phase, a haematoma forms around the fusion bed, with the infiltration of macrophages, polymorphonuclear cells, and fibroblasts. These cells release metabolic factors promoting granulation tissue formation, mesenchymal cell migration, and factors necessary for vascular proliferation, such as vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and epidermal growth factor (EGF). The repair phase involves repopulation of progenitor cells at the host–graft interface, with subsequent chondrogenic and osteogenic development, maturation of a collagen matrix, and ossification to form woven bone. Finally, the remodeling phase involves the interplay between osteoblasts and osteoclasts, yielding the final mature fusion.
The timeframe for successful bony fusion following spinal surgery can vary depending on several factors, including the patient's age, overall health, bone quality, and the specific surgical technique used. The early fusion stage is within the first few months where the bone graft material begins to integrate with the surrounding vertebral bone, and early trabecular bridging can be observed. Full bony fusion with a stable spinal construct can take 3 to 6 months and in some cases up to a year. Pseudoarthrosis is diagnosed when bony fusion hasn't occurred by one year post surgery.
Factors Affecting Bone Formation and Remodeling
The failure of spinal fusion and development of lumbar pseudoarthrosis can result from a variety of factors that interfere with bone healing and remodeling. Some key factors include:
Systemic Factors:
- Medical comorbidities such as rheumatoid arthritis and osteoporosis may negatively affect fusion rates. Smoking, advanced age, diabetes, and certain medications (e.g., corticosteroids, nonsteroidal anti-inflammatory drugs) may also negatively impact bone healing. Nutritional status and medications can influence fusion rates.
- Smoking is a major controllable risk factor for pseudoarthrosis after spinal fusion. Nicotine negatively affects bone healing, gene expression, and vascular networks, ultimately decreasing bone mineral density and formation.
- Medication: NSAIDs may inhibit spinal fusion due to their effect on prostaglandin E2, an important factor in bone healing. Ketorolac use after spine surgery has been associated with pseudoarthrosis in a dose-dependent manner. Systemic steroids inhibit the inflammatory phase of bone healing and the differentiation of progenitor cells, and decrease the synthesis of the extracellular matrix.
Surgical Factors:
Factors controllable by the surgeon include bone graft choice, fusion site, graft site preparation, fusion levels, construct design, and biological modifiers. These factors should be considered to optimize patient outcomes.
- Bone Graft and Graft Selection: Bone graft properties such as osteoconductivity, osteoinductivity, osteogenicity, mechanical strength, and vascularity influence fusion rate. Autologous bone grafts are considered the gold standard, but other options like allografts and synthetic grafts are available but may have variable osteogenic, osteoinductive, and osteoconductive properties.
- Bone Morphogenetic Protein (BMP): BMP-2 is a synthetic protein with osteoinductive properties used as an alternative to autologous bone graft. It has shown efficacy in lumbar spinal fusion, but its safety profile has come under scrutiny.
- Graft Location: The fusion surface location greatly influences the success of arthrodesis. Interbody fusion in the anterior column provides a favorable environment, while posterior fusion is more familiar but less load-sharing.
- Surgical Site Preparation: Proper fusion bed preparation is crucial, involving soft tissue removal, hemostasis, decortication, and graft placement. Decortication stimulates local marrow, but excessive technique may cause thermal necrosis.
- Fusion Construct: Spinal fusion with instrumentation creates a rigid construct, increasing fusion rate. Techniques include posterior pedicle screw fixation and anterior or lateral fixation. Proper global and regional spinal alignment can also impact fusion rates.
Investigations
Various imaging modalities can provide valuable information about the spinal fusion site, bony structure, surrounding soft tissues, and the overall alignment of the spine. The following imaging techniques are commonly used in the assessment of lumbar pseudoarthrosis:
Plain Radiographs
Plain radiographs are often the initial imaging modality used to evaluate the lumbar spine, providing information about spinal alignment, vertebral body height, and the position of any hardware or instrumentation. Arthrodesis is confirmed by visualising solid bone bridging across the fusion site. For posterolateral fusion look for solid bridging of the transverse processes in AP view. For interbody fusion assess for bridging across the disc space. Pseudoarthrosis is suggested by the absence of bridging ossification or a radiolucent line across the fusion mass. In the presence of instrumentation, hardware fracture may indicate failure of fusion.
However, plain radiographs have limited sensitivity and specificity in detecting early pseudoarthrosis, and it can be challenging to visualize the fusion site in detail. Flexion and extension views can be used in identifying spinal instability (in the absence of instrumentation), which may be suggestive of pseudoarthrosis and this can increase sensitivity but not specificity.[2]
CT
Computed tomography (CT) is a more sensitive and specific imaging modality for evaluating the bony structure and fusion site compared to plain radiographs. Multiplanar reconstructions and high-resolution images can provide detailed information about the bone graft, trabecular bridging, and any potential areas of nonunion. In addition, CT scans can help identify hardware complications, such as screw loosening or breakage, which may be contributing to pseudoarthrosis.
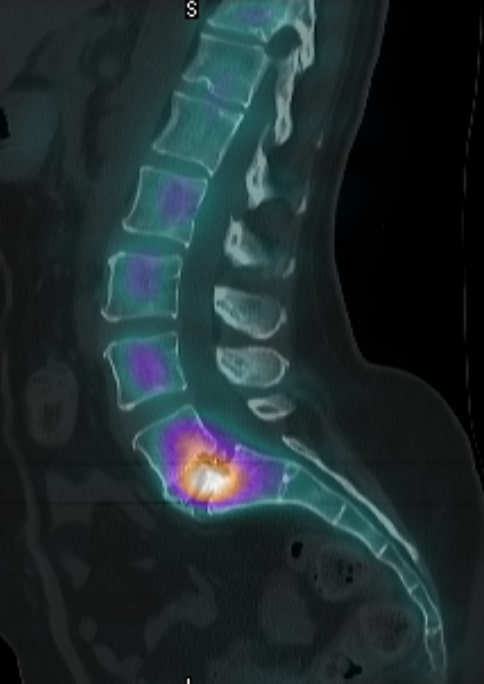
CT-SPECT
Computed Tomography with Single-Photon Emission Computed Tomography (CT-SPECT) is a hybrid imaging modality that combines the detailed anatomical information provided by CT with the functional imaging capabilities of SPECT. This combination allows for improved assessment of bone metabolism and fusion status at the surgical site.
In the context of lumbar pseudoarthrosis, CT-SPECT can be particularly valuable for identifying areas of increased bone turnover or metabolic activity, which may be suggestive of a nonunion or incomplete fusion. Increased radiotracer uptake in the fusion site can indicate the presence of pseudoarthrosis, as it represents increased bone remodeling and metabolic activity in response to mechanical stress or instability. Conversely, a lack of tracer uptake may indicate a solid fusion with no ongoing bone remodeling.
MRI
While MRI is not as sensitive as CT for evaluating the bony fusion site, it can be valuable for assessing adjacent levels or identifying potential causes of persistent pain or neurological symptoms, such as nerve root compression, disc herniation, or scar tissue formation. In certain cases, a contrast-enhanced MRI may be useful for detecting inflammation or infection at the fusion site, which could be contributing to pseudoarthrosis.
Clinical Features
There are no known characteristic or pathognomonic clinical features to indicate a symptomatic pseudoarthrosis. Axial and/or radicular pain can be present, but the condition is often asymptomatic.
Diagnosis
It is not clear why some cases of pseudoarthrosis are asymptomatic and others are symptomatic. In the short term there is no difference in return to activity, symptom relief, and surgical satisfaction between those with pseudoarthrosis and successful fusion. However successful fusion can improve longer term outcomes and decrease repeat operations.
Diagnosing lumbar pseudoarthrosis can be challenging, as it may not always be symptomatic or cause functional impairments. Heggeness and Esses described four unique morphological categories to help classify posterolateral lumbar pseudarthroses: atrophic, transverse, shingle, and complex.[3] Despite this classification, it is often difficult to predict when or if a pseudarthrosis will become symptomatic.
A very old study compared outcomes in patients with radiographic evidence of lumbar pseudarthrosis to a matched cohort with successful lumbar fusion, finding no significant difference between the two groups with regard to return to activity, symptom relief, and subjective satisfaction with the surgery.[4]
However, more recent studies suggest that successful lumbar fusion correlates with long-term improved functional outcomes and decreased symptom severity. One study reported that among their patients with symptomatic spinal stenosis and spondylolisthesis treated with bilateral posterolateral arthrodesis, 86% of the patients with solid arthrodesis had “excellent” or “good” long-term clinical outcome compared with 56% of patients with a pseudarthrosis.[5] In clinical situations that require revision spinal fusion for pseudarthrosis, another study reported that only 26% of patients had excellent or good operative outcomes, despite the fact that solid fusion was achieved in 94% of the total cohort.[6]
It remains unclear why some cases of pseudarthrosis remain asymptomatic with excellent long-term clinical outcomes, while others require significant management and treatment. Bony nonunion can be asymptomatic on short-term follow-up, but this condition can lead to reoperations up to 10 years after the index procedure.
Management
In cases where conservative management fails to alleviate symptoms or when pseudoarthrosis is associated with significant pain, neurological deficits, or spinal instability, surgical intervention may be offered. It is important to note that while revision surgery for lumbar pseudoarthrosis may result in solid fusion, the clinical outcomes can be variable, and not all patients experience significant improvements in pain or function. Revision procedures have historically had high rates of clinical failure (40-70%) and recurrent pseudoarthrosis (30-50%).[7]
The choice of surgical technique depends on various factors, including the patient's overall health, the location and extent of the pseudoarthrosis, and any underlying spinal pathology.
Revision Spinal Fusion
Revision spinal fusion is the most common surgical approach for treating lumbar pseudoarthrosis. The procedure involves the removal of any scar tissue, fibrous tissue, or hardware that may be impeding bone healing, followed by the placement of new bone graft material and stabilization with instrumentation. Autograft, allograft, or synthetic bone graft substitutes can be used to promote bone healing and fusion. In some cases, the use of additional bone morphogenetic proteins (BMPs) or other osteoinductive agents may be considered to enhance the fusion process.
Pedicle Screw Fixation
Instrumentation, such as pedicle screw fixation, is often employed to provide immediate spinal stability and to maintain proper alignment during the bone healing process. The screws are inserted into the pedicles of the affected vertebrae and connected with rods, providing a rigid construct that limits motion at the fusion site. This added stability can facilitate bone healing and reduce the risk of recurrent pseudoarthrosis.
ALIF or TLIF
In select cases, an interbody fusion technique, such as anterior lumbar interbody fusion (ALIF) or transforaminal lumbar interbody fusion (TLIF), may be performed to address lumbar pseudoarthrosis. These procedures involve the removal of the intervertebral disc and placement of an interbody cage filled with bone graft material between the adjacent vertebral bodies. This approach can provide additional spinal stability and improve the chances of successful fusion, particularly in cases with significant disc degeneration or segmental instability.
Resources
References
- ↑ Chun, Danielle S.; Baker, Kevin C.; Hsu, Wellington K. (2015-10). "Lumbar pseudarthrosis: a review of current diagnosis and treatment". Neurosurgical Focus. 39 (4): E10. doi:10.3171/2015.7.FOCUS15292. ISSN 1092-0684. PMID 26424334. Check date values in:
|date=(help) - ↑ 2.0 2.1 Cruz, Alex; Ropper, Alexander E.; Xu, David S.; Bohl, Michael; Reece, Edward M.; Winocour, Sebastian J.; Buchanan, Edward; Kaung, Geoffrey (2021-02). "Failure in Lumbar Spinal Fusion and Current Management Modalities". Seminars in Plastic Surgery. 35 (1): 54–62. doi:10.1055/s-0041-1726102. ISSN 1535-2188. PMC 8110346. PMID 33994880. Check date values in:
|date=(help) - ↑ Heggeness, M. H.; Esses, S. I. (1991-08). "Classification of pseudarthroses of the lumbar spine". Spine. 16 (8 Suppl): S449–454. ISSN 0362-2436. PMID 1785103. Check date values in:
|date=(help) - ↑ DePalma, A. F.; Rothman, R. H. (1968). "The nature of pseudarthrosis". Clinical Orthopaedics and Related Research. 59: 113–118. ISSN 0009-921X. PMID 5665452.
- ↑ Kornblum, Martin B.; Fischgrund, Jeffrey S.; Herkowitz, Harry N.; Abraham, David A.; Berkower, David L.; Ditkoff, Jeff S. (2004-04-01). "Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis". Spine. 29 (7): 726–733, discussion 733–734. doi:10.1097/01.brs.0000119398.22620.92. ISSN 1528-1159. PMID 15087793.
- ↑ Kornblum, Martin B.; Fischgrund, Jeffrey S.; Herkowitz, Harry N.; Abraham, David A.; Berkower, David L.; Ditkoff, Jeff S. (2004-04-01). "Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis". Spine. 29 (7): 726–733, discussion 733–734. doi:10.1097/01.brs.0000119398.22620.92. ISSN 1528-1159. PMID 15087793.
- ↑ Albert, T. J.; Pinto, M.; Denis, F. (2000-01). "Management of symptomatic lumbar pseudarthrosis with anteroposterior fusion. A functional and radiographic outcome study". Spine. 25 (1): 123–129, discussion 130. doi:10.1097/00007632-200001010-00021. ISSN 0362-2436. PMID 10647170. Check date values in:
|date=(help)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


