Lumbar Radicular Pain and Radiculopathy: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{stub}} | {{stub}} | ||
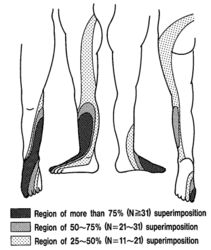
Radicular pain is generated by discharges from a dorsal root or dorsal root ganglion. Inflammation plays an important role as simple compression does not necessarily result in pain. Radicular pain may or may not be associated with radiculopathy. Disc herniation is the most common cause of radicular pain. The pain is often described as travelling along the length of the limb in a narrow band two to three inches wide.<ref>{{#pmid:19762151}}</ref> L4, L5, and S1 pain patterns have significant overlapping pain areas. | Radicular pain is generated by discharges from a dorsal root or dorsal root ganglion. Inflammation plays an important role as simple compression does not necessarily result in pain. Radicular pain may or may not be associated with radiculopathy. Disc herniation is the most common cause of radicular pain. The pain is often described as travelling along the length of the limb in a narrow band two to three inches wide.<ref>{{#pmid:19762151}}</ref> L4, L5, and S1 pain patterns have significant overlapping pain areas. | ||
== | == Aetiology == | ||
Disc herniation is the cause in 98% of cases. The nerve roots can be compressed anywhere along their length but this most commonly occurs in the lateral recess and in the foramen. A large number of other conditions make up the remaining 2% of causes. | |||
{| class="wikitable" | |||
|+Causes of Radiculopathy<ref name="bogduk">Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Chapter 15. Edinburgh: Elsevier/Churchill Livingstone, 2012</ref> | |||
|- | |||
! Condition !! Cause | |||
|- | |||
|Disc Disorders | |||
|Disc Herniation | |||
|- | |||
| Foraminal Stenosis ||<ul><li>Vertical subluxation of vertebrae</li><li>Osteophytes form disc</li><li>Osteophytes from facet joint</li><li>Buckled ligamentum flavum</li><li>Cyst of ligamentum flavum</li><li>Slipped inferior articular epiphysis</li><li>Ganglion</li><li>Synovial tumour</li><li>Infections and tumours of vertebrae</li><li>Paget's disease</li><li>Facet joint lipoma</li></ul> | |||
|- | |||
| Epidural Disorders ||<ul><li>Lipoma</li><li>Angioma</li><li>Infections</li></ul> | |||
|- | |||
| Meningeal Disorders ||<ul><li>Cysts of the nerve root sleeve</li><li>Intradural ossification</li></ul> | |||
|- | |||
| Neurological Disorders ||<ul><li>Diabetes</li><li>Cysts and tumours</li><li>Infections</li><li>Tabes dorsalis</li></ul> | |||
|} | |||
=== Lateral Recess Stenosis === | |||
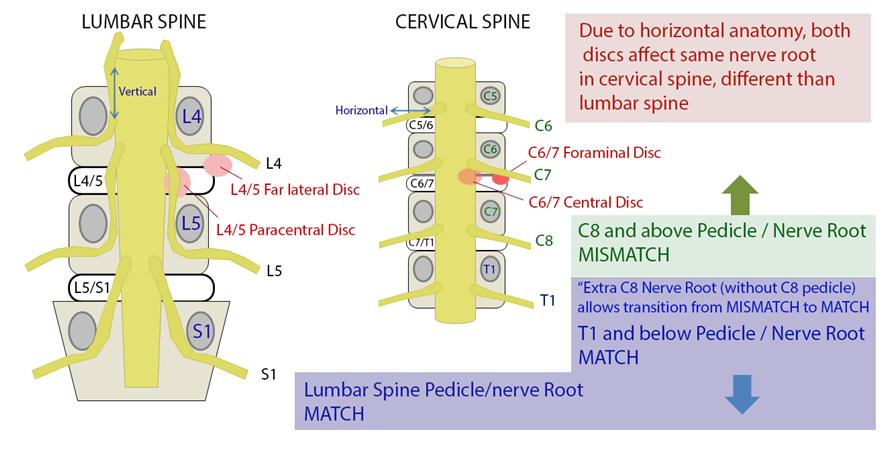
In lateral recess stenosis it is the descending nerve root that is irritated or compressed. For example in L4/5 disc prolapse affecting the lateral recess, it is the descending L5 nerve root that is at risk not the exiting L4 nerve root. | |||
=== | <gallery mode="packed" heights="350"> | ||
Furman et al in 2019 mapped lower limb radicular symptoms based on inadvertent pain patterns during supraneural transforaminal injections, the data is modified in table format below. | File:Nerve roots relationship.jpg|The relationship between nerve roots and spinal anatomy | ||
</gallery> | |||
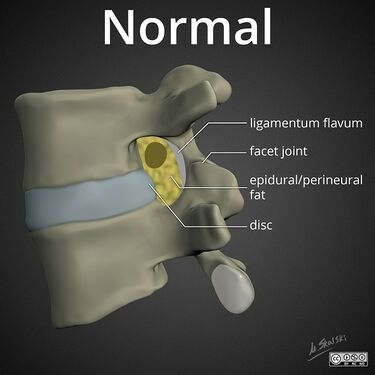
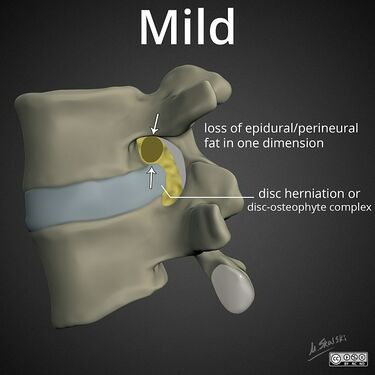
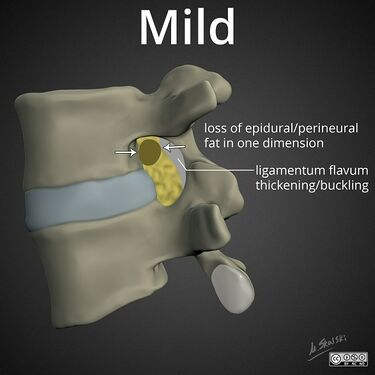
=== Foraminal Stenosis === | |||
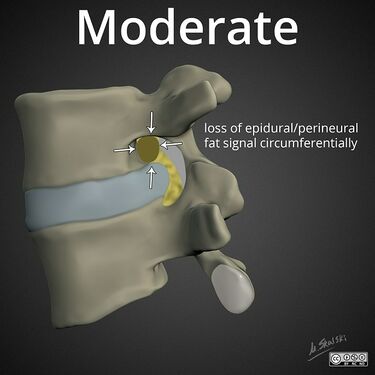
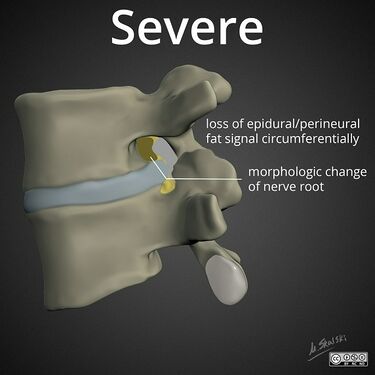
Less commonly the exiting nerve root is irritated or compressed in the foramen.<gallery mode="packed" heights="250px"> | |||
File:lumbar-neuroforaminal-stenosis-normal.jpg|Normal: fat surrounds nerve root | |||
File:lumbar-neuroforaminal-stenosis-mild-disc.jpg|Mild: partial loss of perineural fat signal | |||
File:lumbar-neuroforaminal-stenosis-mild-ligamentum-flavum.jpg|Mild: partial loss of perineural fat signal | |||
File:lumbar-neuroforaminal-stenosis-moderate.jpg|Moderate: circumferential lost of perineural fat signal | |||
File:lumbar-neuroforaminal-stenosis-severe.jpg|Severe: circumferential lost of perineural fat signal with compression of the nerve root | |||
</gallery> | |||
== Pathophysiology == | |||
{{See also|Radicular Pain and Radiculopathy}} | |||
[[Radicular Pain and Radiculopathy|Radiculopathy]] occurs when conduction is blocked in the axons of a spinal nerve or its roots. When the sensory axons are affected the patient develops numbness, while when the motor axons are affected then weakness develops. Radiculopathy can be a result of compression or ischaemia. Radiculopathy does not cause pain in either the back or the legs in the absence of inflammation. It is purely a neurological loss. Radiculopathy may be associated with [[Somatic Referred Pain|somatic referred pain]] or with [[Radicular Pain and Radiculopathy|radicular pain]].<ref name="bogduk" /> | |||
Acute mechanical compression of a ''dorsal root ganglion'' causes ectopic activity in Aδ, C and Aβ fibres. This multimodal activation causes a distinctive quality that is shooting or electric in nature. However acute compression of a nerve root only results in brief activity of nociceptive fibres | |||
The evidence favours tension in sensitised nerve roots as the cardinal mechanism of radicular pain. Chronic compression of a nerve root can result in it becoming sensitised to mechanical stimuli. Possible mechanisms include partial damage to axons, neuroma-in-continuity, focal demyelination, intraneural oedema, and impaired microcirculation. | |||
The nucleus pulposus is inflammatogenic and leucotatic. Cultured disc material produces nitric oxide. If nucleus pulposus is applied to a dorsal root ganglion then there is discharge in Aδ and Aβ fibres. Nucleus pulposus in the epidural space causes a delay in nerve conduction velocity, however intravenous methylprednisolone 24 hours prior to this prevents this. Nucleus pulposus in the epidural space results in mechanical hyperalgesia which correlates with prostaglandin A2 immunoreactivity. Annulus fibrosus and nucleus pulposus in the epidural space results in thermal hyperalgesia which correlates with nitric oxide levels in the disc material, but mechanical ''hypo''algesia. | |||
== Clinical Features == | |||
[[Radicular Pain and Radiculopathy|Radicular pain]] is distinct from [[Somatic Referred Pain|somatic referred pain]]. Radicular pain is shooting and band-like. Somatic referred pain on the other hand is constant in position, poorly localised, diffuse, and aching in quality.<ref name="bogduk" /> | |||
===Pain Pattern=== | |||
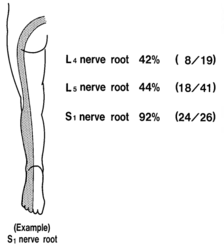
The pattern of lumbar radicular pain is ''not'' [[Dermatomes|dermatomal]], but rather ''dynatomal.'' Furman et al in 2019 mapped lower limb radicular symptoms based on inadvertent pain patterns during supraneural transforaminal injections, the data is modified in table format below. Unfortunately they did not use detailed grid based mapping like Slipman and colleagues did for the cervical spine. Furman found that pain patterns can't predict the nerve root level for the lumbar spine. The buttock is a very common pain referral location across all nerve roots, while pain in the thigh and leg frequently follows dermatomal distributions.<ref>{{#pmid:29800710}}</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
| Line 37: | Line 81: | ||
|Foot || style="background: #ffffff;"|0% || style="background: #F4FFFF;"|3% || style="background: #ffffff;"|0% || style="background: #ffffff;"|0% | |Foot || style="background: #ffffff;"|0% || style="background: #F4FFFF;"|3% || style="background: #ffffff;"|0% || style="background: #ffffff;"|0% | ||
|} | |} | ||
Pain below the knee is a non-specific indicator of radiculopathy as it can occur in other conditions such as somatic referred pain. A careful history should be elicited to distinguish between somatic referred and radicular pain with regards to the pain quality, distribution, pattern, and depth. | |||
{{Somatic Referred vs Radicular Pain}} | |||
== | ===Neurological Examination=== | ||
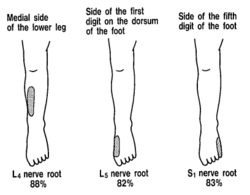
'''Sensory loss''' patterns were evaluated by Nitta and colleagues through fluoroscopically guided spinal nerve anaesthetic blocks in patients with radicular pain. They found the following sensory deficits.<ref>{{#pmid:8235861}}</ref> This is not necessarily what typically occurs in patients not undergoing selective nerve root blocks, but simply the [[dermatomes]] for the nerve roots. | |||
<gallery widths="250" heights="250"> | <gallery widths="250" heights="250"> | ||
File:L4 nerve block sensory deficit Nitta.png|L4 block pattern: Extending from the midline of the trunk posteriorly, across the buttock, through the lateral and anterior side of the thigh and the medial side of the leg to the first digit of the foot. | File:L4 nerve block sensory deficit Nitta.png|L4 block pattern: Extending from the midline of the trunk posteriorly, across the buttock, through the lateral and anterior side of the thigh and the medial side of the leg to the first digit of the foot. | ||
| Line 61: | Line 94: | ||
</gallery> | </gallery> | ||
==Treatment== | |||
== Treatment == | |||
===Injections=== | ===Injections=== | ||
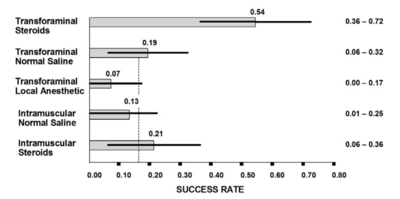
[[File:Lumbar TFI success rates Ghahreman 2010 chart.png|thumb|400x400px|The categorical success rates at one month (and 95% CI) from a randomised trial comparing various injections for radicular pain. The dotted vertical line is the average response rate of the lower four interventions.<ref name=":0" />]] | [[File:Lumbar TFI success rates Ghahreman 2010 chart.png|thumb|400x400px|The categorical success rates at one month (and 95% CI) from a randomised trial comparing various injections for radicular pain. The dotted vertical line is the average response rate of the lower four interventions.<ref name=":0" />]] | ||
Revision as of 17:13, 17 September 2021
Radicular pain is generated by discharges from a dorsal root or dorsal root ganglion. Inflammation plays an important role as simple compression does not necessarily result in pain. Radicular pain may or may not be associated with radiculopathy. Disc herniation is the most common cause of radicular pain. The pain is often described as travelling along the length of the limb in a narrow band two to three inches wide.[1] L4, L5, and S1 pain patterns have significant overlapping pain areas.
Aetiology
Disc herniation is the cause in 98% of cases. The nerve roots can be compressed anywhere along their length but this most commonly occurs in the lateral recess and in the foramen. A large number of other conditions make up the remaining 2% of causes.
| Condition | Cause |
|---|---|
| Disc Disorders | Disc Herniation |
| Foraminal Stenosis |
|
| Epidural Disorders |
|
| Meningeal Disorders |
|
| Neurological Disorders |
|
Lateral Recess Stenosis
In lateral recess stenosis it is the descending nerve root that is irritated or compressed. For example in L4/5 disc prolapse affecting the lateral recess, it is the descending L5 nerve root that is at risk not the exiting L4 nerve root.
Foraminal Stenosis
Less commonly the exiting nerve root is irritated or compressed in the foramen.
Pathophysiology
- See also: Radicular Pain and Radiculopathy
Radiculopathy occurs when conduction is blocked in the axons of a spinal nerve or its roots. When the sensory axons are affected the patient develops numbness, while when the motor axons are affected then weakness develops. Radiculopathy can be a result of compression or ischaemia. Radiculopathy does not cause pain in either the back or the legs in the absence of inflammation. It is purely a neurological loss. Radiculopathy may be associated with somatic referred pain or with radicular pain.[2]
Acute mechanical compression of a dorsal root ganglion causes ectopic activity in Aδ, C and Aβ fibres. This multimodal activation causes a distinctive quality that is shooting or electric in nature. However acute compression of a nerve root only results in brief activity of nociceptive fibres
The evidence favours tension in sensitised nerve roots as the cardinal mechanism of radicular pain. Chronic compression of a nerve root can result in it becoming sensitised to mechanical stimuli. Possible mechanisms include partial damage to axons, neuroma-in-continuity, focal demyelination, intraneural oedema, and impaired microcirculation.
The nucleus pulposus is inflammatogenic and leucotatic. Cultured disc material produces nitric oxide. If nucleus pulposus is applied to a dorsal root ganglion then there is discharge in Aδ and Aβ fibres. Nucleus pulposus in the epidural space causes a delay in nerve conduction velocity, however intravenous methylprednisolone 24 hours prior to this prevents this. Nucleus pulposus in the epidural space results in mechanical hyperalgesia which correlates with prostaglandin A2 immunoreactivity. Annulus fibrosus and nucleus pulposus in the epidural space results in thermal hyperalgesia which correlates with nitric oxide levels in the disc material, but mechanical hypoalgesia.
Clinical Features
Radicular pain is distinct from somatic referred pain. Radicular pain is shooting and band-like. Somatic referred pain on the other hand is constant in position, poorly localised, diffuse, and aching in quality.[2]
Pain Pattern
The pattern of lumbar radicular pain is not dermatomal, but rather dynatomal. Furman et al in 2019 mapped lower limb radicular symptoms based on inadvertent pain patterns during supraneural transforaminal injections, the data is modified in table format below. Unfortunately they did not use detailed grid based mapping like Slipman and colleagues did for the cervical spine. Furman found that pain patterns can't predict the nerve root level for the lumbar spine. The buttock is a very common pain referral location across all nerve roots, while pain in the thigh and leg frequently follows dermatomal distributions.[3]
| Nerve Root | L3 | L4 | L5 | S1 |
|---|---|---|---|---|
| Buttock | 45% | 43% | 62% | 64% |
| Groin | 0% | 3% | 0% | 0% |
| Anterior Thigh | 27% | 29% | 12% | 0% |
| Posterior Thigh | 36% | 25% | 59% | 36% |
| Medial Thigh | 18% | 11% | 3% | 0% |
| Lateral Thigh | 0% | 14% | 9% | 0% |
| Knee | 9% | 7% | 6% | 9% |
| Anterior Leg | 0% | 14% | 3% | 0% |
| Posterior Leg | 18% | 18% | 50% | 45% |
| Medial Leg | 0% | 7% | 6% | 0% |
| Lateral Leg | 9% | 14% | 24% | 0% |
| Foot | 0% | 3% | 0% | 0% |
Pain below the knee is a non-specific indicator of radiculopathy as it can occur in other conditions such as somatic referred pain. A careful history should be elicited to distinguish between somatic referred and radicular pain with regards to the pain quality, distribution, pattern, and depth.
| Somatic Referred | Radicular | |
|---|---|---|
| Pain quality | Dull, deep ache, or pressure-like, perhaps like an expanding pressure | Shooting, lancinating, or electric-shocks |
| Relation to back pain | Referred pain is always concurrent with back pain. If the back pain ceases then so does the referred pain. If the back pain flares then so does the leg pain intensity and spatial spread. | Not always concurrent with back pain. |
| Distribution | Anywhere in the lower limb, fixed in location, commonly in the buttock or proximal thigh. Spread of pain distal to the knee can occur when severe even to the foot, and it can skip regions such as the thigh. It can feel like an expanding pressure into the lower limb, but remains in location once established without traveling. It can wax and wane, but does so in the same location. | Entire length of lower limb, but below knee > above knee. In mild cases the pain may be restricted proximally. |
| Pattern | Felt in a wide area, with difficult to perceive boundaries, often demonstrated with an open hand rather than pointing finger. The centres in contrast can be confidently indicated. | Travels along a narrow band no more than 5-8 cm wide in a quasi-segmental fashion but not related to dermatomes (dynatomal). |
| Depth | Deep only, lacks any cutaneous quality | Deep as well as superficial |
| Neurological signs | Not characteristic | Favours radicular pain, but not required. |
| Neuroanatomical basis | Discharge of the peripheral nerve endings of Aδ and C fibres from the lower back converge onto second order neurons in the dorsal horn that also receive input from from the lower limb, and so the frontal lobe has no way of knowing where the pain came from. | Heterotopic discharge of Aδ, Aβ, and C fibres through stimulation of a dorsal root or dorsal root ganglion of a spinal nerve, typically in the presence of inflammation, with pain being felt in the peripheral innervation of the affected nerve |
Neurological Examination
Sensory loss patterns were evaluated by Nitta and colleagues through fluoroscopically guided spinal nerve anaesthetic blocks in patients with radicular pain. They found the following sensory deficits.[5] This is not necessarily what typically occurs in patients not undergoing selective nerve root blocks, but simply the dermatomes for the nerve roots.
Treatment
Injections
- Main article: Lumbar Transforaminal Epidural Injection
The Pain Physician Epidural Guidelines concluded that there is level I evidence for caudal epidural, lumbar interlaminar epidural, and lumbar transforaminal epidural injections[7]
Some systematic reviews have used mean pain scores to show only modest benefit of epidural injections[8] but this is a misleading measure. More useful are categorical outcomes, i.e. what percentage responded. The systematic reviews also have tended to combine all types of epidurals.
There is good evidence that transforaminal epidural corticosteroid injections (TFIs) are effective[9][10][6], and safe[11] in the short term. Using categorical data, lumbar TFIs are effective in about 50% of patients.[6] Because half the treated sample responds well while the other half does not the mean scores misleadingly tells you that it isn't effective. There is no evidence supporting that epidural injections are effective in the long term, however epidural injections can be repeated.
5% dextrose is more effective than saline but the effect wanes at two weeks.[12]
Surgery
Microdiscectomy is superior to nonoperative care (including epidural injection) if it is doing between 4-12 months for leg pain up to 12 months.[13] It is not generally recommended before 4 months, it may lead to more rapid relief of pain but the superiority is not sustained.[14][15]
References
- ↑ Bogduk. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain 2009. 147:17-9. PMID: 19762151. DOI.
- ↑ 2.0 2.1 2.2 Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Chapter 15. Edinburgh: Elsevier/Churchill Livingstone, 2012
- ↑ Furman & Johnson. Induced lumbosacral radicular symptom referral patterns: a descriptive study. The spine journal : official journal of the North American Spine Society 2019. 19:163-170. PMID: 29800710. DOI.
- ↑ Bogduk et al. Medical Management of Acute and Chronic Low Back Pain: An Evidence Based Approach. Elsevier Science. 2002
- ↑ Nitta et al.. Study on dermatomes by means of selective lumbar spinal nerve block. Spine 1993. 18:1782-6. PMID: 8235861. DOI.
- ↑ 6.0 6.1 6.2 Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010 Aug;11(8):1149-68. doi: 10.1111/j.1526-4637.2010.00908.x. PMID: 20704666.
- ↑ Manchikanti L, et al. Epidural Interventions in the Management of Chronic Spinal Pain: American Society of Interventional Pain Physicians (ASIPP) Comprehensive Evidence-Based Guidelines. Pain Physician. 2021 Jan;24(S1):S27-S208. PMID: 33492918.
- ↑ Oliveira CB, Maher CG, Ferreira ML, Hancock MJ, Oliveira VC, McLachlan AJ, Koes BW, Ferreira PH, Cohen SP, Pinto RZ. Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst Rev. 2020 Apr 9;4(4):CD013577. doi: 10.1002/14651858.CD013577. PMID: 32271952; PMCID: PMC7145384.
- ↑ MacVicar et al.. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain medicine (Malden, Mass.) 2013. 14:14-28. PMID: 23110347. DOI.
- ↑ Kaufmann et al.. Clinical effectiveness of single lumbar transforaminal epidural steroid injections. Pain medicine (Malden, Mass.) 2013. 14:1126-33. PMID: 23895182. DOI.
- ↑ El-Yahchouchi et al.. Adverse Event Rates Associated with Transforaminal and Interlaminar Epidural Steroid Injections: A Multi-Institutional Study. Pain medicine (Malden, Mass.) 2016. 17:239-49. PMID: 26593277. DOI.
- ↑ Maniquis-Smigel et al.. Short Term Analgesic Effects of 5% Dextrose Epidural Injections for Chronic Low Back Pain: A Randomized Controlled Trial. Anesthesiology and pain medicine 2017. 7:e42550. PMID: 28920043. DOI. Full Text.
- ↑ Bailey CS, Rasoulinejad P, Taylor D, Sequeira K, Miller T, Watson J, Rosedale R, Bailey SI, Gurr KR, Siddiqi F, Glennie A, Urquhart JC. Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months. N Engl J Med. 2020 Mar 19;382(12):1093-1102. doi: 10.1056/NEJMoa1912658. PMID: 32187469.
- ↑ Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008 Jun 14;336(7657):1355-8. doi: 10.1136/bmj.a143. Epub 2008 May 23. PMID: 18502911; PMCID: PMC2427077.
- ↑ Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine (Phila Pa 1976). 2006 Oct 1;31(21):2409-14. doi: 10.1097/01.brs.0000239178.08796.52. PMID: 17023847.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,