Lumbar Radicular Pain and Radiculopathy
Radicular pain is generated by discharges from a dorsal root or dorsal root ganglion. Inflammation plays an important role as simple compression does not necessarily result in pain. Radicular pain may or may not be associated with radiculopathy. Disc herniation is the most common cause of radicular pain. The pain is often described as travelling along the length of the limb in a narrow band two to three inches wide.[1] L4, L5, and S1 pain patterns have significant overlapping pain areas.
Clinical Features
Radicular pain is distinct from somatic referred pain. Radicular pain is shooting and band-like. Somatic referred pain on the other hand is constant in position, poorly localised, diffuse, and aching in quality.[2]
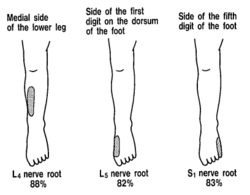
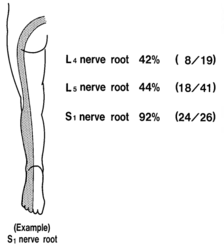
Sensory Deficit Maps with Nerve Block
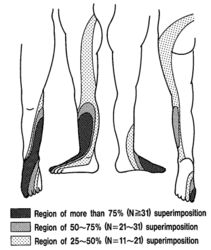
In 1993 Nitta et al looked at dermatome patterns by doing fluoroscopically guided spinal nerve anaesthetic blocks in patients with radicular pain. They found the following sensory deficits.[3]
Inadvertent Pain Maps during TFI
Furman et al in 2019 mapped lower limb radicular symptoms based on inadvertent pain patterns during supraneural transforaminal injections, the data is modified in table format below. They confirmed that history and pain charts cannot predict the nerve root level. The buttock is a very common pain referral location across all nerve roots, while pain in the thigh and leg frequently follows dermatomal distributions. A significant limitation of the study is that injectate in transforaminal injections frequently traverses segment levels.[4]
| Nerve Root | L3 | L4 | L5 | S1 |
|---|---|---|---|---|
| Buttock | 45% | 43% | 62% | 64% |
| Groin | 0% | 3% | 0% | 0% |
| Anterior Thigh | 27% | 29% | 12% | 0% |
| Posterior Thigh | 36% | 25% | 59% | 36% |
| Medial Thigh | 18% | 11% | 3% | 0% |
| Lateral Thigh | 0% | 14% | 9% | 0% |
| Knee | 9% | 7% | 6% | 9% |
| Anterior Leg | 0% | 14% | 3% | 0% |
| Posterior Leg | 18% | 18% | 50% | 45% |
| Medial Leg | 0% | 7% | 6% | 0% |
| Lateral Leg | 9% | 14% | 24% | 0% |
| Foot | 0% | 3% | 0% | 0% |
Radiculopathy
Radiculopathy occurs when conduction is blocked in the axons of a spinal nerve or its roots. When the sensory axons are affected the patient develops numbness, while when the motor axons are affected then weakness develops. Radiculopathy can be a result of compression or ischaemia. Radiculopathy does not cause pain in either the back or the legs. It is purely a neurological loss. Radiculopathy may be associated with somatic referred pain or with radicular pain.[2]
| Condition | Cause |
|---|---|
| Foraminal Stenosis |
|
| Epidural Disorders |
|
| Meningeal Disorders |
|
| Neurological Disorders |
|
| Disc Disorders | Disc Herniation |
Treatment
Injections
- Main article: Lumbar Transforaminal Epidural Injection
There is good evidence that transforaminal epidural corticosteroid injections are effective[5][6], and safe.[7] Other reviews have used mean pain scores but this is a highly misleading measure. More useful is categorical outcomes, and with this measure TFIs are shown to be effective in about 50% of patients. If half the treated sample responds well but the other half does not then a mean score will tell you it isn't effective.
Transforaminal injection of steroid and local anaesthetic is more effective than transforaminal injection of local anaesthetic, normal saline, and intramuscular injection of steroid or normal saline.[8] 5% dextrose is more effective than saline but the effect wanes at two weeks.[9]
References
- ↑ Bogduk. On the definitions and physiology of back pain, referred pain, and radicular pain. Pain 2009. 147:17-9. PMID: 19762151. DOI.
- ↑ 2.0 2.1 2.2 Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Chapter 15. Edinburgh: Elsevier/Churchill Livingstone, 2012
- ↑ Nitta et al.. Study on dermatomes by means of selective lumbar spinal nerve block. Spine 1993. 18:1782-6. PMID: 8235861. DOI.
- ↑ Furman & Johnson. Induced lumbosacral radicular symptom referral patterns: a descriptive study. The spine journal : official journal of the North American Spine Society 2019. 19:163-170. PMID: 29800710. DOI.
- ↑ MacVicar et al.. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain medicine (Malden, Mass.) 2013. 14:14-28. PMID: 23110347. DOI.
- ↑ Kaufmann et al.. Clinical effectiveness of single lumbar transforaminal epidural steroid injections. Pain medicine (Malden, Mass.) 2013. 14:1126-33. PMID: 23895182. DOI.
- ↑ El-Yahchouchi et al.. Adverse Event Rates Associated with Transforaminal and Interlaminar Epidural Steroid Injections: A Multi-Institutional Study. Pain medicine (Malden, Mass.) 2016. 17:239-49. PMID: 26593277. DOI.
- ↑ Ghahreman et al.. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain medicine (Malden, Mass.) 2010. 11:1149-68. PMID: 20704666. DOI.
- ↑ Maniquis-Smigel et al.. Short Term Analgesic Effects of 5% Dextrose Epidural Injections for Chronic Low Back Pain: A Randomized Controlled Trial. Anesthesiology and pain medicine 2017. 7:e42550. PMID: 28920043. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,