Lumbar Transforaminal Epidural Steroid Injection

| |
| Lumbar Transforaminal Epidural Steroid Injection | |
|---|---|
| Indication | Lumbar Radicular Pain |
| Syringe | 3 x 3mL syringes |
| Needle | Spinal needle e.g. 22-25g Quincke tip |
| Steroid | Dexamethasone 8mg in 1mL or 12mg in 1.5mL |
| Local | 1-2mL of 1-2% lidocaine as test dose |
| Volume | 3-8mL |
There are a variety of methods for epidural steroid injection for the treatment of lumbar radicular pain. The highest quality outcome data are weighted towards the transforaminal technique. The transforaminal approach targets medication delivery to the ventral epidural space.
Alternative epidural delivery options are interlaminar, and caudal injection.
Anatomy
A good understanding of lumbar spine anatomy is essential for safe and effective epidural injection.
The epidural space has dorsal and ventral compartments.
- The ventral/anterior compartment is bordered by the vertebral body anteriorly and the thecal sac posteriorly.
- The dorsal/posterior compartment is bordered by the thecal sac anteriorly and the ligamentum flavum and laminae posteriorly.
The epidural space contains adipose tissue, loose areolar tissue, arteries, lymph vessels, and venous plexus. There is a a proportionally greater amount of adipose tissue inside the dural sleeve than in the epidural space.
Intervertebral Foramen
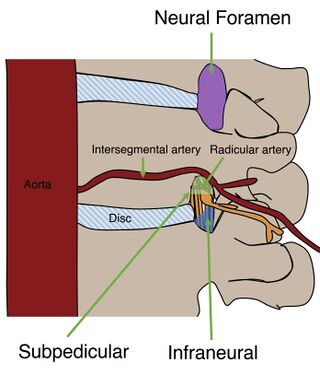
The intervertebral foramen is bordered anteriorly by the caudal half of the most cranial of the two vertebral bodies, intervertebral disc, and the cranial half of the most caudal of the two vertebral bodies. It is bordered posteriorly by the facet joint, lamina, and ligamentum flavum. It is bordered superiorly and inferiorly by the pedicles of the adjacent vertebrae.
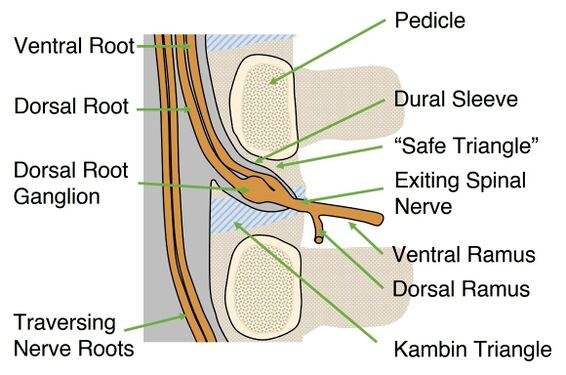
The fat-containing "safe triangle", in the AP view, is formed inferomedially by the spinal nerve and superiorly by the pedicle. The traditional safe triangle is the anterior superior quadrant of the foramen. The term "safe" in safe triangle is actually misnomer. The term originally referred to being furthest away from the nerve root. However the anterior superior quadrant is the area where a radicular artery is most likely to be located. If the needle is kept in the posterosuperior quadrant then it is less likely to hit a vessel.[1] Some authors have even gone so far as to rename it the "unsafe triangle."[2]
Kambin's triangle in the inferior third of the foramen is the injection location for the alternative infraneural approach. It is a right angle triangle over the dorsolateral disc, with the hypotenuse of the triangle being the exiting nerve root, the adjacent side being the superior border of the caudal vertebra, and the opposite side being the traversing nerve root. It is theorised to be safer than the "safe triangle" due to the lack of radicular branches in the area, and also has the additional advantage of being at the nerve-disc interface.
The exiting nerve root sits cranial in the foramen - cranial to the disc and caudal to the pedicle. It is surrounded by a dural sleeve which is made up of dura and arachnoid mater. The dural sleeve extends as far as the foramen. The nerve root usually does not sit in the safe triangle. However in spinal stenosis the nerve root may move cephalad.
Within the foramen the dorsal and ventral nerve roots join to form the spinal nerve. The spinal nerve then ramifies into the dorsal and ventral rami.
Spinal nerves exit below their corresponding vertebral bodies. For example the L4 spinal nerve exits from the L4/5 foramen below the L4 pedicle and transverse process. The L5 nerve root traverses through this region before exiting at the L5/S1 foramen.
The anterior segmental artery is most likely to sit in the anterior superior quadrant of the neural foramen (96% of the time). © 2017 by American Journal of Neuroradiology.[1]
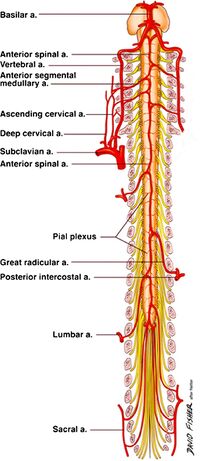
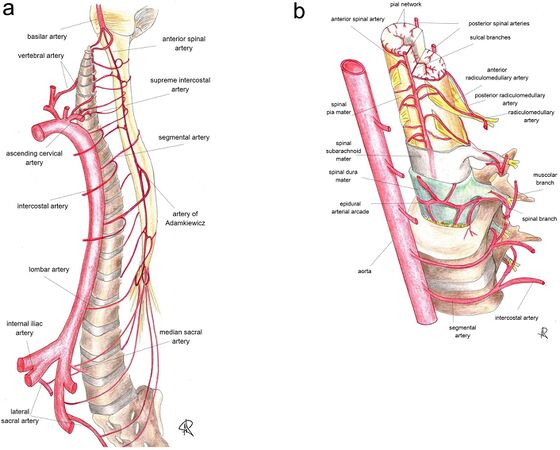
Blood Vessels
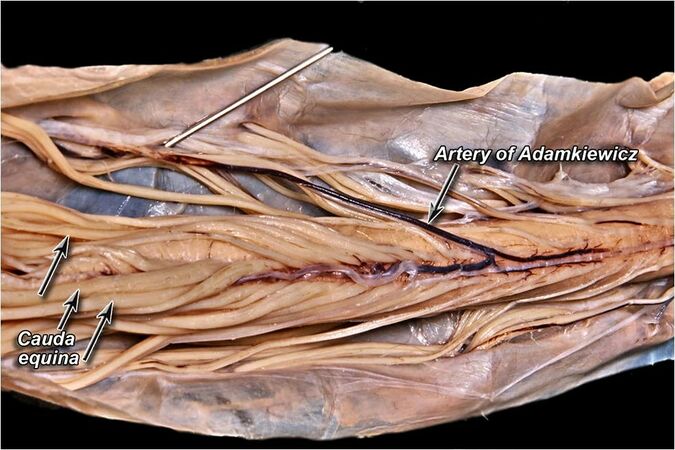
The arterial supply is of particular importance. Anterior segmental arteries enter through the foramen as radicular arteries and travel along the nerve roots into the thecal sac. There are multiple radicular arteries however most people (~85%) have one that is dominant known as the Artery of Adamkiewicz. It is also known as the great anterior radiculomedullary artery, great radicular artery, great anterior segmental medullary artery, amongst other names.
The artery of adamkiewciz varies in origin, typically arising from a spinal branch of the lower posterior intercostal arteries (T8-11), the subcostal artery (T12), or from an upper lumbar artery (L1). However it can arise as high as T3 and as low as L4.[3] It usually arises from the left side, with left-sided rates of 77%[3] and 88%[4] having been reported.
It runs along the course of the ventral root of the spinal cord, medially, through the intervertebral foramen. The distal portion forms a characteristic "hairpin" turn together with the anterior spinal artery.
The artery feeds into the anterior spinal artery and also provides a smaller branch to the posterior spinal artery. This artery thus provides much of the blood to the spinal cord, with it possibly being the main supply to the lower two thirds of the spinal cord from T8 to the conus medullaris.
Any one radiculomedullary artery can be a regular artery or the artery of adamkiewicz. In most cases the segmental vessels are found in the anterior compartment and so it is recommended to inject in the posterior compartment. In 97% of cases the radiculomedullary arteries are in the superior half of the foramen, and never in the lower fifth.[1]
Indications and Efficacy
There have been many proposed mechanisms for the effect of epidural steroid injections. They include anti-inflammatory effects, anti-nociceptive effects (blocking of C-fibre transmission[5]), suppression of immune response, mechanical debridement (washing away of inflammatory mediators), stopping the "pain-spasm" cycle, and placebo effect.
Radicular Pain
The primary indication for transforaminal epidural steroid injection is for lower extremity radicular pain due to lumbar disc herniation in patients:[6]
- who require pain relief
- who have had a failed response to non-surgical intervention or non-surgical interventions aren't indicated
- whose pain likely has an inflammatory basis.
- whose symptoms are consistent with lumbar or sacral radicular pain and may or may not have radiculopathy.
- who have imaging findings that support the diagnosis of radicular pain
Probably the most important efficacy study is that by Ghahreman and colleagues.[7] It was a randomised controlled study where they compared transforaminal steroid with a variety of other control groups. Transforaminal steroid with local anaesthetic resulted in a successful primary outcome 54% of the time and was more effective than the control groups. Success was defined as at least 50% relief one month post injection.
A 2013 systematic review looked at 6 RCTs, 5 pragmatic comparative trials, and 12 observational trials. They found that up to 70% achieve 50% or more greater pain relief at 1 to 2 months, up to 30% experience complete relief, injections reduce health care consumption, are surgery sparing, are cost effective, and can be durable with 25-40% having 12 months of relief. The procedure is slightly more effective for acute than chronic pain. 69% of patients with acute pain had benefit, compared to 57% with chronic pain. They also concluded that the transforaminal approach was better than caudal, interlaminar, and blind injections.[8]
Non-Evidence Based Indications
Spinal Stenosis
Epidural steroid injection is less effective for spinal stenosis. For example in one 2004 study of mixed caudal/transforaminal patients only around one third having relief of greater than 2 months, one third having relief of less than 2 months, and one third having no relief. There was an overall small magnitude of change.[9] However a pivotal 2014 RCT showed that there was no difference for pain or disability at 6 weeks between the steroid-anaesthetic group and anaesthetic only group.[10]
Axial Pain
There is no evidence for the use of epidural corticosteroid in the treatment of axial pain such as that arising from a disc, zygapophyseal joint, or other surrounding structures.
Contraindications
Contraindications as outlined by the SIS guidelines are:[6]
- Absolute contraindications
- Informed consent not possible
- Not possible to use contrast medium
- Untreated local infection
- Patient non-cooperation despite consent.
- Pregnancy due to fluoroscopic use
- Relative contraindications
- Coagulopathy
- Anatomical abnormalities precluding safe intervention
- Systemic infection
- Significant cardiorespiratory compromise
- Immunosuppression
Pre-procedural Evaluation
Medication is injected at the suspected pathologic site that correlates with the patient's clinical and radiological picture.
If the patient is on anticoagulants the doctor should weigh up the pros and cons of ceasing the agent prior to the procedure. Antiplatelets are not a significant risk for spinal procedures. For other anticoagulants there is usually a greater risk from ceasing the medication than the risk of adverse events from conducting the procedure while the patient is taking it. Guidelines are available to aide the clinician.[11]
Equipment
- Fluoroscopy machine
- Standard core disposables
- 22-25g x 3.5 inch or 5 inch quincke needle
- Contrast in 3mL syringe
- 2mL 0.125% bupivacaine or 1% lidocaine or 2% lidocaine in 3mL syringe
- 1 or 1.5mL of dexamethasone 8mg/mL in 3mL syringe
- Extension tube
Steroid Choice
The epidural administration of corticosteroids is off-label.
Most steroid preparations contain preservatives (polyethylene glycol and/or benzyl alcohol), however the clinical effect seems undetectable. All particular steroids have larger particles than RBCs, with betamethasone being the smallest. Dexamethasone is a solution with no particles and is the preferred agent used in New Zealand.
In one study comparing dexamethasone versus triamcinolone for transforaminal injection, no difference was found in efficacy between the groups at 2 weeks, 3 months, and 6 months in one RCT. However the dexamethasone group had slightly more people needing three injections to achieve the same outcomes, but most still only required 1 (~50%) or 2 injections (~30%) for symptomatic relief.[12]
Technique
Transforaminal epidural injections should be done in accordance with the Spine Intervention Society guidelines under fluoroscopic guidance. CT guidance is an alternative method typically used by radiologists rather than the fluoroscopic guidance used by most Musculoskeletal physicians. The traditional approach is the supraneural technique, with infraneural being an alternative option. Sedation is not advised, the patient should be able to have a conversation to avoid adverse events.
Fluoroscopically Guided Subpedicular (Supraneural) Approach
The subpedicular approach is the "classic" technique, also known as the "safe triangle" approach for L1-2 through to L5-S1. The needle is placed immediately underneath the pedicle, just above the exiting spinal nerve, and brought anteriorly to contact the vertebral body.
The safe triangle is the site of minimal risk for intrathecal or neural injury, however it is has a greater anatomical risk of arterial injury. Therefore the technique can be modified by using a supraneural approach. This approach has an identical trajectory but is not brought in contact with the vertebral body in order to reduce the risk of penetrating a radicular artery.
- Preparation
- Patient position is prone on the injection table, with the face in a comfortable position to allow for clear communication.
- Sterile preparation and drape area. The preferred agent for all spine procedures is 2% chlorhexidine in 70% alcohol.[13]
- Anaesthetise skin with 1% lidocaine.
- Target visualisation
- Centre the spinous process between the pedicles on AP view of the target disc space.
- Square off the target segment with the beam tangential to the inferior endplate of the upper of the two vertebrae of the target disc space (e.g. if target is L5 then square up inferior endplate of L5). This usually requires a cephalad tilt of the C-arm for the L4-5 and L5-1 segments, and a caudal tilt for the upper segments.
- Target position is just inferior to upper pedicle i.e. 6 o' clock, or slightly lateral to that point. This is the safe triangle area.
- However often the AP view does not offer an unobstructed needle path to the safe triangle, i.e. an "open look".
- Ipsilateral oblique (~25 degrees, exact amount depends on patient anatomy and level). Unobstructed needle path is visualised. The margins of the superior articular process, transverse process, and lamina should not overlap.
- Needle placement
- The needle insertion is marked In the ipsilateral oblique view, under the pedicle. In the oblique position the target point is shifted slightly laterally (e.g. ~5:30 on right sided injection).
- Infiltrate skin with 1-2mL of 1% lidocaine
- Needle placement for spinal needle is down the beam approaching the target.
- If deviate from directly down the beam then do so from a caudal-lateral to cephalad-medial direction.
- Intermittent fluoroscopy is used to check correct needle placement.
- The aim is to try and hit the lower border of the pedicle.
- Once bone contact has been made the needle should be slipped under the lower edge of the pedicle and advanced by 1mm.
- When the needle is thought to have reached the depth of the pars interarticularis, change to a true lateral position with pelvic lines superimposed
- On the true lateral advance the needle halfway across the pedicle. The needle tip should be in the safe triangle area. Staying in the posterior half is recommended because in most cases the vessels are found in the anterior half just dorsal to the vertebral body.
- Change back to AP view to confirm that the needle is still is in the correct 6 o clock position (or just lateral).
- The needle can be steered by rotating the needle bevel. The notch on the hub indicates the bevel direction, and it will usually steer away from this point. Some practitioners bend the needle to allow for easier manipulation. (See Needlecraft for Fluoroscopy)
- Injection
- Connect a low volume extension tube to the syringe
- Contrast: Inject contrast (e.g. 0.5-1mL of Omnipaque) under live fluoroscopy, using digital subtraction if available.
- Watch for the following flow patterns: venous, arterial, intrathecal, suboptimal, and epidural. Note that simultaneous epidural and vascular injection can occur.
- Venous pattern - reposition the needle usually by advancing it
- Arterial - abort the procedure
- Intrathecal - abort the procedure
- Sub-optimal distribution - adjust the needle
- You are wanting to see contrast outlining the spinal nerve and flow into the epidural space medial to the pedicle.
- Save contrast flow image in AP and lateral
- Local Anaesthetic Test Dose: Following contrast injection, inject a test dose local anaesthetic (e.g. 1-2mL of 1% or 2% preservative free lidocaine). Look for signs of spinal cord anaesthetisation.
- Steroid: If there is no central or contralateral neurologic change over the next 1-2 minutes steroid can then be injected. In New Zealand it is typically dexamethasone 8mg in 2mL or 12mg in 3mL.
- A total injectate volume of 3-4mL is the traditional approach. 4mL reaches the superior aspect of the intervertebral disc and inferior aspect of the inferior intervertebral disc 93% of the time.[14] A randomised trial found that 8mL was more effective than 3mL, however they only used 4mg of dexamethasone.[15] If larger volumes are used it is suggested to inject very slowly.
- Check washout AP image to verify that the contrast has been dispersed which means that the steroid has been delivered to the epidural space.
Fluoroscopically Guided Infraneural Approach
The infraneural technique (triangle of Kambin) is an alternative approach that some argue that is safer due to the lower chance of encountering the radicular artery. It is also known as the retrodiscal approach due to the close proximity of the needle tip to the posterior annulus. It is also described as preganglionic because the needle tip is proximal to the dorsal root ganglion.
It may result in a greater chance of depositing the medication at the nerve disc interface compared to the subpedicular approach. The injectate optimally transits inferomedially past a centrally herniated disc. Some authors argue that this should be the standard approach due to theorised greater safety and efficacy,[2] but there may be more posterior annular disc coverage but less foraminal coverage.[16] Some practitioners only use this approach when anatomical constraints prevent the subpedicular approach, or when injecting at L3 or above due to the higher likelihood of encountering the artery of Adamkiewicz.[17]
The initial needle trajectory is similar to that used in lumbar discography and has a risk of inadvertent disc entry.
- Target visualisation
- AP view through target disc space. Square off the targeted segment by lining up the superior endplate. This usually requires a cephalad tilt of the C-arm for the L4-5 and L5-1 segments, and a caudal tilt for the upper segments. Preferably line up the superior endplate inferior to the target.
- Oblique the fluoroscope ipsilaterally, i.e. towards the symptomatic side. Aim for the superior articular process to bisect the inferior endplate of the superior vertebral body.
- Target position is the junction of the superior articular process and superior endplate of the inferior vertebral body. This oblique position is the trajectory view.
- Needle placement
- Maintain the needle in the lower third of the foramen to avoid the spinal nerve, it may be placed as low as possible.
- Use the AP view to avoid dural puncture. The needle should not advance medially beyond the midpedicular line or the inferior pedicle'/s 12 o'clock position at its superior aspect.
- Use the lateral view to avoid inadvertent disc entry by using this view to advance the needle.
- Injection
Fluoroscopically Guided S1 Subpedicular Approach
S1 transforaminal injection is used for S1 radicular pain, most commonly due to L5-S1 paracentral disc herniation. It requires placing the needle through the posterior S1 foramen onto the pedicle of S1.
- Target visualisation
- AP view through L5-S1 disc space, with a cephalo-caudad tilt
- Slight ipsilateral oblique, superimposing the anterior and posterior S1 foramina.
- The target point lies on the caudal border of the S1 pedicle, just dorsal to the internal opening of the S1 anterior sacral foramen.
- Needle placement
- The needle insertion point is marked at the lateral margin of the posterior foramen.
- Advance the needle towards the dorsal surface of the sacrum at the lateral margin of the S1 posterior foramen
- When the needle hits the sacrum, it is readjusted in order to pass superiorly and slightly medially into the S1 posterior sacral foramen. The aim is to hit the middle of the caudal border of the anterior half of the S1 pedicle.
- The needle shouldn't go medial tot he middle of the caudal border of the pedicle.
- Injection
- Inject contrast under live fluoroscopy, using digital subtraction if available.
- Watch for intravascular or intrathecal flow. Intravascular uptake is more common here.
- After contrast inject local anaesthetic followed by steroid. 3mL will cover the L5-S1 disc 92% of the time.
Ultrasound Guided
A cadaver study found that ultrasound guided transforaminal injection was almost as accurate as fluoroscopic guidance.[18] The thoughts in New Zealand is that it is not ready for prime time. However many clinicians overseas use this approach.
A video of the technique can be found here.
- Place the curvilinear transducer midline in the axial plane. Identify the from lateral the medial the transverse processes, articular processes and the posterior complex centrally.
- Slide the transducer laterally with it facing in a medial direction , and also slide it caudally. Identify from lateral to medial the vertebral body, spinal nerve, lamina, and spinous process.
- Insert the needle from lateral to medial in plane aiming for the epidural space of the posterior aspect of the spinal nerve.
- Test injection of local anaesthetic, then inject corticosteroid.
Complications
The incidence of minor complications is between 2.4 and 9.6%. These include vascular penetration, non-positional headaches, back pain, worsening leg pain, facial flushing, intraoperative hypertension, transient nerve root irritation, and vasovagal reaction.[19]
Major complications are all extremely rare and include epidural abscess, epidural haematoma, and spinal cord infarction. The most catastrophic and extremely rare complication is spinal infarction from thrombosis of the artery of Adamkiewicz (i.e. arteria radicularis magnus or ARM) from injection of particulate steroids or direct trauma (laceration, dissection, or spasm) from needle placement. This artery supplies the spinal cord from T8 to the conus medularis. It most often enters the canal via the neural foramen T12 through L3 but the artery or a radiculomedullary feeder artery can be present at any level with a high degree of anatomic variation. In some individuals it can arise from the lower lumbar spine. The risk if injury is thought to be reduced by:
- Avoid advancing the needle to the ventral floor of the neural foramen for levels at or superior to L3.[16]
- Using non-particulate steroids
- Using continuous fluoroscopy during injection of contrast to identify intra-arterial flow
- Injecting a test dose of local anaesthetic prior to injection of corticosteroid to recognise neurological effects.
Some authors contend that this major complication is a black swan event not related to technique, and that the infraneural approach should be used as a matter of routine to minimise the risk.[2]
Aftercare
Assess the patient's pain at 15-30 minutes after the procedure. Consider fall risk if a test dose of anaesthetic was used and ensure they are able to mobilise safely. The patient should not drive or operate heavy machinery. Another responsible adult such as a family member should drive them home.
The majority of patients require only a single injection. One review found that of the patients who achieved ≥50% pain relief, 94% required one injection, and 4% required two injections to achieve this level of relief.[8]
One study found that 22.4% of patients had repeat injections within a year either in the hopes of achieving greater relief or for recovery of lost benefit. [12]Another study reported 42% having repeat injections within 6 months.[17]
In the event of an incomplete response at 2 weeks post-injection, one can consider a repeat injection.[17]
Postprocedure changes in sensation are expected, and even temporary motor function impairment. The response at two weeks is strongly associated with the two month outcomes. Immediate response is only weakly associated with two month outcomes.[20]
Videos
L4/5 Supraneural TFI:
Resources
See Also
External Links
References
- ↑ 1.0 1.1 1.2 Gregg, L., Sorte, D. E., & Gailloud, P. (2017). Intraforaminal Location of Thoracolumbar Radicular Arteries Providing an Anterior Radiculomedullary Artery Using Flat Panel Catheter Angiotomography. AJNR. American journal of neuroradiology, 38(5), 1054–1060. https://doi.org/10.3174/ajnr.A5104
- ↑ 2.0 2.1 2.2 Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: the 'unsafe' triangle. Pain Physician. 2010 May-Jun;13(3):237-44. PMID: 20495587.
- ↑ 3.0 3.1 Taterra D, Skinningsrud B, Pękala PA, Hsieh WC, Cirocchi R, Walocha JA, Tubbs RS, Tomaszewski KA, Henry BM. Artery of Adamkiewicz: a meta-analysis of anatomical characteristics. Neuroradiology. 2019 Aug;61(8):869-880. doi: 10.1007/s00234-019-02207-y. Epub 2019 Apr 27. PMID: 31030251; PMCID: PMC6620248.
- ↑ Rivera CE. Lumbar Epidural Steroid Injections. Phys Med Rehabil Clin N Am. 2018 Feb;29(1):73-92. doi: 10.1016/j.pmr.2017.08.007. PMID: 29173666.
- ↑ Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine (Phila Pa 1976). 1997 Jan 1;22(1):98-104. doi: 10.1097/00007632-199701010-00016. PMID: 9122790.
- ↑ 6.0 6.1 Bogduk N. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd Ed. San Francisco: ISIS; 2013
- ↑ Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010 Aug;11(8):1149-68. doi: 10.1111/j.1526-4637.2010.00908.x. PMID: 20704666.
- ↑ 8.0 8.1 MacVicar J, King W, Landers MH, Bogduk N. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013 Jan;14(1):14-28. doi: 10.1111/j.1526-4637.2012.01508.x. Epub 2012 Oct 30. PMID: 23110347.
- ↑ Delport EG, Cucuzzella AR, Marley JK, Pruitt CM, Fisher JR. Treatment of lumbar spinal stenosis with epidural steroid injections: a retrospective outcome study. Arch Phys Med Rehabil. 2004 Mar;85(3):479-84. doi: 10.1016/s0003-9993(03)00472-6. PMID: 15031837.
- ↑ Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. doi: 10.1056/NEJMoa1313265. Erratum in: N Engl J Med. 2014 Jul 24;371(4):390. PMID: 24988555.
- ↑ Goodman BS, House LM, Vallabhaneni S, Mallempati S, Willey MR, Smith MT. Anticoagulant and Antiplatelet Management for Spinal Procedures: A Prospective, Descriptive Study and Interpretation of Guidelines. Pain Med. 2017 Jul 1;18(7):1218-1224. doi: 10.1093/pm/pnw227. PMID: 28339551.
- ↑ 12.0 12.1 Kennedy DJ, Plastaras C, Casey E, Visco CJ, Rittenberg JD, Conrad B, Sigler J, Dreyfuss P. Comparative effectiveness of lumbar transforaminal epidural steroid injections with particulate versus nonparticulate corticosteroids for lumbar radicular pain due to intervertebral disc herniation: a prospective, randomized, double-blind trial. Pain Med. 2014 Apr;15(4):548-55. doi: 10.1111/pme.12325. Epub 2014 Jan 2. PMID: 24393129.
- ↑ Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, Miller HJ, Awad SS, Crosby CT, Mosier MC, Alsharif A, Berger DH. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. 2010 Jan 7;362(1):18-26. doi: 10.1056/NEJMoa0810988. PMID: 20054046.
- ↑ Furman MB, Mehta AR, Kim RE, Simon JI, Patel R, Lee TS, Reeves RS. Injectate volumes needed to reach specific landmarks in lumbar transforaminal epidural injections. PM R. 2010 Jul;2(7):625-35. doi: 10.1016/j.pmrj.2010.04.023. PMID: 20659718.
- ↑ Chun EH, Park HS. Effect of High-Volume Injectate in Lumbar Transforaminal Epidural Steroid Injections: A Randomized, Active Control Trial. Pain Physician. 2015 Nov;18(6):519-25. PMID: 26606003.
- ↑ 16.0 16.1 Furman. Lumbar Transforaminal Epidural Steroid Injection. Atlas of Image Guided Spinal Procedures. 2018
- ↑ 17.0 17.1 17.2 Murthy NS, Geske JR, Shelerud RA, Wald JT, Diehn FE, Thielen KR, Kaufmann TJ, Morris JM, Lehman VT, Amrami KK, Carter RE, Maus TP. The effectiveness of repeat lumbar transforaminal epidural steroid injections. Pain Med. 2014 Oct;15(10):1686-94. doi: 10.1111/pme.12497. Epub 2014 Jul 7. PMID: 25039323.
- ↑ Hashemi, Masoud et al. “Ultrasound-Guided Lumbar Transforaminal Epidural Injections; A Single Center Fluoroscopic Validation Study.” Bulletin of emergency and trauma vol. 7,3 (2019): 251-255. doi:10.29252/beat-070307
- ↑ Chang A, Ng AT. Complications Associated with Lumbar Transforaminal Epidural Steroid Injections. Curr Pain Headache Rep. 2020 Sep 29;24(11):67. doi: 10.1007/s11916-020-00900-9. PMID: 32990823.
- ↑ El-Yahchouchi C, Wald J, Brault J, Geske J, Hagen C, Murthy N, Kaufmann T, Thielen K, Morris J, Diehn F, Amrami K, Carter R, Shelerud R, Maus T. Lumbar transforaminal epidural steroid injections: does immediate post-procedure pain response predict longer term effectiveness? Pain Med. 2014 Jun;15(6):921-8. doi: 10.1111/pme.12347. Epub 2014 Jan 21. PMID: 24612150.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,
![The anterior segmental artery is most likely to sit in the anterior superior quadrant of the neural foramen (96% of the time). © 2017 by American Journal of Neuroradiology.[1]](/w/img_auth.php/thumb/8/89/Scatterplot_of_arteries_in_the_neural_foramen.jpg/369px-Scatterplot_of_arteries_in_the_neural_foramen.jpg)