Lumbar Zygapophysial Joint Pain
| |
| Lumbar Zygapophysial Joint Pain | |
|---|---|
| Epidemiology | Approximately 30% of all chronic low back pain |
| Clinical Features | No reliable clinical features. Can cause somatic referred pain into the lower limbs. |
| Tests | Controlled diagnostic medial branch blocks |
| DDX | Internal Disc Disruption, Sacroiliac Joint Pain |
| Validity | Well validated and accepted source of pain in secondary care. |
| Treatment | Radiofrequency neurotomy |
The lumbar zygapophyseal joints are a validated source of chronic low back pain.
Anatomy
The lumbar zygapophysial joints are true synovial joints. They have hyaline cartilage that overlies the subchondral bone, a synovial membrane, a fibrous joint capsule, and a joint space (1-2mL).
Histological studies have shown encapsulated and free nerve endings, and the presence of substance P and calcitonin gene-related peptide.
Pathology
The causative pathology of lumbar zygapophysial joint pain is unknown.[1] It is thought to occur through trauma and cumulative stress over a lifetime. Possible sources are the synovial villi, capsule, and meniscal or synovial entrapments. What is clear however is that degenerative changes as detected radiographically are not associated with low back pain.[2]
Excessive compression or torsion can lead to microfracture and capsular avulsion of the zygapophysial joints. These post-traumatic structural changes have been shown in laboratory studies and postmortem pathoanatomic studies, but not in any antemortem studies. There are no validated techniques of identifying pathology during life[3]
It can be illustrative to compare with the cervical zygapophysial joints. In the cervical spine the joints face upwards and backwards, and therefore equally share the compressive load with the discs. Injuries are most likely to occur from weight bearing, and degenerative changes occur at all levels, most commonly at C3/4. In the lumbar spine, the zygapophysial joints face posteriorly and laterally, and share little of the axial load. The joints resist axial rotation and anterior translation. Degenerative changes arise earlier, most commonly at L4/5.
History
The lumbar facet joints were first posited to be a source of low back pain in the early 20th century. It was only from the 1970s onwards where more detailed anatomical studies of the sensory supply were done. Research by Bogduk and Long in 1979, with subsequent refinements by Bogduk essentially set the stage for the modern understanding of the lumbar facet joints in chronic low back pain.
| Year | Authors | Finding |
|---|---|---|
| 1911 | Joel Goldthwait | First described the lumbar facets as a potential source of pain[4] |
| 1933 | Ralph Ghormely | Used the term “facet syndrome” to describe pain originating from the ZAJ. [5] |
| 1941 | Badgley et al | facet joint pain suggested to be the source of up to 80% of back pain.[6] |
| 1963 | Hirsch et al | Injected 11% hypertonic saline in the region of the facet joints and provoked low back and thigh pain[7] |
| 1971 | Rees | Described "Multiple bilateral percutaneous rhizolysis,"[8] However later shown by Bogduk that it was only a fasciotomy.[9] |
| 1971 | Shealy | Used radiofrequency neurotomy to treat ZAJ origin back pain. |
| 1976 | Moony & Robertson | Intra-articular injections of hypertonic saline followed by local anaesthetic. Described non-radicular referred pain. |
| 1979 | Bogduk & Long | Detailed anatomical study of the ZAJ innervation. Developed percutaneous lumbar medial branch neurotomy.[10][11][12][13] Bogduk continued to refine the technique in the subsequent decades. |
Epidemiology
On the whole, studies have reported prevalence rates of around 30%.[16] This compares to about 40% for disc pain, and 20% for sacroiliac joint pain.
In many studies, complete relief of pain was not a diagnostic criterion, but was usually 50% or 80%. As a diagnostic test, there is a balance between sensitivity and specificity depending on the cut off, with a higher relief of pain criterion resulting in a higher specificity but lower sensitivity.
The argument of using a cut-off lower than 100% is usually around the possibility of having more than one source of pain. King and Bogduk[3] reference two studies[17][18] to argue that patients with chronic low back pain only rarely have concurrent sources of pain, and so placebo responses can't be excluded. They note that if 100% relief of pain is used then the prevalence drops to about 5% or less.[19][20][21][22]
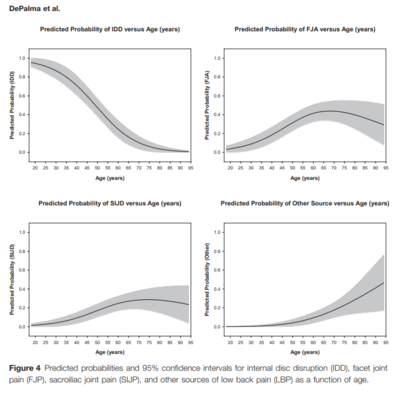
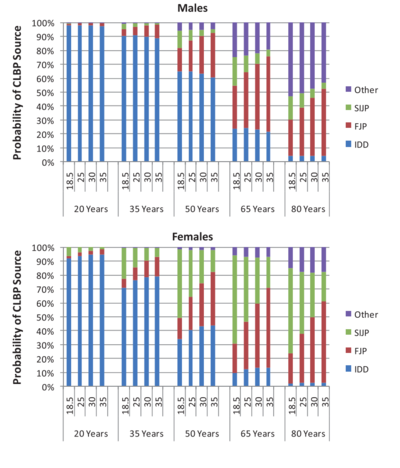
They continue however that the prevalence appears to be highly dependent on age. In a study of the elderly using a 90% criteron, 34% were positive.[23] A later study with two publications found that the prevalence was 2% in those 20-35, 5-10% in those 35-50, 20% in those 50-65, and 30-40% in those over 65. There was also an association with age and BMI.[24][25] (figures 2 and 3) It appears that in certain groups the prevalence is as high as internal disc disruption.
Importantly, there is no association with zygapophysial joint osteoarthritis.[3]
Clinical Features
No reliable clinical features or imaging findings that are diagnostic
ZJ pain can cause back pain with referral into the lower limb Some cases of chronic low back pain can be relieved by anaesthetisation of the lumbar ZJ
- Like IDD, no clinical features that distinguish lumbar ZJ pain from other causes
- Often unilateral, but can be bilateral
- In a study by Mooney and Robertson[26], which demonstrated pain referral patterns of 5 normal and 15 abnormal volunteers (chronic LBP +/- sciatica) by injecting hypertonic saline:
- 2 patients – pain crossed the midline
- 3 patients – pain encompassed entire leg and foot
- Increased stimulus (i.e volume) = increased pain and increased radiation distally
- Localization of pain in the low back, buttock, and leg is a non-specific finding
- In all subjects, pain abolished by lignocaine
Diagnosis
- See also: Lumbar Medial Branch Blocks
Lumbar zygapophysial joint pain cannot be diagnosed through standard clinical means, nor through plain films, CT, or MRI. It can only be diagnosed by controlled diagnostic blocks.
The diagnostic criteria utilising controlled comparative diagnostic local anaesthetic blocks of the medial branches is the gold standard for diagnosis. This method has been shown to be durable over time with repeated testing at 1 year and 2 years.[27] A single block is not recommended due to the high false positive rate.[28] See Causes and Sources of Chronic Low Back Pain for a full discussion.
There are no clinical features that can distinguish between those who respond to blocks and those who don't. In fact, the presence of pain with extension or pain with extension and rotation is not correlated with positive blocks, however its absence does. See for example Revel's criteria below.
| Criteria | Points | Present | |
|---|---|---|---|
| Age > 65 | 1 | ||
| Pain relieved by recumbency | 1 | ||
| Absence of aggravation by coughing | 1 | ||
| Absence of aggravation by forward flexion | 1 | ||
| Absence of aggravation by rising from flexion | 1 | ||
| Absence of aggravation by hyperextension | 1 | ||
| Absence of aggravation by extension-rotation | 1 | ||
| Probability | Negative (0) | ||
5 or more criteria has a positive likelihood ratio of 3.1 for positive medial branch blocks.[29] However a follow up study found high specificity (90%) but very low sensitivity (<17%)[30]
Of note intra-articular injections are not used for the purpose of diagnosis for the following reasons:[31]
- They do not have diagnostic specificity. One study showed that inflammatory cytokines produced in a degenerative facet joint can leak into the epidural space.[32]
- They have no prognostic specificity for predicting the outcome of radiofrequency neurotomy.
- They also don't have therapeutic utility, meaning that if it is positive there is no follow up treatment. On the other hand medial branch blocks do have therapeutic utility because if positive then radiofrequency neurotomy can be offered.
Treatment
Precision Treatment
- Main article: Lumbar Facet Joint Precision Treatment
Lumbar radiofrequency ablation has level 2 evidence but but patients must be selected by two positive medial branch blocks with >80% pain relief. Repeated therapeutic medial branch blocks also has level 2 evidence.
Intra-articular corticosteroid
Some practitioners use corticosteroid as a first line intervention for facet joint pain. A placebo-controlled RCT, enrolling patients with confirmed ZJ pain by way of dual medial branch blocks, showed that IA steroid did not provide any meaningful benefit above saline.[33]
Resources
See Also
- Causes and Sources of Chronic Low Back Pain
- Chronic Low Back Pain
- Internal Disc Disruption
- Sacroiliac Joint Pain
References
- ↑ Bogduk. Low back pain In: Clinical and Radiological Anatomy of the Lumbar Spine. 5th Edition. Elsevier 2012
- ↑ Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O'Donnell CJ, Hoffmann U, Cole R, Hunter DJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976). 2008 Nov 1;33(23):2560-5. doi: 10.1097/BRS.0b013e318184ef95. PMID: 18923337; PMCID: PMC3021980.
- ↑ 3.0 3.1 3.2 Wade King and Nikolai Bogduk. Chronic Low Back Pain In: Bonica's Management of Pain. 2018
- ↑ GOLDTHWAIT, JOEL E. (1911-03-16). "The Lumbo-Sacral Articulation; An Explanation of Many Cases of "Lumbago," "Sciatica" and Paraplegia". The Boston Medical and Surgical Journal. 164 (11): 365–372. doi:10.1056/NEJM191103161641101. ISSN 0096-6762.
- ↑ Ghormley RK. Low back pain with special reference to the articular facets, with presentation of an operative procedure. JAMA. 1933;101:773 doi: 10.1001/jama.1933.02740480005002
- ↑ Badgley CE. The articular facets in relation to low back pain and sciatic radiation. J Bone Joint Surg Am. 1941;23:481–496. Abstract
- ↑ Hirsch, Carl; Ingelmark, Bo-Eric; Miller, Malcolme (1963-01-01). "The Anatomical Basis for Low Back Pain: Studies on the presence of sensory nerve endings in ligamentous, capsular and intervertebral disc structures in the human lumbar spine". Acta Orthopaedica Scandinavica. 33 (1–4): 1–17. doi:10.3109/17453676308999829. ISSN 0001-6470.
- ↑ Rees WES. Multiple bilateral subcutaneous rhizolysis of segmental nerves in the treatment of the intervertebral disc syndrome. Ann General Practice. 1971;16:126–127.
- ↑ Bogduk, N.; Colman, R. R.; Winer, C. E. (1977-03-19). "An anatomical assessment of the "percutaneous rhizolysis" procedure". The Medical Journal of Australia. 1 (12): 397–399. doi:10.5694/j.1326-5377.1977.tb130762.x. ISSN 0025-729X. PMID 141591.
- ↑ Bogduk, Nikolai; Long, Don M. (1979-08-01). "The anatomy of the so-called "articular nerves" and their relationship to facet denervation in the treatment of low-back pain". Journal of Neurosurgery (in English). 51 (2): 172–177. doi:10.3171/jns.1979.51.2.0172.
- ↑ Bogduk, N.; Wilson, A. S.; Tynan, W. (1982-03). "The human lumbar dorsal rami". Journal of Anatomy. 134 (Pt 2): 383–397. ISSN 0021-8782. PMC 1167925. PMID 7076562. Check date values in:
|date=(help) - ↑ Bogduk, N. (1980-11-15). "Lumbar dorsal ramus syndrome". The Medical Journal of Australia. 2 (10): 537–541. doi:10.5694/j.1326-5377.1980.tb100759.x. ISSN 0025-729X. PMID 6450875.
- ↑ Bogduk, N.; Long, D. M. (1980-03). "Percutaneous lumbar medial branch neurotomy: a modification of facet denervation". Spine. 5 (2): 193–200. doi:10.1097/00007632-198003000-00015. ISSN 0362-2436. PMID 6446163. Check date values in:
|date=(help) - ↑ DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011 Feb;12(2):224-33. doi: 10.1111/j.1526-4637.2010.01045.x. Epub 2011 Jan 25. PMID: 21266006.
- ↑ DePalma et al.. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain medicine (Malden, Mass.) 2012. 13:498-506. PMID: 22390231. DOI.
- ↑ DePalma MJ. Diagnostic Nihilism Toward Low Back Pain: What Once Was Accepted, Should No Longer Be. Pain Med. 2015 Aug;16(8):1453-4. doi: 10.1111/pme.12850. Epub 2015 Jul 27. PMID: 26218010.
- ↑ Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The relative contributions of the disc and zygapophyseal joint in chronic low back pain. Spine (Phila Pa 1976). 1994 Apr 1;19(7):801-6. doi: 10.1097/00007632-199404000-00013. PMID: 8202798.
- ↑ Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995 Jan 1;20(1):31-7. doi: 10.1097/00007632-199501000-00007. PMID: 7709277.
- ↑ Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, Latulippe M. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991 Oct 3;325(14):1002-7. doi: 10.1056/NEJM199110033251405. PMID: 1832209.
- ↑ Jackson RP, Jacobs RR, Montesano PX. 1988 Volvo award in clinical sciences. Facet joint injection in low-back pain. A prospective statistical study. Spine (Phila Pa 1976). 1988 Sep;13(9):966-71. doi: 10.1097/00007632-198809000-00002. PMID: 2974632.
- ↑ Laslett M, Oberg B, Aprill CN, McDonald B. Zygapophysial joint blocks in chronic low back pain: a test of Revel's model as a screening test. BMC Musculoskelet Disord. 2004 Nov 16;5:43. doi: 10.1186/1471-2474-5-43. PMID: 15546487; PMCID: PMC534802.
- ↑ Laslett M, McDonald B, Aprill CN, Tropp H, Oberg B. Clinical predictors of screening lumbar zygapophyseal joint blocks: development of clinical prediction rules. Spine J. 2006 Jul-Aug;6(4):370-9. doi: 10.1016/j.spinee.2006.01.004. PMID: 16825041.
- ↑ Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995 Feb;54(2):100-6. doi: 10.1136/ard.54.2.100. PMID: 7702395; PMCID: PMC1005530.
- ↑ DePalma et al.. Multivariable analyses of the relationships between age, gender, and body mass index and the source of chronic low back pain. Pain medicine (Malden, Mass.) 2012. 13:498-506. PMID: 22390231. DOI.
- ↑ DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain Med. 2011 Feb;12(2):224-33. doi: 10.1111/j.1526-4637.2010.01045.x. Epub 2011 Jan 25. PMID: 21266006.
- ↑ Mooney V, Robertson J. The facet syndrome. Clin Orthop Relat Res. 1976;115:149–156.
- ↑ Pampati S, Cash KA, Manchikanti L. Accuracy of diagnostic lumbar facet joint nerve blocks: a 2-year follow-up of 152 patients diagnosed with controlled diagnostic blocks. Pain Physician. 2009 Sep-Oct;12(5):855-66. PMID: 19787011.
- ↑ Manchikanti L, Kosanovic R, Pampati V, Cash KA, Soin A, Kaye AD, Hirsch JA. Low Back Pain and Diagnostic Lumbar Facet Joint Nerve Blocks: Assessment of Prevalence, False-Positive Rates, and a Philosophical Paradigm Shift from an Acute to a Chronic Pain Model. Pain Physician. 2020 Sep;23(5):519-530. PMID: 32967394.
- ↑ Revel M, Poiraudeau S, Auleley GR, Payan C, Denke A, Nguyen M, Chevrot A, Fermanian J. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine (Phila Pa 1976). 1998 Sep 15;23(18):1972-6; discussion 1977. doi. PMID
- ↑ Laslett M, Oberg B, Aprill CN, McDonald B. Zygapophysial joint blocks in chronic low back pain: a test of Revel's model as a screening test. BMC Musculoskelet Disord. 2004 Nov 16;5:43. doi PMID
- ↑ Bogduk N. Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd Ed. San Francisco: ISIS; 2013
- ↑ Igarashi, Akira; Kikuchi, Shin-ichi; Konno, Shin-ichi (2007-03). "Correlation between inflammatory cytokines released from the lumbar facet joint tissue and symptoms in degenerative lumbar spinal disorders". Journal of Orthopaedic Science: Official Journal of the Japanese Orthopaedic Association. 12 (2): 154–160. doi:10.1007/s00776-006-1105-y. ISSN 0949-2658. PMID 17393271. Check date values in:
|date=(help) - ↑ Kennedy, David J; Fraiser, Ryan; Zheng, Patricia; Huynh, Lisa; Levin, Joshua; Smuck, Matthew; Schneider, Byron J (2018-12-12). "Intra-articular Steroids vs Saline for Lumbar Z-Joint Pain: A Prospective, Randomized, Double-Blind Placebo-Controlled Trial". Pain Medicine. 20 (2): 246–251. doi:10.1093/pm/pny225. ISSN 1526-2375.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


