Middle Cluneal Nerve Entrapment
The cluneal nerves are a group of pure sensory nerves (superior, medial or middle, and inferior) that provide sensory supply to the buttocks. This article covers middle cluneal nerve entrapment. See also the more common superior cluneal nerve entrapment, as well as inferior cluneal nerve entrapment.
Anatomy
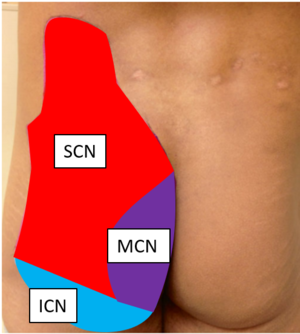
The cluneal nerves are divided into the superior cluneal nerve (SCN), middle cluneal nerve (MCN), and inferior cluneal nerve (ICN). The middle cluneal nerves are sensory nerves derived from the lateral branches of the dorsal rami of S1-S3. It has also been described as arising from the posterior sacral nerve plexus formed by S1-S3 dorsal rami. The nerves exit the sacral foramina and travel inferolaterally under the PSIS and across the long posterior sacroioliac ligament. The nerve route is variable, with the MCN travelling underneath the LPSP or superficial to it. The MCNs pierce the gluteus maximus and travel to the dorsal sacrum. The MCNs supplies sensory innervation overlying the intermediate medial gluteus maximus. There may be an anastamosis between the MCN and SCN.[2] The most superior branch of the MCN often anastamoses with the medial SCN distally, and this may explain why leg symptoms are common as the MCN comprises of the sensory branches of the dorsal rami of S1-S3.
See Konno et al for an open access anatomical study of middle cluneal nerve entrapment.[3]
Pathophysiology
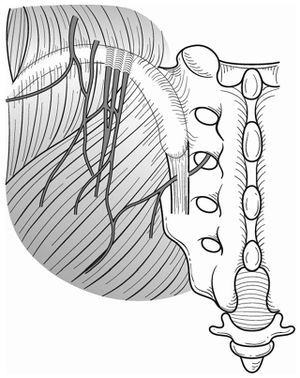
The MCN can become trapped while passing underneath or through the long posterior sacroiliac ligament (LPSL).[4]
Epidemiology
The epidemiology is largely unknown.
Clinical Features
The pain is aggravated by short and long periods of standing, lumbar flexion, rolling, prolonged sitting, and especially by walking. The clinical features are similar to other causes of low back pain, especially sacroiliac joint pain and sciatica.[5] The S1 to S2 composition could explain why most patients with MCN entrapment get leg symptoms.[4]
There should be maximal tenderness and a Tinel-like sign approximately 35mm caudal to the PSIS at a slightly lateral point at the edge of the iliac crest (corresponding to the area of nerve compression). An important diagnostic finding is the patient reporting numbness and radiating pain upon palpation over the compression zone.[5]
Imaging
The cluneal nerves are too thin to be visualised on MRI.
Diagnosis
Isu et al offer the following diagnostic criteria for MCN entrapment[5]:
- Low back pain involving the buttocks
- Symptoms exacerbated by lumbar movement or posture
- Trigger point 35 mm caudal to the posterior superior iliac spine at a slightly lateral point at the edge of the iliac crest (corresponding to the nerve compression zone)
- Patients report numbness and radiating pain in the MCN area (Tinel sign) when the trigger point is compressed
- Symptom relief by MCN block at the trigger point
Differential Diagnosis
Sacroiliac joint pain and sciatica are the two main differential diagnoses. A particular note must be made about the gold standard for sacroiliac joint pain diagnosis - sacroiliac joint block - other than the false positive rate. A positive sacroiliac joint block could still indicate long posterior sacroiliac ligament (LPSL) pain or MCN entrapment if there is dorsal extravasation of the local anaesthetic.[4] There are data to suggest that the LPSL is a significant pain generator in patients with sacroiliac joint pain. Murakami et al found that periarticular sacroiliac joint injection was more effective than intraarticular injection (100% vs 36%) in 50 patients with suspected sacroiliac joint or ligament pain.[6] Fortin et al looked at the patterns of contrast extravasation during 76 sacroiliac joint arthrograms, and found dorsal leakage around the LPSL in 24% and dorsal leakage into the S1 in 8%.[7]
Treatment
MCN injection can be done but there is limited information on its success rate. The injection is done around the LPSL.
See Matumoto et al for a well documented minor surgical MCN decompression technique.[8]
References
- ↑ Trescot, Andrea. Peripheral nerve entrapments : clinical diagnosis and management. Switzerland: Springer, 2016.
- ↑ Karri et al.. Pain Syndromes Secondary to Cluneal Nerve Entrapment. Current pain and headache reports 2020. 24:61. PMID: 32821979. DOI.
- ↑ Konno et al.. Anatomical study of middle cluneal nerve entrapment. Journal of pain research 2017. 10:1431-1435. PMID: 28652809. DOI. Full Text.
- ↑ 4.0 4.1 4.2 4.3 Aota. Entrapment of middle cluneal nerves as an unknown cause of low back pain. World journal of orthopedics 2016. 7:167-70. PMID: 27004164. DOI. Full Text.
- ↑ 5.0 5.1 5.2 Isu et al.. Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain. Neurospine 2018. 15:25-32. PMID: 29656623. DOI. Full Text.
- ↑ Murakami et al.. Effect of periarticular and intraarticular lidocaine injections for sacroiliac joint pain: prospective comparative study. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association 2007. 12:274-80. PMID: 17530380. DOI.
- ↑ Fortin et al.. Three pathways between the sacroiliac joint and neural structures. AJNR. American journal of neuroradiology 1999. 20:1429-34. PMID: 10512224. Full Text.
- ↑ Matsumoto et al.. Surgical treatment of middle cluneal nerve entrapment neuropathy: technical note. Journal of neurosurgery. Spine 2018. 29:208-213. PMID: 29775161. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


