Nerves of the Lumbar Spine
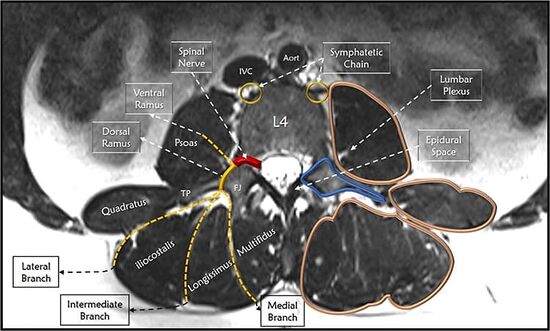
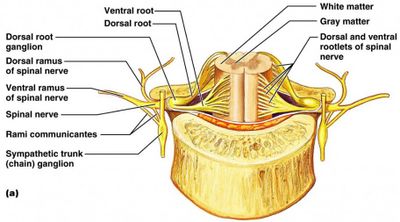
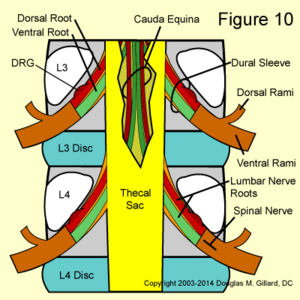
The lumbar spinal nerves lie in the intervertebral foraminae, and are connected by spinal nerve roots to the spinal cord. The spinal nerves divide into the ventral and dorsal rami outside the vertebral column. The lumbar sympathetic trunks run along the anterolateral lumbar vertebral column, and they communicate with the ventral rami of the lumbar spinal nerves
Lumbar Spinal Nerves
- The lumbar spinal nerves are numbered according to the vertebra beneath which they lie. The L1 spinal nerve lies below the L1 vertebra in the L1/2 intervertebral foramen. The L2 spinal nerve lies below the L2 vertebra in the L2/3 intervertebral foramen etc.
- Each spinal nerve is connected centrally to the spinal cord by a dorsal and ventral root.
- The joining of the spinal nerve roots to the spinal nerve occurs in the intervertebral foramen.
- The spinal nerve divides peripherally into a larger ventral ramus and smaller dorsal ramus.
- The branching into the two rami occurs outside the foramen.
- The spinal nerves are short, and no longer than the width of their intervertebral foramen.
- They are generally a few millimetres, but can be less than 1mm with the roots branching directly into rami without the formation of a proper spinal nerve.
Lumbar Nerve Roots
- The dorsal root transmits sensory fibres from the spinal nerve to the spinal cord
- The ventral root transmits mostly motor fibres from the spinal cord to the spinal nerve
- The ventral root may also transmit some sensory fibres
- The L1 and L2 ventral roots also transmit preganglionic, sympathetic, efferent fibres
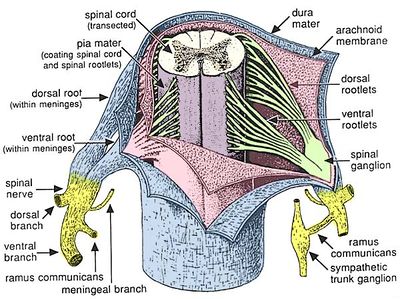
- The spinal cord has its termination opposite the L1/2 intervertebral disc, but the range is T12/L1 to L2/3.
- The lower lumbar and sacral nerve roots run within the vertebral canal largely enclosed in the dural sac.
- In the cauda equina, the lumbar, sacral, and coccygeal nerve roots run freely
- Each root is covered by individual pia mater, continuous with the pia mater of the spinal cord.
- The roots of the cauda equina are within the cerebrospinal fluid (CSF) which flows through the subarachnoid space
- The nerve fibres within the nerve roots run in a single trunk for most of their course
- Rootlets
- Near the spinal cord they separate into rootlets which are smaller bundles, and attach to the spinal cord.
- There are between 2-12 rootlets for each root, and are 0.5-1mm in diameter.
- The ventral root rootlets attach to the ventrolateral aspect of the spinal cord
- The dorsal root rootlets attach to the dorsolateral sulcus of the cord and along the ventral and dorsal surface of the cord the rootlets form an uninterrupted series of attachments
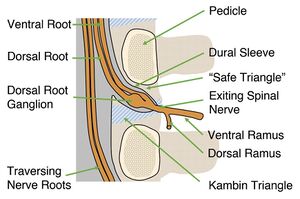
- Dural sleeve
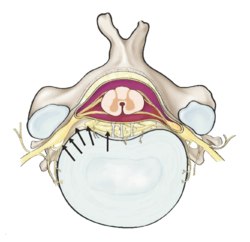
- A pair of spinal nerve roots leaves the dural sac just above the level of the intervertebral foramen
- The nerve roots penetrate the dural sac inferolaterally
- They take an extension of dura mater and arachnoid mater called the dural sleeve
- The dural sleeve encloses the nerve roots merges or becomes the epineurium of the spinal nerve
- The nerve roots are sheathed with pia mater and CSF flows around them as far as the spinal nerve
- Dorsal root ganglion
- The dorsal root ganglion is an enlargement of the dorsal root
- It is formed immediately proximal to the dorsal roots junction with the spinal nerve.
- It contains the cell bodies of the sensory fibres in the dorsal root
- It lies within the dural sleeve of the nerve roots and occupies the upper, medial part of the intervertebral foramen. It may lie further distally in the foramen with short spinal nerves. The location can be divided into intraspinal, neuroforaminal, and extraforaminal regions. From L1-L5 it is increasingly more likely that the DRG will be in the neuroforaminal region.[1]
- Nerve root angles leaving the dural sac
- The angles of each pair of nerve root as it leaves the dural sac varies, getting increasingly acute angles more caudally.
- The L1 nerve root leaves at about 80°, the L2 at about 70°, L3 and L4 at 60°, and L5 at 45°.
- Nerve root vertebral body origins
- The nerve root sleeves generally arise opposite the back of their respective vertebral bodies (L1 sleeve arises behind the L1 body, etc)
- However with successively caudal sleeves, they arise increasingly higher behind their vertebral bodies.
- And so the L5 nerve root arises behind the L4/5 intervertebral disc.
Relations of the Nerve Roots
- The nerve roots are intimately related to the meninges.
- The roots of the cauda equina are covered in the dural sac. Individual pairs of roots are covered by pia, arachnoid, and dura mater in the nerve root sleeves.
- Tumours or cysts of the dura or arachnoid can compress the nerve roots
- Radicular arteries and veins run within the root sleeves.
- Dural sac
- Anteriorly: floor of the vertebral canal, the vertebral bodies, discs, posterior longitudinal ligament, anterior spinal canal arteries and sinuvertebral nerves
- Posteriorly: roof of the vertebral canal, the laminae, and ligamenta flava
- Epidural space
- A space between the dural sac and the osseoligamentous boundaries of the vertebral canal
- Narrow space, almost a potential space.
- Filled by a thin layer of areolar connective tissue, some call the epidural membrane. This surrounds the dural sac.
- Relations
- Dorsally: lines the deep surface of the laminae and pedicles
- Ventrally: Lines the vertebral bodies, and passes medially deep to the posterior longitudinal ligament, and attaches to the anterior surface of the deep portion of the ligament. It doesn't cover the anulus fibrosis, but blends with the upper and lower borders of the AF just anterior to that of the posterior longitudinal ligament.
- Laterally: Opposite the intervertebral foramen, it goes laterally forming a circum-neural sheath around the dural sleeve of the nerve roots and spinal nerve
- The anterior and posterior internal vertebral venous plexuses run within the areolar tissue of the epidural membrane
- Epidural fat is concentrated around the nerve roots in the intervertebral foramina
- Radicular canals
- Individual pairs of nerve roots enclosed in their dural sleeves, course to the intervertebral foraminae along radicular canals
- The nerve roots are related laterally to a pedicle
- The pass the back of their vertebral body, run downwards, and enter the upper portion of their intervertebral foramen.
- Dorsally is a lamina and ligamenta flava, and these separate the root sleeve from the overlying facet joints.
- Dural ligaments (also known as meningovertebral ligaments or ligaments of Hofmann)
- The nerve root sleeves are tethered to the vertebral column by these ligaments, which are condensations of the epidural fascia
- The term dural ligament isn't anatomically correct. It is a connection between the meninges and the vertebral column
- Variably developed at L1-L4, well developed at L5
- Ventrally: passes from the ventral surface of the dura to the posterior longitudinal ligament
- Laterally: passes from the lateral surface of the dural sac to the periosteum of the pedicles and the capsule of the facet joint.
- Posteriorly: attached to the roof of the vertebral canal by occasional weak pseudo-ligamentous connections
- Nerve root sleeves are tethered within the vertebral canal and in the intervertebral foramen.
- Vertebral canal: the meningovertebral ligaments connect the dural to the posterior longitudinal ligament and the periosteum of the adjacent pedicle.
- Intervertebral foramen: the root sleeve is surrounded by the circum-neural sheath, indirectly binding the nerve roots and the spinal nerve mainly to the facet joint capsule dorsally, but also to the margins of the foramen. At the outer end of the foramen, there may be a transforaminal ligament - the spinal nerve is below most varieties of transforaminal ligaments but above the inferior type.
- Size of the spinal nerve and nerve roots
- The intervertebral foramen increases from L1/2 to L4/5.
- The L5/S1 foramen is smaller than the rest despite the L5 spinal nerve being the largest.
- The L5 spinal nerve occupies about 25-30% of the foramen while the other nerves occupy between 7-22%
- The L5 nerve is therefore the most susceptible to foraminal stenosis.
Anomalies of the Nerve Roots
The clinically most significant anomalies of the lumbar nerve roots are aberrant courses and anastomoses between nerve roots. See Trimba et al for a comprehensive review of the topic.[2]
Classification of conjoined nerve roots.[3]
| Type | General Anomaly | n-A | n-B |
|---|---|---|---|
| Type 1 | Aberrant courses | 1A: two pairs of nerve roots arise from a single dural sleeve | 1B: A dural sleeve arises from a low position on the dural sac |
| Type 2 | Variable nerve roots in an intervertebral foramen | 2A: A foramen is unoccupied by a nerve, with the foramen above or below containing two sets of roots | 2B: A foramen contains a supernumerary set of roots |
| Type 3 | Extradural anastomoses between roots in which a bundle of nerve fibres leaves one dural sleeve to enter an adjacent sleeve. May be superimposed on a type 2 | ||
- The incidence of anomalies is about 8.5%
- The anomalies do not always produce symptoms
- The doubled nerve roots occupy more of the available space in the radicular canal or intervertebral foramen than a single root
- Any space-occupying lesion is therefore more likely to compress a double nerve root, and symptoms will occur sooner than for a single nerve root compression.
- Disorders of the lumbar spine are not more common, but symptom development is more common in the presence of a space-occupying lesion.
- Clinical signs
- Clinical exam might reveal compression of a nerve root, but if that root has an anomalous course, then the lesion won't be at the expected location.
- In the case of a double nerve root, a single compressive lesion could cause signs that are suggestive of two lesions.
- Unusual clinical signs should lead to at least considering a nerve root anomaly.
- Intrathecal anastomoses are more common at 11-30%, but these occur proximal to the standard location of compression and so are not of diagnostic significance (but may be important in proximal nerve root surgery).
Dorsal Rami
- The L1-L4 dorsal ramiShort in length about 5mm
- Arise at almost right angles from the lumbar spinal nerves
- Directed backwards towards the upper border of the subjacent transverse process
- As they approach their transverse processes, they divide into two or three branches. A medial branch and lateral branch are consistently present. The intermediate branch will either arise from the dorsal ramus itself, or the be a branch off the lateral branch.
- L5 dorsal rami
- Longer and travels over the top of the ala of the sacrum.
- It forms only a medial branch and a branch that is equivalent to the intermediate branches of the other lumbar dorsal rami.
- Lateral branches
- Principally distributed to the iliocostalis lumborum muscle
- The L1-L3 lateral branches can emerge from the dorsolateral border of the iliocostalis lumborum and become cutaneous, piercing the thoracolumbar fascia and descending inferolaterally across the iliac crest to innervate the skin of the buttock over an area extending from the iliac crest to the greater trochanter. When crossing the iliac crest they run parallel to one another with those from lower levels lying most medially. See article on cluneal nerve pain.
- The lowest and most medial nerve that crosses the iliac crest does so approximately 7-8cm from the midline.
- Variability in which of the lateral branches become cutaneous
- In embryos and fetuses L1 is always cutaneous, L2 in 90%, L3 in 70%, and L4 in 40%.
- In adults it is similar except L4 cutaneous branches are uncommon. L1 exclusively in 60%. L1 and L2 in 27%. L1-L3 in 13%.
- Intermediate branches
- Only have a muscular distribution to the lumbar fibres of the longissimus muscle. They form an intersegmental plexus within this muscle.
- The L5 intermediate branch supplies the lowest fibres of longissimus which arise from the L5 transverse process and attach to the medial aspect of the iliac crest.
- Medial branches
- Distribution to the facet joints, and so are of clinical relevance
- L1-L4 medial branches of the dorsal rami
- Travel across the superior aspect of their respective transverse processes, and then pierce the dorsal leaf of the intertransverse ligament at the base of the transverse process.
- The nerve then runs along the bone at the junction of the root of the transverse process with the root of the superior articular process.
- Each nerve hooks medially around the base of the superior articular process, and is covered by the mamillo-accessory ligament.
- It then crosses the vertebral lamina, and divides into multiple branches that supply the multifidus muscle, the interspinous muscle and ligament, and two facet joints.
- Each medial branch supplies the zygapophysial joints above and below its course
- An ascending articular branch arises from the nerve just beyond the mamillo-accessory ligament where it starts to cross the lamina.
- A descending articular branch arises slightly more distally and travels downwards to the subjacent joint.
- L5 medial branch of the dorsal ramus
- Similar course to L1-L4, except instead it crosses the ala of the sacrum instead of a transverse process.
- It runs in the groove that is formed by the junction of the ala and the root of the superior articular process of the sacrum.
- It then hooks medially around the base of the lumbosacral facet joint.
- An articular branch supplies the lumbosacral facet joint, and it ramifies in multifidus.
- Muscular and interspinous ligament dorsal rami medial branches
- The muscles that move a particular segment are innervated by the nerve of that segment.
- L1 medial branch supplies only those fibres from the L1 vertebra, etc.
- The muscles arising from the spinous process and lamina of a lumbar vertebra, are innervated by the medial branch of the dorsal ramus immediately below that vertebra.
Histology
- Facet joint capsules
- Lumbar facet joint capsules are richly innervated with encapsulated, unencapsulated, and free nerve endings.
- Lumbar facet joint capsules transmit proprioceptive and nociceptive information
- Nerves containing neuropeptide Y is more common than substance P and calcitonin gene-related peptide.
- Facet joint subchondral bone
- Nerve fibres and nerve endings are also present in the subchondral bone of the facet joints
- The subchondral bone is another location for nociception.
- Intra-articular inclusions of the facet joints have nerve fibres that contain substance P - unclear if nociceptive or vasoregulatory.
- Interspinous ligaments
- Nerve fibres are plentiful
- The nerves give rise to Ruffini endings, pacini-form endings, and free nerve endings
- Ruffini endings are mechanoreceptors and are more numerous in the lateral surfaces.
- Pacini-form endings are associated with blood vessels and are uniformly distributed, the function is unclear.
- Free nerve endings are found near the attachment of the ligament to the spinous processes.
- Supraspinous ligaments and thoraco-lumbar fascia well well innervated and contain nerve fibres, Ruffini endings, and pacini-form endings.
- Ligamentum flavum is sparsely innervated.
Variations
- Occasionally, an articular branch arises from the dorsal ramus proper, and innervates the ventral aspect of the adjacent joint.
- One author found multiple articular branches from the spinal nerve, lateral branch of the dorsal ramus, and the entire length of the medial branch, but this hasn't been observed in other studies. Bogduk suspects the author mis-identified collagen fibres as nerves, as they weren't confirmed histologically.
Ventral Rami
- The ventral rami pierces the ventral leaf of the intertransverse ligament through the intervertebral foramen.
- They lie within the substance of the psoas major muscle in front of the ligaments
- They form plexuses within the muscle
- The L1-L4 ventral rami form the lumbar plexus
- The L4 and L5 ventral rami join to form the lumbosacral trunk
- The L5 ventral ramus crosses the ala of the sacrum, below the L5 transverse process. It can be trapped between these two bones which is called the "far out syndrome'
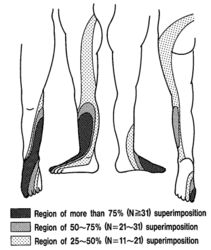
Dermatomes
- Main article: Dermatomes
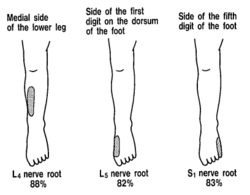
- Fluoroscopically guided local anaesthetic blocks has allowed a re-appraisal of the classical data on the cutaneous distribution of the lumbar spinal nerves.[4]
- The L4, L5, and S1 dermatomes vary between individuals with respect to their total extent, but exhibit a consistent concentric pattern between individuals.
- Each dermatome can extend from the posterior midline of the back, across the buttock, and into the lower limb.
- However, only a minority of individuals has such an extensive distribution for L4 and L5.
- Sensory deficit areas
- L4: most people have an area centred on the medial aspect of the lower leg
- L5: medial aspect of the foot, across the dorsum of the foot, and the lateral aspect of the lower leg
- S1: more extensive, a band from the posterior sacrum, along the entire length of the lower limb posteriorly, to the lateral aspect of the foot.
- The distal nature of each distribution indicates the area of skin supplied by branches of the ventral ramus of the particular spinal nerve.
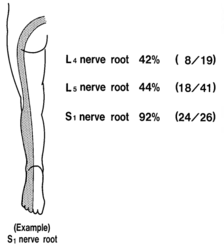
- Buttock distribution
- Buttock distribution indicates supply from the dorsal ramus.
- L4 dorsal ramus: 42% have a cutaneous distribution, L5 dorsal ramus: 44%, and S1 dorsal ramus: 92%.
- Nerve block data is inconsistent with anatomical data which acknowledges a S1 cutaneous distribution but not for L4 or L5. L5 might be from a communication with the dorsal sacral plexus. How the L4 dorsal ramus gets to the skin is a mystery.
Sympathetic Nerves
- The lumbar sympathetic trunks travel down along the anterolateral borders of the lumbar spine
- Each trunk is at the medial edge of the attachment of the psoas muscle
- Ganglia numbers vary from one to six, with four being most common.
- Branches
- Distributed to the abdominal and pelvic blood vessels and viscera, with some direct branches into the psoas muscle
- Principal branches are the rami communicantes to the lumbar ventral rami
- White rami communicantes: distributed to the L1 and L2 ventral rami
- Grey rami communicantes: distributed to every lumbar ventral ramus
- Number of rami communicantes to each lumbar nerve varies from one to three, and rarely even as much as five.
- Rami communicantes course: tunnels deep to the psoas, along the concave lateral aspects of the lumbar vertebral bodies, down to the lower borders of the transverse processes, and joins the ventral rami just outside the intervertebral foramina. They may also reach the ventral rami by passing through the substance of the psoas.
- Efferent fibres go to the blood vessels and skin in the territories supplied by the lumbar spinal nerves.
- They are involved in the formation of the lumbar sinuvertebral nerves, and the innervation of the lumbar intervertebral discs.
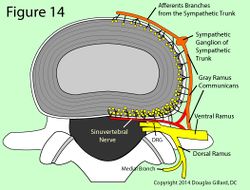
Sinuvertebral Nerves
Sinuvertebral nerves are formed from two roots: the ventral ramus and the gray ramus communicans. They provide provide the afferent pathways in lumbar discogenic pain.
- Sinuvertebral nerves are recurrent branches of the ventral rami, that re-enter the intervertebral foramina and are distributed within the vertebral canal.
- Each supplies the intervertebral disc at its level of entry into the vertebral canal, the disc above, and the intervening posterior longitudinal ligament.
- They are mixed nerves
- Somatic root from a ventral ramus
- Autonomic root form a grey ramus communicans
- They may be a series of filaments or a single trunk accompanied by additional fine filaments
- The nerves run along the posterior surface of the vertebral body just below the upper pedicle.
- An ascending branch forms within the vertebral canal, passing rostrally, parallel to the posterior longitudinal ligament (sending branches to it), and ends up in the superjacent interbertebral disc supplying it as well.
- A Shorter descending branch ramifies in the disc, and ligament at the level of entry of the originating nerve.
- Each nerve is also distributed to the blood vessels of the vertebral canal, and to the ventral aspect of the dura mater
- In the dura mater, each sinuvertebral nerve forms ascending and descending meningeal branches.
- The descending branches are longer, extending up to two segments caudally
- The ascending branch courses up to one segment.
- The dura mater is covered with a dense plexus of nerves on its ventral surface. It extends laterally but attenuates dorsally. The paramedian portion has no nerve fibres.
Innervation of the Lumbar Intervertebral Discs
- Lumbar disc innervation is a controversial issue
- Early studies did not show nerve fibres or nerve endings in the discs
- Other studies identified nerve fibres in the superficial layers of the anulus fibrosus (AF), and a variety of free and complex nerve endings in the outer third of the AF.
- Receptor distribution is not uniform in the disc.
- They are greatest laterally, and nearly all encapsulated receptors are here.
- A small number are posteriorly
- Least number anteriorly
Histology
- Development
- In the fetus nerves are abundant in the AF
- Postnatally - unencapsulated receptors arise, and in the adult there are five types of nerve endings.
- There is a relative decrease in the number of anterior region receptors
- Nerve endings resemble Golgi tendon organs, Ruffini endings, and paciniform endings in the outer lamellae of the AF.
- The endings contain CGRP, substance P, and vasoactive intestinal polypeptide. Substance P may have a vasoactive role.
- The anterior and posterior longitudinal ligaments also contain frequent nerve endings
Sources
- There are extensive microscopic plexuses of nerves that accompany the anterior and posterior longitudinal ligaments.
- The plexuses innervate around the entire circumference of the vertebral bodies and intervertebral discs.
- The anterior and posterior plexuses innervate the periosteum of the vertebral bodies through superficial branches, and the intervertebral disc and vertebral bodies through long penetrating branches. They follow blood vessels as far as the centre of the vertebral body.
- Direct branches of the ventral rami enter the posterolateral corner of the discs, and are one of several sources that contribute to the plexus that overlies the discs and vertebral bodies. The other sources are the grey rami communicantes, which send branches to the discs across their lateral surface and at their posterolateral corner.
- Somatic afferent fibres simply use the course of the rami communicantes to return to the ventral rami, rather than returning via the sympathetic trunk.
| Plexus | Formation | Relation |
|---|---|---|
| Anterior Plexus | Formed by branches of the sympathetic trunks, and branches from the proximal ends of the rami communicantes. Bridges the two lumbar sympathetic trunks | Covers the ALL. |
| Posterior Plexus | Formed from the sinuvertebral nerves | Accompanies the PLL |
| Lateral plexus | Formed by branches of the grey rami communicantes. | Connects the anterior and posterior plexuses |
- Endplate innervation
- There is additional nerve supply to the endplate, so both the AF and endplate are innervated.
- These nerves accompany the basivertebral veins and arteries, branching through the spongiosa.
- Endplate innervation is greater in painful discs
- The nerve endings contain substance P and CGRP, are often not related to blood vessels, and so they are sensory rather than vasomotor nerves.
- Intervertebral disc innervation role
- There are few blood vessels and so the nerves are unlikely vasomotor
- There is no evidence of a proprioceptive function, but cannot be excluded.
- The nerve endings are likely nociceptive.
Nerve Ingrowth
- Nerve fibres are only found in the outer third of the AF in normal discs, and do not occur deeper in the AF or NF
- In painful discs, nerve fibres are found in the deeper AF and into the NF. These are damaged rather than degenerated discs.
- In painful discs, the nerves accompany blood vessels that grow along annular fissures.
Summary
- Posteriorly: the branches of the lumbar dorsal rami innervate the back muscles and the facet joints
- Anteriorly: The ventral rami innervate the psoas major and quadratus lumborum
- Vertebral bodies and discs are surrounded by extensive plexuses that accompany the longitudinal ligaments, and are derived from the lumbar sympathetic trunks
- Within the posterior plexus, larger filaments constitute the sinuvertebral nerves
- Short branches innervate the vertebral periosteum, and long penetrating branches innervate deep into the vertebral body around its entire circumference
- The outer third of the AF has nerves from the longitudinal plexuses circumferentially.
- The posterior plexus innervates the dura mater and nerve root sleeves anteriorly and laterally.
Resources
See this brilliant visual tour of the lumbar nerve roots by a US physiotherapist.
References
These are study notes taken from Chapter 10 of:
- Bogduk, Nikolai. Clinical and radiological anatomy of the lumbar spine. Edinburgh: Elsevier/Churchill Livingstone, 2012.
- ↑ Silverstein, Michael P et al. “Lumbar dorsal root Ganglia location: an anatomic and MRI assessment.” International journal of spine surgery vol. 9 3. 12 Feb. 2015, doi:10.14444/2003
- ↑ Trimba et al.. Conjoined nerve roots of the lumbar spine. The spine journal : official journal of the North American Spine Society 2012. 12:515-24. PMID: 22749652. DOI.
- ↑ Morishita et al.. Intra-operative identification of conjoined lumbosacral nerve roots: a report of three cases. Journal of orthopaedic surgery (Hong Kong) 2012. 20:90-3. PMID: 22535819. DOI.
- ↑ Nitta et al.. Study on dermatomes by means of selective lumbar spinal nerve block. Spine 1993. 18:1782-6. PMID: 8235861. DOI.
![Classification of conjoined nerve roots.[3]](/w/img_auth.php/thumb/7/7d/Nerve_root_anomalies.png/600px-Nerve_root_anomalies.png)