Nociception
Pain is an unpleasant sensory and emotional experience. The physiology is complex and is located largely in the brain. In normal circumstances pain is elicited in the presence of actual or threatened tissue damage. The nervous system relays information to the brain about that tissue damage. However that information itself does not constitute pain, and is not pain until that information reaches the brain. Stimuli that elicits pain is commonly termed noxious. The information about tissue damage is referred to as nociceptive information. Most of what we know about pain relates to the physiology of nociception.
Transduction
Transduction means the detection of stimuli that might elicit pain. There are three basic mechanisms of transduction - chemical, mechanical, and thermal nociception. The function stems from the different ion channels and membrane receptors that convert the varying stimuli into action potentials through opening voltage-gated sodium channels.
The sensitivity of nociceptors is determined by the balance of excitatory and inhibitory influences through the action of neuropeptides on certain receptors. Substance P and CGRP sensitise part of the neurons, while opioid ligands and somatostatin inhibit the neurons.
Chemical Nociception
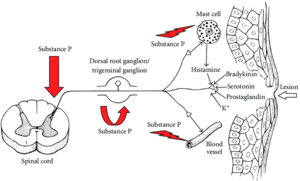
A free nerve ending is stimulated by chemicals, and action potentials are generated in that nerve. Various noxious chemicals are capable of triggering a nerve and eliciting pain such as bradykinin, histamine, serotonin, hydrogen ions, and potassium ions. These chemicals are released by cell damage as well as through inflammation.
Prostaglandins, derived from the action of cyclooxygenase on arachidonic acid, are also released by cell damage, but aren't able by in large to elicit nociceptive activity in nerve fibres. Prostaglandins facilitate the excitatory effect of the other chemicals and cause hyperalgesia. Leukotrienes, derived from lipoxygenase, are also synthesised and cause hyperalgesia which can be blocked by a reduction in polynuclear leucocytes.
Substance P is another chemical involved in the process of nociception. This chemical is located inside the terminals of peripheral nerve fibres. When the nerve fibre is stimulated by other chemicals, substance P is released into the extracellular space. In the periphery substance P is unable to directly stimulate these nerve fibres. It acts to promote vasodilation, which enhances inflammation, which thereby will secondarily increase the release of the above noxious chemicals and therefore secondarily enhance the stimulation of the nerve fibres. The primary function of substance P is to heal tissue damage and is part of the nocifensive system. The nocifensive system - a combination of nociception and defensive - being a process that protects the body from injury, i.e. looking at the vasodilation as a useful process.
| Source | Substance | Actions |
|---|---|---|
| Damaged cells | Potassium | Algesiogenic toward polymodal receptors |
| Histamine | Algesiogenic toward polymodal receptors | |
| Serotonin | Activation or sensitisation | |
| Bradykinin | Activation or sensitisation | |
| ATP | Activation or sensitisation | |
| Synthesised on site | Prostaglandin | Hyperalgesia and nociceptor sensitisation |
| Leukotriene | Hyperalgesia | |
| Nociceptors | Substance P | Vasodilation, oedema, enhanced release of histamine |
Thermal Nociception
The best known sensor molecule is transient receptor potential vanilloid 1 (TRPV1). It is one transducer of noxious heat and is the crucial ion channel for inflammatory thermal hyperalgesia.
This ligand-gated ion channel is only expressed on nociceptors, i.e. not other peripheral neurons. When this ion channel is opened, calcium flows into the cell and depolarises it. The human experiences painful heat or burning pain.
TRPV1 is opened with
- Temperatures higher than 43°C
- By chemicals such as capsaicin and ethanol
- By low pH (<5.9) such as in inflamed tissue
TRPV1 is activated by metabolites of arachidonic acid that are produced by the lipoxygenase pathway, for example 12-hydroperoxyeicosaenoic acid (12-HPETE), as well as by endocannabinoids.
TRPV1 is also sensitised by second messengers through inflammatory mediators: bradykinin, prostaglandin E2, extracellular adenosine triphosphate, glutamate, proteases, cytokines, and nerve growth factor.
There other TRP channels with different numbers at the ends of their names. Some of these other TRP channels are found on nociceptive neurons, but also on non-nociceptive neurons. For example TRPM8 is thought to be the primary transducer in non-nociceptive cold fibres, by opening with cold stimuli. The complete set haven't been fully studied.
Mechanical Nociception
The ionic basis for mechanonociception is not well understood. One theory is that it occurs when tissues that involve collagen are subjected to mechanical stress. Woven between collagen fibres are terminals of nociceptive nerve fibres. At rest the nerve fibres are able to pass through the weave of collagen easily. However when a tension is applied to the collagen, the spaces between the collagen fibres are constricted, and the nerve endings are compressed or stretched and are stimulated mechanically.
Peripheral Transmission
Copyright Michael D Mann
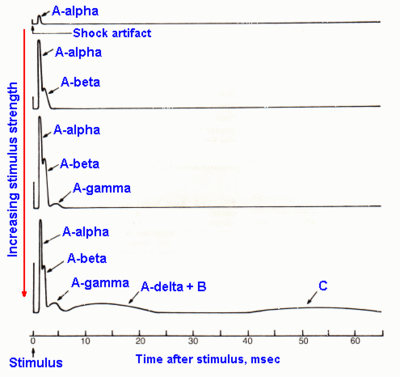
This includes events in peripheral nerve fibres once transduction has occurred. A response can be recorded from a peripheral nerve after a stimulus has been applied. The recording electrode experiences large changes in electrical potential. There are three major waves corresponding to three groups of nerves - A wave, B wave, and a smaller later C wave.
Velocities can be calculated through using the distances between the two electrodes. The diameters of myelinated (group A) nerve fibres are proportional to their conduction velocities, with a ratio of 6, i.e. the conduction velocity is equal to 6 times its diameter with appropriate adjustment of units.
The Aα and Aγ nerves are largely made up of motor neurons. The Aβ waves are produced by large diameter sensory nerve fibres that information related to proprioception, touch, and pressure. All fibres capable of transmitting nociception are Aδ fibres or C fibres.
There is no such thing as a "pain fibre" or specific nociceptive fibre. There are a variety of nerve fibres that are capable of transmitting nociception, but that may not be their only function. In various situations there may be more than one fibre involved in transmitting nociceptive information.
Nerves that transmit nociception have a threshold (called the noxious range) at which nociception occurs, and different nerves have different thresholds. For example there can be Aδ high threshold mechanoreceptors, and Aδ low threshold mechanoreceptors. Some mechanoreceptors are mixed in that they respond to both heat and mechanical information. Thermoreceptors respond to heat stimuli, but some do not have a linear increase in firing frequency in respond to increasing temperatures. C fibres are polymodal and can respond to chemical, thermal, or mechanical stimuli.
- Characteristics of peripheral nerve fibres
| Nerve Fibre | Myelin | Diameter (µm) | Conduction velocity (m/s) | General Function |
|---|---|---|---|---|
| Aα (I) | Yes | 13-20 | 80-120 | Proprioception: muscle spindle primary endings (Ia), golgi tendon organs (Ib), and alpha motor neurons |
| Aβ (II) | Yes | 6-12 | 35-75 | Discriminative sensitivity to mechanical stimuli (touch, vibration), proprioception, pain modulation (block nociceptive information, allodynia in sensitisation) |
| Aγ | Yes | 4-8 | 15-40 | Touch, pressure, and gamma motor neurons. |
| Aδ (III) | Thin | 1-5 | 5-30 | "rapid" pain, crude touch, pressure, temperature. AMH type I for rapid mechanical pain (high heat threshold >53C), AMH type II for rapid heat pain (lower heat threshold 43-47C). |
| B | No | 1-3 | 3-14 | preganglionic autonomic |
| C (IV) | No | 0.2-1.5 | 0.5-2.0 | "second" pain, mechanical, chemical, thermal, pruritis, and postganglionic autonomic. polymodal |
Central Transmission
Primary Afferents
Once information is detected by transduction, and passed along nerve fibres through transmission, it will reach the central nervous system. The dorsal roots transmit all manner of sensory fibres. They are sorted into large diameter afferents in the medial division of the dorsal root and small diameter afferents located in the lateral division.
Large diameter afferents aren't involved in nociception, but rather convey other information such as proprioception and touch, and pass up the posterior faniculus. They do however send collateral branches into the dorsal horn.
The small diameter afferent fibres contain those nerve fibres involved in nociception, along with fibres involved with temperature and visceral sensation. When they reach the spinal cord they don't go directly into the grey matter. They first send ascending and descending collateral branches that run longitudinally through the dorsolateral tract of the spine, also called the dorsolateral fasciculus of Lissaeur. Within several segments they leave the tract to synapse on neurons in the dorsal horn. In practical terms, nociceptive information reaching a segment is not restricted to that segment. A single nerve fibre conveying nociception can be distributed as far as 1-3 segments cephalad and 1-3 segments caudad.
The ventral roots also have a considerable number of small-diameter unmyelinated afferent fibres, however the majority of them end blindly, while the rest either loop within the ventral roots or branch into the dorsal root. The function of these ventral root afferents is unclear.
Dorsal Horn
The dorsal horn is the first site where there is integration and processing of incoming sensory information. Within the dorsal horn are neurons that pass upwards to more rostral regions of the central nervous system. They form the anterolateral funiculus (also known as the anterior and lateral spinothalamic tracts). The cell bodies of these neurons are mostly located within lamina V and lamina I of the dorsal horn. These second order neurons have connections higher up in the nervous system, and wait to receive information from the peripheral first order neurons.
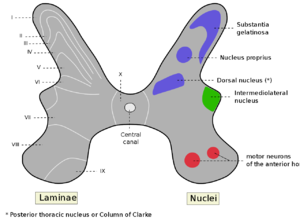
Laminae
Historically the dorsal horn has been divided into the marginal zone, substantia gelatinosa, and the nucleus proprius. It was subsequently divided into six laminae, with the most dorsal lamina being lamina I. There are functional differences in dorsal horn neurons in different laminae, along with different patterns of projections, and different chemical profiles. Large fibres (Aα and Aβ) enter in the medial division, and small fibres (Aδ and C) enter in the lateral division of the dorsal root.
Lamina I is also called the marginal zone. There are marginal neurons which are nociceptive-specific neurons, as well as wide dynamic range neurons (also in laminae V-VI) that respond to nociceptive and mechanoreceptive input. Interneurons are also found here which can inhibit first order Aδ neurons (pre-synaptic inhibition) and/or second order marginal neurons (post-synaptic inhibition).
Lamina II is also called the substantia gelatinosa, and the predominant cell types are wide dynamic range. There are glomeruli which are complex structures through which a primary afferent terminal can make synaptic contact with several peripheral dendrites, axonal terminals, and cell bodies. They allow both presynaptic and postsynaptic modulation of the primary afferent input. The peripheral terminals have inhibitory synapses, while the central terminals have excitatory synapses. The neurons can excite the marginal neurons of lamina I, as well as the dentrites of wide dynamic range neurons of lamina V. Therefore these neurons can modulate the influence of incoming peripheral nerve fibres.
Lamina III is similar to lamina II, but the cells are slightly larger, and there are myelinated axons. The predominant cell type is low-threshold mechanoreceptive.
Lamina IV has prominent large cells.
Lamina V has longitudinally oriented myelinated axons. The nucleus proprius is comprised of Lamine III, IV, and the upper part of Lamina V. Wide dynamic range neurons in lamina V can respond to non-noxious mechanical stimulation via collateral branches from large diameter afferents, as well as respond to noxious information from C fibres via interneurons. Inhibitory neurons activity determines what input will predominate.
Lamina VI is only present in the cervical and lumbosacral enlargements. It is a transitional zone between the primary afferent-dominated dorsal horn and the ventral horn. It has descending input that predominates.
Terminations of afferent fibres in the dorsal horn
There is a web of connections between the incoming afferent fibres and the dorsal horn neurons with a pattern of excitatory and inhibitory inputs. In normal situations there is a degree of segregation in the termination pattern for different types of afferent fibres in the dorsal horn. However in pathological situations this can change, for example in peripheral nerve injury there can be sprouting of myelinated afferents into lamina II resulting in functional contacts of low-threshold mechanoreceptive afferents with cells that normally only have C-fibre input
| Afferents | Terminal zones in dorsal horn |
|---|---|
| Large diameter myelinated fibres | III, IV, V |
| Small diameter myelinated fibres (Aδ) | I, V |
| Unmyelinated fibres (C) | II, III |
| Visceral projections | II, IV-V, X |
Dorsal horn neuron types
There are three major classes of dorsal horn neurons, the first two being involved in nociception and are called projection neurons.
- Nociceptive-specific (NS). These cells are only excited by high-threshold noxious or near-noxious levels of peripheral stimulation.
- Wide dynamic range (WDR) or convergent cells. The firing rate of the cells is increased by innocuous events, but further increased when stimulus intensity is raised to noxious levels.
- Low-threshold mechanosensitive (LTM). These cells are only excited by low-threshold innocuous stimuli. This includes hair movement, touching, or brushing the skin
Intracellular Physiology of Second Order Neurons
On the surface of the neuron are various receptors. There are a series of facilitations between receptors.
There are NMDA receptors and AMPA receptors which are triggered by aspartate and glutamate. With glutamate release by a primary afferent, the first effect is AMPA activation, resulting in an action potential in the second order neuron, but it is a brief stimulus. A second effect of AMPA triggering, is that the action potential acts on the calcium channel that is controlled by the NMDA receptor. At rest, the NMDA channel is blocked by magnesium. However upon arrival of an action potential generated by an AMPA receptor, that block is released, and calcium is allowed to enter through the channel and into the second order neuron. Therefore the AMPA role is to unlock the calcium channel controlled by the NMDA receptor.
Glutamate can act on the NMDA receptor producing an action potential. This action potential is stronger and longer lasting than that of the AMPA receptor, and is probably the main effect in nociceptive transmission.
Neurokinin 1 (NK1) receptors are stimulated by Substance P released from the central terminals of nociceptive nerve fibres. Substance P acting on NK1 receptors also allows influx of calcium through NMDA through protein kinase C by removing the blocking magnesium. This produces a long lasting depolarisation of the membrane, but it has a late onset. NK1 receptor antagonists were shown to not have a therapeutic effect in clinical trials.
Glutamate acting on a G protein, can trigger an enzyme within the cytoplasm called PLC. This results in the conversing of PIP to produce IP3 and DAG. DAG triggers PKC which acts on the NMDA receptor calcium channel, and enhances the influx of calcium. G protein function therefore enhances the operation of the NMDA receptor.
cfos is produced through release of calcium from the endoplasmic reticulum or through influx of calcium from outside the cell. cfos production is a signal that the cell is active, but it isn't necessarily so that the production of cfos leads to destructive effects or chronic pain.
Overall, there is a cascade of increasing hierarchy and graded pattern of possible responses from AMPA, to NMDA, to G protein and NK1 receptors. The more serious the peripheral stimulus, the more prolonged the effect on these various receptors, which progressively add up to produce a serious and sustained discharge in the second order neuron. Without a sustained effect from the periphery, the second order neuron will respond only briefly.
Spinal Cord Transmission Pathways
Ascending Pathways Involved in Nociception
The axons of the second order nociceptive specific and wide dynamic range neurons cross the spinal cord, pass upwards through the anterolateral funiculus, and into different regions of the somatosensory thalamus where it establishes contact with third order neurons. The second order neuron also makes synaptic contacts in different regions of the brainstem, such as the periaqueductal gray matter (PAG) and the nucleus raphe magnus (NRM). The third order neuron then transmits nociceptive information to different areas of the somatosensory cortex and limbic structures. At each synpatic contact, there is integration of information with inhibitory or excitatory influences.
Somatosensory signals are transmitted along two major ascending tracts in the spinal cord. These are the anterolateral system and the dorsal column-medial lemniscal system. The dorsal column-medial lemniscal system transmits tactile and proprioception information. The anterolateral system transmits pain and temperature predominantly, but also some tactile information. The anterolateral system has three pathways, the spinothalamic tract, the spinoreticular tract, and the spinomesencephalic tract. The main pathways for nociceptive afferents are the lateral spinothalamic tract and spinoreticular tract (or medial spinothalamic tract).
The lateral spinothalamic tract ascends directly towards the contralateral lateral thalamic nuclei of the ventrobasal complex. The projections in the ventrobasal complex is also called the "neospinothalamic" tract. The receptive field is limited to one side of the body, and the second order neurons come mainly from laminae I and IV-VI. This tract has rapid afferents with relatively precise receptive fields and is therefore involved in the localisation and perception of the sensory-discriminative component of pain - i.e. "where is it coming from."
The spinoreticular tract is more medial and ascends to the medial complex of the thalamus. It is also called the "paleospinothalamic tract". Most afferents arise from laminae VII and VIII. They project towards the medial nuclei of the thalamus, the periaqueductal gray matter (PAG), and the nucleus raphe magnus (NRM). This tract has fibres with larger receptive fields, the majority coming from C fibres. The projections lead towards regions of the brainstem, thalamus, and cortex that play a role in memory and emotions. Therefore this pathway is involved in the motivational-affective aspect of pain - i.e "what does it feel like."
The thalamus integrates nociceptive information and plays a role in pain modulation. The thalamic nuclei that receive afferents from the nociceptive tracts are divided into two groups: the nuclei of the ventrobasal complex (VPL, VPM), and the nuclei of the centromedian (CM) or intralaminar complex.
The ventrobasal complex mainly receives afferents from the spinothalamic tract, and then sends projections to the primary and secondary somatosensory cortex, facilitating the sensory-discriminative component of pain.
The CM (and central lateral?) nuclei mainly receive afferents from the spinoreticular tract and projects towards various limbic structures. The motivational-affective component of pain arises from connections to both the limbic system and frontal lobe.
Through the medulla, the upward travelling axons send collaterals to various nuclei in the reticular formation of the brainstem, in particular the nucleus reticularis gigantocellularis (NRGC). This initiates a rostrad pathway that reinforces the affective components of the pain experience.
There are four distinct steps in nociceptive stimuli: transduction, transmission, modulation, and perception. Transduction refers to the transformation of mechanical, thermal, or electrical stimuli into electrochemical energy in the specialised nerve endings. Transmission refers to the transmission of nerve impulses from the peripheral to the spinal cord, from the spinal cord to the brainstem and thalamus, and from the thalamus to the cortex. Modulation refers to different adjustments made by neurons responsible for transmission. Perception is the result of a nociceptive stimulus travelling through the entire central nervous system. See basic neurophysiology.
Descending Modulatory Pathways
Following painful stimulation, in addition to nociceptive information being transmitted to the higher centres via the spinothalamic tract, afferent collateral signals are also sent to various centres of the brainstem, including the periaqueductal grey matter (PAG) and nucleus raphe magnus (NRM). These centres send inhibitory efferent messages to various spinal segments and cause diffuse inhibition. This is called the diffuse noxious inhibitory control (DNIC), although later research has shown that input from the PAG isn't required, and the mechanism utilises structures of the midbrain.
The PAG relays down the NRM, and the NRM has axons that travel down the dorsolateral funiculus to the spinal cord. The NRM are also joined by other neurons located in the lateral medullary reticular formation (LMRF) and the locus coeruleus (LC), and these also caudally in the dorsolateral funiculus exerting influences in the spinal cord. These descending pathways are considered to be modulatory pathways of nociception, and the dorsolateral funiculus is the principal efferent tract of the descending inhibitory system. Injury to the dorsolateral funiculus causes hyperalgesia.
Axons that descend from the brainstem (e.g. from the NRM and LMRF) relay to various sites in the dorsal horn, and are able to exert excitatory and inhibitory effects. Descending pathways are able to control the throughput of nociceptive information in the dorsal horn. The descending pathways can act directly to inhibit marginal neurons, or they can excite inhibitory neurons. Of the various inhibitory neurons, some use enkephalin and others use GABA.
Centre-surround Inhibition
There is a constant background of activity from all ascending axons in the central nervous system such that the thalamus hears a lot of noise. When an axon is stimulated with nociceptive information it reaches the thalamus, a peak of activity is recorded, but this can be hard to discriminate from the background noise. With activation of the NRM, information is sent down to the spinal cord to inhibit spinal cord neurons, resulting in a suppression of background activity. There is inhibition of all the segments adjacent to the one that is transmitting nociceptive information. i.e. it doesn't inhibit the incoming pathway, only the surrounding pathways. The activity recorded in the thalamus but the nociceptive input remains the same, but the adjacent activity is suppressed, and so the nociceptive information is highlighted. In other words, pain is not only triggered by excitatory processes, but also by the perception of a contrast between the excitatory and inhibitory processes.
Neurogenic Pain
Pain can arise through another mechanism not involving damage to peripheral tissues, but rather when neurons are disordered. Neurogenic pain means pain arising from nerves, not peripheral tissues. Neurogenic pain does not involve transduction because peripheral nerve endings are not being stimulated.
Neuromas
One type of neurogenic pain is produced by a neuroma. Neuromas occur when a peripheral nerve is cut. Axon sprouts form from the proximal cuff, forming a neuroma. These are exquisitely sensitive to mechanical stimuli, and are also chemically sensitive to noradrenaline. Triggering of the neuroma generates an action potential, without any activity from the distal denervated end of the nerve. The patient is not able to tell whether the pain is arising from the periphery or from the neuroma.
Dorsal Root Ganglion
Pain from the dorsal root ganglion is radicular pain because of its location on a dorsal root. Ganglion cells can be affected by infection, inflammation, compression, or ischaemia. For example as a result of a disc herniation. Activity starts in the dorsal root ganglion cells, passed into the spinal cords, and processed in the same way as conventional nociceptive information.
Central Pain
The mechanisms here are located exclusively within the central nervous system. Under normal conditions a primary afferent sends action potentials to a second order neuron. Receptors on a second order neuron responds from neurotransmitters released from the first order neuron and an action potential is generated in the second order neuron.
In the event of deafferentation to the first order neuron. It doesn't transmit action potentials or release neurotransmitters onto the second order neuron. However the second order neuron, in the absence of incoming activity, change their characteristics. They become unstable, lose their receptors, leak sodium, and become spontaneously active. The spontaneous active generates action potentials which is perceived as noxious from the brain, in the absence of noxious activity. This is called deafferentation pain.
Resources
References
- Hubert van Griensven. Pain a textbook for health professionals. Second edition.
- ↑ Serge Marchand. The Phenomenon of Pain. IASP. 2012