Os Peroneum and Os Peroneum Syndrome: Difference between revisions
| (7 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{Partial}} | {{Partial}} | ||
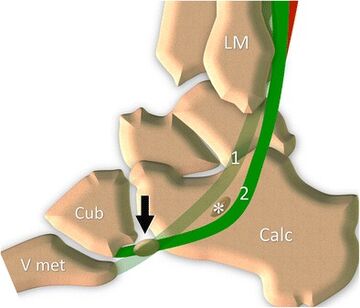
[[File:Os peroneum normal.jpg|thumb|360x360px|'''Os peroneum (OP) normal anatomy'''. Peroneal tendons (peroneus brevis 1, peroneus longus 2) travel along the lateral surface of the calcaneus that presents a small bony prominence, the peroneal tubercle (''asterisk''). The OP can be found inside the tendon at the level of the calcaneocuboid joint (''black arrow''). ''LM'' lateral malleolus, ''Calc'' calcaneus, ''Cub'' cuboid, ''V met'' fifth metacarpal bone.<ref name=":1">Bianchi S, Bortolotto C, Draghi F. Os peroneum imaging: normal appearance and pathological findings. Insights Imaging. 2017 Feb;8(1):59-68. doi: 10.1007/s13244-016-0540-3. Epub 2017 Jan 5. PMID: 28058662; PMCID: PMC5265202.</ref>]] | |||
The '''os peroneum''' is found within the peroneus longus in 26% of feet,<ref>Peterson JJ, Bancroft LW. Os peroneal fracture with associated peroneus longus tendinopathy. AJR Am J Roentgenol. 2001 Jul;177(1):257-8. doi: 10.2214/ajr.177.1.1770257a. PMID: 11418450.</ref> usually located plantar to the cuboid, lateral to the calcaneus, or at the [[Transverse Tarsal Joint (Chopart's Joint)|calcaneocuboid joint]].<ref name=":0">Sobel M, Pavlov H, Geppert MJ, Thompson FM, DiCarlo EF, Davis WH. Painful os peroneum syndrome: a spectrum of conditions responsible for plantar lateral foot pain. Foot Ankle Int. 1994 Mar;15(3):112-24. doi: 10.1177/107110079401500306. PMID: 7951939.</ref>It is a factor in the development of '''os peroneum syndrome'''.<ref>Clarke HD, Kitaoka HB, Ehman RL. Peroneal tendon injuries. Foot Ankle Int. 1998 May;19(5):280-8. doi: 10.1177/107110079801900503. PMID: 9622417.</ref> | |||
The | == Anatomy == | ||
{{Article derivation|article-link=https://pubmed.ncbi.nlm.nih.gov/28058662/|article=Os peroneum imaging: normal appearance and pathological findings|author=Stefano Bianchi, Chandra Bortolotto, Ferdinando Draghi|license-link=https://creativecommons.org/licenses/by/4.0/|license=CC-BY}} | |||
The peroneal tendon (PT) complex is made up of the muscles and tendons of the peroneus longus tendon (PLT) and peroneus brevis tendon (PBT), their common synovial sheath, the superior and inferior retinaculum, and the Os peroneum (OP). | |||
The peroneal longus (PLM) and brevis (PBM) muscles are located inside the external compartment of the leg, lateral to the fibula. The PLM originates from the proximal portion of the lateral surface of the fibula and from the nearby intermuscular septum. The PBM originates from the distal third of the lateral surface of the fibula and from the nearby intermuscular septum. At the level of the leg’s median third, the PLM extends through a superficial, flat aponeurosis that covers the PBM. The PBM presents a myoaponeurotic junction distally located with regard to that of the PLM. Both muscles are innervated by the peroneal superficial nerve. The peroneal muscles are supplied by two principal source arteries, the anterior tibial artery and the peroneal artery. | |||
At the malleolar region, the two tendons reflect against the posterior aspect of the lateral malleolus. At this level they run inside an osteofibrous tunnel (proximal tunnel) made up of the concave bony gutter and the thick fibrous superior retinaculum. This inserts into the lateral surface of the malleolus and guarantees the stability of the tendons during ankle movement, thus preventing their anterior luxation during movement of the ankle. | |||
Distal to the lateral malleolus, the PT travel along the lateral surface of the calcaneus, which presents a small bony prominence, the peroneal tubercle (PTub). The peroneus brevis tendon (PBT) runs superiorly while the PLT runs inferiorly to it. At this level, the two tendons run inside another osteofibrous tunnel (distal tunnel), stabilized against the calcaneus thanks to the inferior retinaculum, which inserts on the apex of the PTub. The tubercle acts as a pulley for the PLT that reflects on its inferior surface. | |||
Distal to the PTub, the PBT travels straight forward, to insert into the base of the fifth metatarsal bone. | |||
The PLT, after reflecting against the cuboid, reaches the plantar region and attaches to the first and second metatarsal bones. | |||
The two PT are enclosed by a common synovial sheath allowing optimal sliding of the tendons during movements of the ankle and/or contraction of the peroneal muscles. The sheath is made of a parietal layer adherent to the paratendinous soft tissue and a visceral layer adherent to the tendons. Proximal to the PTub the sheath divides to individually surround the two tendons. In some cases, the sheath surrounding the PLT is longer and extends from the cuboid tunnel to the plantar aspect of the foot. In physiologic conditions, it contains only a small amount of synovial fluid. | |||
The OP is a small sesamoid bone which can be found inside the PLT at the level of the calcaneocuboid joint. The OP is ossified in around 20% of the population, and it is bilateral in around 60% of cases. This small sesamoid bone can show different sizes and can also be bipartite or multipartite. A recent cadaveric study described the normal shape and size of the OP on 36 cadavers. The ossicle presented a flattened oval shape, with one or two concave articular deep surfaces. The average thickness was 4 mm and length 13 mm. A bipartite bone is common and can be seen in around 30% of cases. | |||
The presence of an OP or a bipartite OP can be clinically significant. The differential diagnosis between the ossicle and a cortical avulsion or a soft tissue calcification can be difficult in patients with pain in the lateral side of the foot. Similarly, a multipartite bone must be differentiated from a fractured one. | |||
The origin of OP development is controversial. Some authors advocate an embryonic development of the ossicle, while others believe that the OP develops from a “stress response”. A recent cadaveric study from Guimera and colleagues demonstrates that a precursor of the OP is already present during the foetal period. Mittal et al. propose that development of the OP follows local stresses to the tendon, leading to its thickening and secondary ossification. | |||
== Pathophysiology == | == Pathophysiology == | ||
Os peroneum syndrome, also referred to as painful Os peroneum syndrome is a spectrum of conditions associated with an Os peroneum in the lateral foot. It can include the following:<ref>Weerakkody, Y., Luong, D. Os peroneum syndrome. Reference article, Radiopaedia.org. (accessed on 07 Mar 2022) <nowiki>https://doi.org/10.53347/rID-76408</nowiki></ref> | |||
* acute os peroneum '''fracture or diastasis''' of a multipartite os peroneum | |||
* chronic (healing or healed) os peroneum fracture or diastasis of a multipartite os peroneum with callus formation which can result in '''peroneus longus stenosing tenosynovitis'''. | |||
* attrition or '''partial rupture of the peroneus longus tendon''', proximal or distal to the os peroneum | |||
* '''frank rupture of the peroneus longus tendon''' with discontinuity proximal or distal to the os peroneum | |||
* presence of a '''large peroneal tubercle''' on the lateral aspect of the calcaneus which '''entraps the peroneus longus tendon''' and/or the os peroneum during tendon excursion leading to '''peroneus longus stenosing tenosynovitis.''' | |||
== Classification == | |||
Tears are classified as follows<ref name=":1" /> | |||
# Type 1: proximal to the Os peroneum | |||
# Type 2: at the Os peroneum | |||
# Type 3: distal to the Os peroneum | |||
== Clinical Features == | == Clinical Features == | ||
| Line 13: | Line 48: | ||
== Investigations == | == Investigations == | ||
Standard plain films show the Os peroneum (AP, lateral, mortise of the ankle, and AP and oblique of the foot). Also look for fracture, diastasis of multipartite Os peroneum, callus formation, proximal migration of the Os peroneum.<ref name=":0" /> | Standard plain films show the Os peroneum (AP, lateral, mortise of the ankle, and AP and oblique of the foot). Also look for fracture, diastasis of multipartite Os peroneum, callus formation, proximal migration of the Os peroneum.<ref name=":0" /> | ||
Take care in not mistaking it for:<ref>Gaillard, F., Baba, Y. Os peroneum. Reference article, Radiopaedia.org. (accessed on 07 Mar 2022) <nowiki>https://doi.org/10.53347/rID-7648</nowiki></ref> | |||
* os vesalianum pedis | |||
* os cuboideum secundarium | |||
* apophysis of the 5th metatarsal | |||
* avulsion fracture (pseudo-Jones fracture) | |||
Ultrasound can also be useful however only the outer surface of the Os peroneum can be assessed (but it can see displacement). It can however assess the tendons such as for tears and tenosynovitis.<ref name=":1" /> | |||
On MRI the Os peroneum can present as a "pseudo-tear" due to its intermediate signal by inexperienced radiologists. It can be very helpful but needs a proper sequence and field of view selection.<ref name=":1" /> | |||
== Treatment == | == Treatment == | ||
| Line 18: | Line 63: | ||
In severe cases immobilisation of the limb may be required. | In severe cases immobilisation of the limb may be required. | ||
[[Peroneal Tendon Sheath Injection|Peroneal tendon sheath injection]] is an option in tenosynovitis. | |||
The patient should also have a graded exercise programme. | The patient should also have a graded exercise programme. | ||
== See Also == | |||
Open access article.<ref name=":1" /> | |||
== References == | == References == | ||
Latest revision as of 19:55, 7 March 2022
The os peroneum is found within the peroneus longus in 26% of feet,[2] usually located plantar to the cuboid, lateral to the calcaneus, or at the calcaneocuboid joint.[3]It is a factor in the development of os peroneum syndrome.[4]
Anatomy
Part or all of this article or section is derived from Os peroneum imaging: normal appearance and pathological findings by Stefano Bianchi, Chandra Bortolotto, Ferdinando Draghi, used under CC-BY
The peroneal tendon (PT) complex is made up of the muscles and tendons of the peroneus longus tendon (PLT) and peroneus brevis tendon (PBT), their common synovial sheath, the superior and inferior retinaculum, and the Os peroneum (OP).
The peroneal longus (PLM) and brevis (PBM) muscles are located inside the external compartment of the leg, lateral to the fibula. The PLM originates from the proximal portion of the lateral surface of the fibula and from the nearby intermuscular septum. The PBM originates from the distal third of the lateral surface of the fibula and from the nearby intermuscular septum. At the level of the leg’s median third, the PLM extends through a superficial, flat aponeurosis that covers the PBM. The PBM presents a myoaponeurotic junction distally located with regard to that of the PLM. Both muscles are innervated by the peroneal superficial nerve. The peroneal muscles are supplied by two principal source arteries, the anterior tibial artery and the peroneal artery.
At the malleolar region, the two tendons reflect against the posterior aspect of the lateral malleolus. At this level they run inside an osteofibrous tunnel (proximal tunnel) made up of the concave bony gutter and the thick fibrous superior retinaculum. This inserts into the lateral surface of the malleolus and guarantees the stability of the tendons during ankle movement, thus preventing their anterior luxation during movement of the ankle.
Distal to the lateral malleolus, the PT travel along the lateral surface of the calcaneus, which presents a small bony prominence, the peroneal tubercle (PTub). The peroneus brevis tendon (PBT) runs superiorly while the PLT runs inferiorly to it. At this level, the two tendons run inside another osteofibrous tunnel (distal tunnel), stabilized against the calcaneus thanks to the inferior retinaculum, which inserts on the apex of the PTub. The tubercle acts as a pulley for the PLT that reflects on its inferior surface.
Distal to the PTub, the PBT travels straight forward, to insert into the base of the fifth metatarsal bone.
The PLT, after reflecting against the cuboid, reaches the plantar region and attaches to the first and second metatarsal bones.
The two PT are enclosed by a common synovial sheath allowing optimal sliding of the tendons during movements of the ankle and/or contraction of the peroneal muscles. The sheath is made of a parietal layer adherent to the paratendinous soft tissue and a visceral layer adherent to the tendons. Proximal to the PTub the sheath divides to individually surround the two tendons. In some cases, the sheath surrounding the PLT is longer and extends from the cuboid tunnel to the plantar aspect of the foot. In physiologic conditions, it contains only a small amount of synovial fluid.
The OP is a small sesamoid bone which can be found inside the PLT at the level of the calcaneocuboid joint. The OP is ossified in around 20% of the population, and it is bilateral in around 60% of cases. This small sesamoid bone can show different sizes and can also be bipartite or multipartite. A recent cadaveric study described the normal shape and size of the OP on 36 cadavers. The ossicle presented a flattened oval shape, with one or two concave articular deep surfaces. The average thickness was 4 mm and length 13 mm. A bipartite bone is common and can be seen in around 30% of cases.
The presence of an OP or a bipartite OP can be clinically significant. The differential diagnosis between the ossicle and a cortical avulsion or a soft tissue calcification can be difficult in patients with pain in the lateral side of the foot. Similarly, a multipartite bone must be differentiated from a fractured one.
The origin of OP development is controversial. Some authors advocate an embryonic development of the ossicle, while others believe that the OP develops from a “stress response”. A recent cadaveric study from Guimera and colleagues demonstrates that a precursor of the OP is already present during the foetal period. Mittal et al. propose that development of the OP follows local stresses to the tendon, leading to its thickening and secondary ossification.
Pathophysiology
Os peroneum syndrome, also referred to as painful Os peroneum syndrome is a spectrum of conditions associated with an Os peroneum in the lateral foot. It can include the following:[5]
- acute os peroneum fracture or diastasis of a multipartite os peroneum
- chronic (healing or healed) os peroneum fracture or diastasis of a multipartite os peroneum with callus formation which can result in peroneus longus stenosing tenosynovitis.
- attrition or partial rupture of the peroneus longus tendon, proximal or distal to the os peroneum
- frank rupture of the peroneus longus tendon with discontinuity proximal or distal to the os peroneum
- presence of a large peroneal tubercle on the lateral aspect of the calcaneus which entraps the peroneus longus tendon and/or the os peroneum during tendon excursion leading to peroneus longus stenosing tenosynovitis.
Classification
Tears are classified as follows[1]
- Type 1: proximal to the Os peroneum
- Type 2: at the Os peroneum
- Type 3: distal to the Os peroneum
Clinical Features
Patients complain of lateral ankle and/or foot pain.
Physical exam shows tenderness over the lateral plantar cuboid or at the calcaneocuboid joint. There may be thickening and tenderness of the peroneus longus tendons and peroneus brevis tendon sheath. Pain is exacerbated with the heel-rise phase of gait. Pain is also exacerbated by resisted plantarflexion of the first ray (first metatarsal and two phalanges of the great toe). The varus inversion stress test may provoke pain and this is performed by putting the foot in an inverted, supinated, and adducted position. Forced foot eversion may also cause pain.[3]
Investigations
Standard plain films show the Os peroneum (AP, lateral, mortise of the ankle, and AP and oblique of the foot). Also look for fracture, diastasis of multipartite Os peroneum, callus formation, proximal migration of the Os peroneum.[3]
Take care in not mistaking it for:[6]
- os vesalianum pedis
- os cuboideum secundarium
- apophysis of the 5th metatarsal
- avulsion fracture (pseudo-Jones fracture)
Ultrasound can also be useful however only the outer surface of the Os peroneum can be assessed (but it can see displacement). It can however assess the tendons such as for tears and tenosynovitis.[1]
On MRI the Os peroneum can present as a "pseudo-tear" due to its intermediate signal by inexperienced radiologists. It can be very helpful but needs a proper sequence and field of view selection.[1]
Treatment
First line treatments are rest, ice, and NSAIDs.
In severe cases immobilisation of the limb may be required.
Peroneal tendon sheath injection is an option in tenosynovitis.
The patient should also have a graded exercise programme.
See Also
Open access article.[1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Bianchi S, Bortolotto C, Draghi F. Os peroneum imaging: normal appearance and pathological findings. Insights Imaging. 2017 Feb;8(1):59-68. doi: 10.1007/s13244-016-0540-3. Epub 2017 Jan 5. PMID: 28058662; PMCID: PMC5265202.
- ↑ Peterson JJ, Bancroft LW. Os peroneal fracture with associated peroneus longus tendinopathy. AJR Am J Roentgenol. 2001 Jul;177(1):257-8. doi: 10.2214/ajr.177.1.1770257a. PMID: 11418450.
- ↑ 3.0 3.1 3.2 Sobel M, Pavlov H, Geppert MJ, Thompson FM, DiCarlo EF, Davis WH. Painful os peroneum syndrome: a spectrum of conditions responsible for plantar lateral foot pain. Foot Ankle Int. 1994 Mar;15(3):112-24. doi: 10.1177/107110079401500306. PMID: 7951939.
- ↑ Clarke HD, Kitaoka HB, Ehman RL. Peroneal tendon injuries. Foot Ankle Int. 1998 May;19(5):280-8. doi: 10.1177/107110079801900503. PMID: 9622417.
- ↑ Weerakkody, Y., Luong, D. Os peroneum syndrome. Reference article, Radiopaedia.org. (accessed on 07 Mar 2022) https://doi.org/10.53347/rID-76408
- ↑ Gaillard, F., Baba, Y. Os peroneum. Reference article, Radiopaedia.org. (accessed on 07 Mar 2022) https://doi.org/10.53347/rID-7648
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


