Paediatric Fractures of the Upper Extremities
Sternoclavicular Dislocation
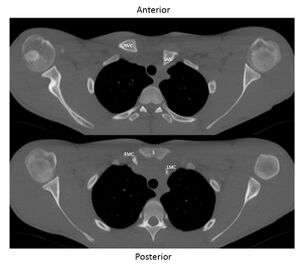
Sternoclavicular (SC) injuries in skeletally immature patients can occur as a result of either a true sternoclavicular dislocation or a medial clavicular physeal separation. The medial clavicular physis is the last to ossify and can fuse as late as 25 years old, so physeal separations can occur in young adults as well. SC injuries are relatively uncommon and account for <1% of pediatric fractures. The clavicle more commonly displaces anteriorly to the sternum, but posterior displacement is more dangerous, as the posteriorly displaced clavicle can cause injury or compression to vital mediastinal structures (Figure 1).
Anterior SC injuries can be felt as a bump near the SC joint with visible deformity. Posterior SC injuries are more subtle and can be easily missed unless clinical vigilance is maintained. Red flags that may help to identify patients requiring more urgent treatment for posterior dislocation include dyspnea, dysphagia, stridor, pulse changes from the contralateral arm, venous congestion of the arm, and paresthesias.
SC injuries can be identified with AP and serendipity (40 degree cephalic tilt) radiographs of the bilateral clavicles in order to detect subtle differences between the injured and un-injured SC joints. Often an axial CT scan will show the diagnosis more definitively, including the direction of dislocation and potential mediastinal compression.
Patients with asymptomatic anterior injuries may be treated non-operatively. Anterior SC injuries can be treated with an attempt at closed reduction, with open reduction and suture fixation reserved for patients with symptomatic instability. Patients with posterior injuries can be treated with open reduction and suture fixation of the SC joint or physeal injury.
Supracondylar Humerus Fractures
Supracondylar (distal humeral metaphysis) fractures of the humerus are the most common elbow injury in children. They usually occur in children between 4 and 8 years old after a fall on an outstretched hand.
Supracondylar fractures can be described as either a flexion or extension injury type, meaning that the distal humerus fragment is flexed or extended relative to the proximal humeral shaft on a lateral radiograph. Extension-type fractures are far more common.
Children with supracondylar fractures present with elbow pain and swelling; deformity and ecchymosis might be present with a more severe injury. The neurovascular exam at presentation is critical in children with supracondylar humerus injuries. The anterior interosseus nerve is most commonly injured in extension-type injuries, and the ulnar nerve is most commonly injured in flexion type injuries. The brachial artery can have decreased flow (owing to stretch or spasm) when it is tented over the distal humeral metaphysis. Examination of radial pulses and perfusion of the hand (including skin color and capillary refill) is required.
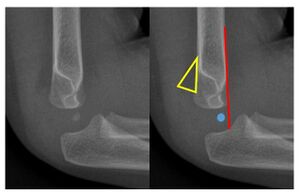
Plain radiographs are sufficient to diagnose supracondylar injuries. Occasionally, non-displaced fractures might not be easily visible. These so-called “occult fracture” can be identified by the presence of a “posterior fat pad sign.” This sign is created when bleeding into the joint elevates the posterior fat pad off the bone (as seen in Figure 2). Radiographs will also demonstrate the direction and degree of displacement in the other injury types.
A line drawn down the anterior humerus can also help to determine the severity of these injuries. Typically the line will intersect the middle third of the capitellum distally, but will cross more anteriorly, or not at all, in the setting of extension type fractures (Figure 2). Fractures can be classified as non-displaced, hinged and completely displaced (separation of both the anterior and posterior cortices).
The differential diagnosis that should be considered includes a distal humerus transphyseal separation, which is a variant of supracondylar fractures that occurs in very young children (neonate to 2 years of age) and is very suspicious for non-accidental trauma. Other diagnoses to consider include lateral condyle fractures, medial epicondyle fractures, and radial neck fractures (discussed below).
A red flag in children with supracondylar fractures is an ipsilateral forearm fracture, as this injury, termed a “floating elbow,” may place patients at a higher risk of compartment syndrome. The three A’s -- anxiety, agitation, and increasing analgesia requirements -- are clues of an impending compartment syndrome.
Pulseless supracondylar injuries with a warm, well perfused hand can often be treated with reduction and fixation of the fracture and close monitoring postoperatively, but patients who present with a white, pulseless hand require urgent treatment, often with operative exploration of the anterior neurovascular bundle.
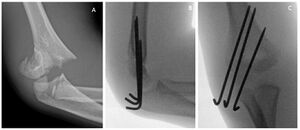
Treatment of supracondylar injuries depends on the pattern of the fracture. Non-displaced injuries can be treated non-operatively with a long arm cast for three weeks. Most incomplete, hinged fractures are treated with closed reduction and percutaneous pinning, but casting might be tried. Completely displaced fractures should all be treated with closed reduction and pinning (Figure 3). Open, rather than percutaneous, pining is reserved for injuries that cannot be anatomically reduced or exploration of the neurovascular bundle is required for pulseless injuries.
Children typically regain full elbow range of motion after resuming their daily activities, and they usually do not require physical therapy. The most common complications of surgical treatment include pin migration and pin site infection. Compartment syndrome can occur as a result of the injury itself or with hyperflexion of the elbow during treatment. Compartment syndrome should be treated urgently with forearm fasciotomies in order to prevent long term ischemic contractures of the forearm and hand. Cubitus varus (an angular malalignment of the elbow, also known as a "Gunstock deformity") can occur with inadequate reduction of the fracture. It usually does not cause significant functional deficits, but can be treated with a distal humerus valgus osteotomy if severe.
Medial Epicondyle Fractures
Medial epicondyle fractures are common injuries of children typically between 9 and 14 years old. These injuries can occur in isolation but 60% are associated with elbow dislocations.
The medial epicondyle is an apophysis (a second growth center) of the distal humerus and begins to ossify between 5-7 years of age. It is the origin site of the flexor-pronator mass of the forearm, as well as the ulnar collateral ligament (the most important valgus stabilizer of the elbow). It is the last physis of the distal humerus to undergo fusion (around age 15) and is at risk of fracture during high valgus stresses to the elbow.
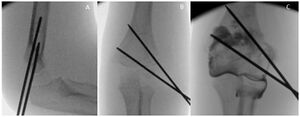
Patients with medial epicondyle fractures will present with medial elbow pain. It is important to obtain any history of instability or self-reduced dislocation at the time of injury, and range of motion and a complete neurovascular exam are important. AP, lateral, and oblique radiographs of the elbow are necessary to evaluate a medial epicondyle fracture, although they can often underestimate the true displacement of the fragment. In cases of elbow dislocation, it is possible for the epicondyle fragment to become trapped in the joint. The joint should be carefully evaluated on lateral radiographs to ensure that the fragment is not trapped and that the joint is congruous (Figure 4). CT scan can help to better estimate the displacement and location of the fragment when treatment is controversial. Differential diagnoses include concurrent elbow dislocation, ulnar collateral ligament injury, and other fractures around the elbow.
Chronic valgus stress to the elbow, e.g. with baseball pitching, can also lead to stress fractures or fibrous unions of the medial epicondyle physis and should be considered. Red flags include instability of the elbow and crepitus or a mechanical block during range of motion. These should alert the examiner to the possibility of a prior dislocation and/or an incarcerated fragment.
Treatment of medial epicondyle fractures has traditionally been non-operative in a long arm cast. Absolute indications for surgical treatment are open fractures and fractures with the medial epicondyle incarcerated in the joint. Citing the high valgus stresses that athletes like gymnasts and throwers place on their medial elbow, some surgeons have advocated operative treatment for this population. Surgical treatment typically consists of open reduction and screw fixation into the medial column, with careful protection of the ulnar nerve. Suture of the ulnar collateral ligament and flexor pronator insertion can augment the fixation of the medial epicondyle.
Loss of motion and bony non-union are two of the most common complications of both surgical and non-surgical treatment of medial epicondyle fractures. Patients tend to have more difficulty regaining full motion after these fractures compared to other pediatric fractures of the elbow, which is why stable fixation to allow early motion is important. While some studies have reported 15-30% non-union rates for medial epicondyle fractures, most patients obtain asymptomatic fibrous unions and do not require further treatment.
Lateral Condyle Fractures
Lateral condyle fractures of the elbow are intra-articular fractures that start in the lateral distal humeral metaphysis and extend into the joint. The forearm extensor muscles originate on the lateral epicondyle and tend to displace fractures posteriorly and laterally.
Lateral condyle fractures are the second most common pediatric elbow fracture. Because most of the lateral condyle fragment is cartilage and not easily visible on radiographs, these fractures are commonly missed on initial imaging. Therefore, a high index of suspicion is needed.
Patients with lateral condyle fractures of the elbow present with elbow pain after a fall, and physical exam typically reveals lateral elbow tenderness and pain with active wrist flexion and extension. AP and lateral radiographs can help to make the diagnosis, but an internal oblique radiograph of the elbow is the most critical view for both diagnosis and determining the degree of displacement. The differential diagnosis for lateral condyle fractures includes supracondylar humerus fractures and radial neck fractures, which can present similarly in pediatric patients and can be difficult to distinguish when they are non-displaced.
Treatment of lateral condyle fractures depends on the degree of displacement. Fractures that are truly non-displaced on all views can be treated non-operatively in a long arm cast for four to six weeks. Any lateral condyle with displacement is typically treated operatively because of their decreased healing potential. Minimally displaced fractures are treated with closed reduction and percutaneous lateral pinning, particularly if the articular cartilage appears to be hinged and remains intact. Closed reduction and percutaneous pinning can be supplemented with a post-reduction arthrogram in order to confirm the reduction and joint congruity (Figure 5).
Significantly displaced fractures, or fractures in which an anatomic reduction cannot be obtained through closed means, are treated with open reduction through a lateral approach to the elbow and percutaneous pinning. Lateral condyle fractures are associated with complications to a greater extent than other pediatric elbow fractures. Possible complications include stiffness, delayed union and non-union, osteonecrosis and deformity. Stiffness is most common and usually resolves with time. Deformity can present as cubitus valgus with or without an ulnar nerve palsy.
Radial Neck Fractures
Radial neck fractures tend to occur in children between 8-11 years old, slightly older than the typical supracondylar humerus fracture. Radial neck fractures can occur in isolation or in combination with other elbow injuries, such as olecranon fractures or elbow dislocations. The ossification center of the radial head begins to ossify between 3 and 5 years old, and fuses with the radial shaft between 16 and 18 years old.
Radial neck fractures often occur after a fall onto an outstretched hand, often when the elbow is extended and undergoes a valgus force. Patients present with elbow pain, tenderness over the radial head, and pain with elbow motion, particularly pronation and supination. Radial neck fractures are described by their degree of angulation relative to the radial shaft. Older children and adolescents who present with tenderness over the radial head but no fracture seen on radiographs can be assumed to have an occult radial head fracture.
The differential diagnosis includes supracondylar and lateral condyle elbow fractures, as well as a nursemaid’s elbow (see below).
Red flags include signs and symptoms of compartment syndrome, which should be considered after higher energy injuries, especially those associated with other elbow injuries like elbow dislocation.
Non-displaced fractures, occult fractures and those with less than 30 degrees of angulation can also be treated non-operatively. Fractures with more than 30 degrees of angulation should be treated with an attempt at closed reduction either in the emergency department or in the operating room. When performed in the operating room, a percutaneous k-wire can also be used to help obtain and maintain the reduction. For more severely displaced fractures that cannot be reduced with closed techniques, an open reduction and percutaneous pinning can be used to fix the fractures.
Loss of pronation and/or supination is the most commonly reported complication of radial neck fractures.
Nursemaid’s Elbow
Nursemaid’s elbow is a common injury in very young children, and it occurs when the annular ligament subluxes and becomes trapped between the radial head and the capitellum. Most nursemaid’s elbows occur in children between 2 and 3 years old; and it is very uncommon after the age of 5. Nursemaid’s elbow occurs after a longitudinal force is applied to the forearm while it is pronated with the elbow in extension, like when a parent pulls on the child’s hand or forearm. The child usually presents with pain and refusal to move the elbow, with the elbow held in flexion and forearm pronation.
Radiographs should be obtained in any children with elbow deformity or a presentation that is not completely consistent with nursemaid’s elbow. (Radiographs are not required to make the diagnosis if the history and exam are classic.) Radiographs, if obtained, are often normal or will show a slight subluxation of the radial head.
The differential diagnosis includes supracondylar or transphyseal humerus fractures, radial neck fractures, and congenital conditions like radioulnar synostosis. Red flags include elbow deformity, unknown mechanism of injury, and children over 5 years old.
Nursemaid’s elbow is easily treated with closed reduction maneuvers. The two most commonly used techniques are: 1- hyperpronation with the elbow in 90 degrees of flexion; 2- supination of the forearm followed by flexion at the elbow. A click is usually felt in the elbow when the annular ligament reduces, and children often feel immediate relief and will start to fully range the elbow again. No further immobilization or treatment is required after reduction, and children typically have good outcomes without any further sequelae related to the elbow. Recurrence of nursemaid’s elbow is sometimes seen in younger children, but usually does not happen again after the age of 5.
Both Bone Forearm Fractures
The radius and ulna form a ring in the forearm that transmits forces from the wrist to the elbow during a fall. Both bone forearm fractures are typically described based on their location (i.e. middle third), direction of angulation, and whether the fractures are complete or incomplete (i.e. greenstick) fractures. The radius and ulna each have a proximal and distal physis, but the distal physis in both of the bones account for the vast majority of growth in the forearm. Thus, fractures closer to the distal physis have greater potential for remodeling after they heal.
Patients with a both bone forearm fracture present with forearm pain and deformity after a fall. The wrist and elbow must be examined for any findings that may signify anything more than a straightforward both bone forearm fracture. The differential diagnoses for this injury include isolated distal radius fracture, a so-called Galeazzi fracture (radial shaft fracture with associated distal radioulnar joint dislocation), or a Monteggia fracture (ulna fracture with associated radial head dislocation). The presence of elbow pain in a patient with a forearm fracture may signify a concomitant supracondylar fracture, creating a “floating elbow” (as discussed above). Other red flags include persistently oozing wounds, which typically indicate an open fracture that requires irrigation and antibiotics.
AP and lateral radiographs of the forearm will demonstrate the fracture pattern. Additional radiographs of the elbow and wrist are necessary to rule out associated injuries of these joints.
Although both bone forearm fractures in adults are often treated surgically, both bone forearm fractures in children are often more stable because the thick periosteum usually remains intact and can usually be treated non-operatively with closed reduction and casting (Figure 6).
Surgical treatment is reserved for fractures with unacceptable alignment after reduction, as well as for both bone fractures in adolescents who have nearly finished growth.
Outcomes after treatment are all typically satisfactory, with at most a mild loss of motion (particularly pronation or supination) but no functional deficits.