Piriformis Syndrome
Piriformis Syndrome is a highly controversial entity that describes extra-spinal entrapment neuropathy of the sciatic nerve by the piriformis muscle. It is a subset of Deep Gluteal Syndrome, as there are many potential sites for extra-spinal sciatic nerve entrapment.
Controversy
It is the opinion of the author and the general consensus of Musculoskeletal Medicine specialists in New Zealand that this condition is over-diagnosed in New Zealand. The flaws in logical reasoning are usually of a material nature. These are the most common reasons that the author has seen for a patient being incorrectly diagnosed as having piriformis syndrome:
- Misreading lumbar MRI imaging. For example not looking at the lateral recesses - where stenosis there is a common cause for radicular pain. Another example is incorrectly believing that proper nerve compression is required for radicular pain to occur. Nerve root compression causes radiculopathy, nerve root inflammation with or without compression is a cause of pain. I.e. "no nerve root compression" does not mean that the pain isn't arising from the nerve roots.
- Not being familiar with the concept of somatic referred pain where pain is arising from structures such as a lumbar disc, lumbar facet joint, or sacroiliac joint.
- Not being aware that buttock pain is extremely common in radicular pain syndromes from disc disease.
- Putting too much emphasis on the straight leg raise test, thinking that a negative test excludes disc disease as a cause.
Complicating matters is that there is no gold standard for diagnosis and so different studies use different inclusion criteria. The research literature is dominated by case studies and review articles and flawed reasoning is a common feature. Using Bogduk's Postulates, the concept fails in postulates 2, 3, and 4.
Finally it is not clear why a compressed sciatic nerve in the buttock would cause pain in addition to loss of function. In the lumbar spine tension or compression of a nerve root only leads to loss of function. You need the additional component of inflammation to cause radicular pain (i.e. from Internal Disc Disruption).
History
Piriformis syndrome was originally described by Robinson in 1948. He described it as a type of sciatica that was due to an abnormal condition of the piriformis muscle, usually of traumatic origin. He presented two post-traumatic cases.[1] However ultrasound and MRI were no available in 1948 to exclude conditions like partial hamstring rupture.
Anatomy and Aetiology
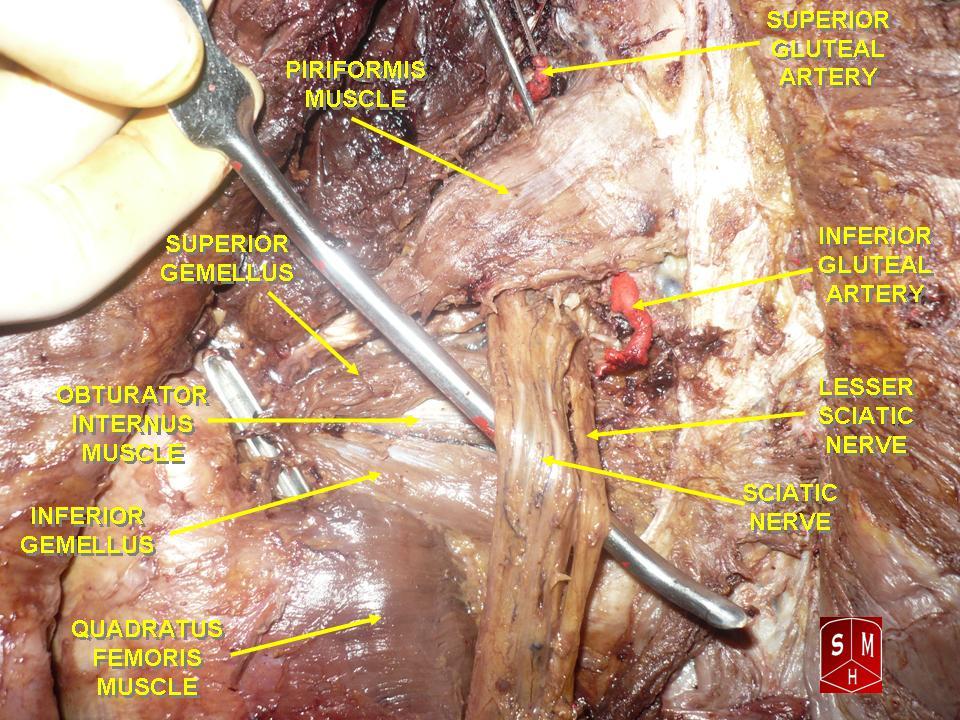
The piriformis muscle runs from the anterior costotransverse bars of S2-4 and inserts onto the piriformis fossa which is on the anterior part of the medial aspect of the greater trochanter of the femur. It works on the hip primarily as an external rotator, but also provides abduction and some weak flexion.
The sciatic nerve typically passes immediately anterior to the piriformis muscle. Both the piriformis muscle and sciatic nerve exit the pelvis through the greater sciatic notch.
Aetiology
Piriformis syndrome is defined as impingement of the sciatic nerve by the piriformis muscle causing buttock pain and sciatica.
Deep gluteal syndrome can been classified into primary and secondary causes.[2]
- Primary: Anomalous anatomy
- Hypertrophy of piriformis. Russell: 66% specificity; 46% sensitivity
- Dynamic nerve entrapment
- Anomalous course
- Secondary: Direct or blunt trauma to the piriformis muscle
Sciatic nerve entrapment may occur subsequent to buttock trauma or sprain of the piriformis muscle which is purported to cause perineural fibrosis. Another mechanism is through anatomical variation where the sciatic nerve branches pass through a bifid piriformis muscle. An accessory piriformis muscle can be implicated.
During downhill running or sprinting, the piriformis muscle undergoes eccentric contraction and some runners may develop the syndrome via this mechanism.
Other causes include muscle hypertrophy, muscle shortening, infection, endometriosis of the sciatic nerve, and leg length discrepancy.
Classification
"Sciatic pain" can be classified into discogenic and non-discogenic causes. The term deep gluteal syndrome is preferable for extra-spinal causes because there are various potential sites for sciatic nerve entrapment.[2] These include:
- Sciatic nerve entrapment - fibrous bands
- Piriformis syndrome
- Gemelli-obturator syndrome
- Hamstring tendinopathy
- Ischiofemoral impingement
- Ischial bursitis
Epidemiology
The author has not found any reliable sources evaluating the prevalence of this condition in those with chronic low back pain or sciatica.
There is a varying prevalence quoted in the literature, with anywhere from rare to 8% in patients with low back and buttock pain. The lack of uniform inclusion criteria, lack of standardised diagnostic criteria, and poor study methodologies all plague assessment of prevalence. Case series are common and they typically report positive outcome from treatment being evidence as proof of diagnosis which is problematic.
Poor referencing is another common problem that plagues the literature of this entity. A 1983 study by P Hallin is often quoted by review authors stating that piriformis syndrome accounts for between 6% to 8% of all sciatica cases.[3] However in the Hallin article there is no discussion or study of the prevalence whatsoever.[4] A July 2021 statpearls article on piriformis syndrome quotes some figures[5], but they reference another statpearls article, which itself doesn't reference the figures.[6]
Naties and colleagues evaluated 147 cadavers and found that 6.4% had anatomical variations of the sciatic nerve around the piriformis muscle.[7] Benzon and colleagues reported data on 30 cadavers and 19 patients and found that anatomical abnormalities causing piriformis syndrome are rare.[8]
Clinical Features
In a 2018 systematic review by Hopayian and Danielyan, the authors reported on a quartet of clinical findings to describe piriformis syndrome. However it remains unknown whether these findings are sensitive and specific to the condition.[9]
- Buttock pain
- More pain while sitting
- External tenderness over the greater sciatic notch
- Pain when tension in the piriformis muscle increases.
There are no data regarding the diagnostic accuracy of any particular clinical sign. All have questionable clinical value. They all look for production of pain or typical symptoms except for tonic external rotation of hip.
| Test | Description |
|---|---|
| Freiburg test | The patient lies prone with knees flexed and then rotates the hip. Or can be performed supine with placing the hip in extension and internal rotation, and then resisting external rotation |
| Pace test | Patient seated. Patient resists abduction and external rotation. |
| Tonic external rotation of hip | Visible sign, hip externally rotated while patient at rest in supine position |
| FAIR | Maintaining the hip in flexion abduction and internal rotation. |
| Beatty | The patient holds the flexed hip in abduction against gravity while lying on the unaffected side |
| Heel-contralateral knee manoeuvre (HCLK) | The patient externally rotates, flexes the hip, and places the heel on the contralateral knee, and then, the examiner flexes the contralateral hip |
| Active piriformis | The patients actively abducts and externally rotates the hip in the lateral position against resistance by the examiner |
| Seated piriformis | The examiner internally rotates the hip and palpates the sciatic notch with the patient seated |
Diagnosis
Endoscopic evaluation has been used for diagnosis but this also has questionable value.
Another diagnostic method is the injection of local anaesthetic into the piriformis muscle with a positive result being resultant pain reduction by a significant but arbitrary percentage.
Electrodiagnostic testing is frequently normal. There are no specific findings for piriformis syndrome.
Imaging
MRI and x-rays can help evaluate for other causes of symptoms. Often MRI of the piriformis muscle is normal, however an accessory piriformis muscle can be identified, and if there is relatively acute sprain or inflammation then there may be an increased T2 signal. Neurophysiology studies are not typically helpful. In one small study, ultrasound evaluation showing increased piriformis thickness was found to be helpful in diagnosis in those without lumbosacral radiculopathy on MRI.[10]
Treatment
Treatment options include physiotherapy, corticosteroid injections, botulinum toxin injections, piriformis tenotomy, and sciatic nerve release.
Resources
- See review by US physiotherapist here
- See Marin et al for a recent open source review [11]
- Closed access review by Miller and colleagues[12]
- ISHA presentation[13]
Summary
- Piriformis syndrome probably exists but it is over-diagnosed, there are numerous other more common causes that can explain the symptoms in almost all individuals
- There is no convincing evidence that the piriformis muscle is anything more than a very rare cause of sciatic nerve compression
- Evidence is based on flawed studies and flawed reasoning
- Deep gluteal syndrome is a better descriptive term to describe non-discogenic radicular pain with a gluteal origin because the anatomical conflict is not always the piriformis muscle
- Deep gluteal syndrome has many pathologies but the same pain, same EMG, some different tests, different anatomical problem, and different possible treatments.
- Injections and surgery are performed too commonly and without adequate justification
References
- ↑ ROBINSON DR. Pyriformis syndrome in relation to sciatic pain. Am J Surg. 1947 Mar;73(3):355-8. doi: 10.1016/0002-9610(47)90345-0. PMID: 20289074.
- ↑ 2.0 2.1 Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol. 2015 Jul;44(7):919-34. doi: 10.1007/s00256-015-2124-6. Epub 2015 Mar 5. PMID: 25739706.
- ↑ Probst et al.. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM & R : the journal of injury, function, and rehabilitation 2019. 11 Suppl 1:S54-S63. PMID: 31102324. DOI.
- ↑ Hallin. Sciatic pain and the piriformis muscle. Postgraduate medicine 1983. 74:69-72. PMID: 6878094. DOI.
- ↑ Hicks BL, Lam JC, Varacallo M. Piriformis Syndrome. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448172/
- ↑ Chang A, Ly N, Varacallo M. Piriformis Injection. [Updated 2021 Dec 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448193/
- ↑ Natsis K, Totlis T, Konstantinidis GA, Paraskevas G, Piagkou M, Koebke J. Anatomical variations between the sciatic nerve and the piriformis muscle: a contribution to surgical anatomy in piriformis syndrome. Surg Radiol Anat. 2014 Apr;36(3):273-80. doi: 10.1007/s00276-013-1180-7. Epub 2013 Jul 31. PMID: 23900507.
- ↑ Benzon HT, Katz JA, Benzon HA, Iqbal MS. Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology. 2003 Jun;98(6):1442-8. doi: 10.1097/00000542-200306000-00022. PMID: 12766656.
- ↑ Hopayian K, Danielyan A. Four symptoms define the piriformis syndrome: an updated systematic review of its clinical features. Eur J Orthop Surg Traumatol. 2018 Feb;28(2):155-164. doi: 10.1007/s00590-017-2031-8. Epub 2017 Aug 23. PMID: 28836092.
- ↑ Zhang et al.. Ultrasound appears to be a reliable technique for the diagnosis of piriformis syndrome. Muscle & nerve 2019. 59:411-416. PMID: 30663080. DOI. Full Text.
- ↑ Martin et al.. Deep gluteal syndrome. Journal of hip preservation surgery 2015. 2:99-107. PMID: 27011826. DOI. Full Text.
- ↑ Miller TA, White KP, Ross DC. The diagnosis and management of Piriformis Syndrome: myths and facts. Can J Neurol Sci. 2012 Sep;39(5):577-83. doi: 10.1017/s0317167100015298. PMID: 22931697.
- ↑ Piriformis Syndrome Is Clearly Overdiagnosed. ISHA Academy. Bataillie F. Oct 5 2018; 277672 (ishasoc.net). Link
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,