Plica Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Authors}} | {{Authors | ||
|Authors=Jeremy | |||
}} | |||
{{Condition | {{Condition | ||
|quality= | |quality=Partial | ||
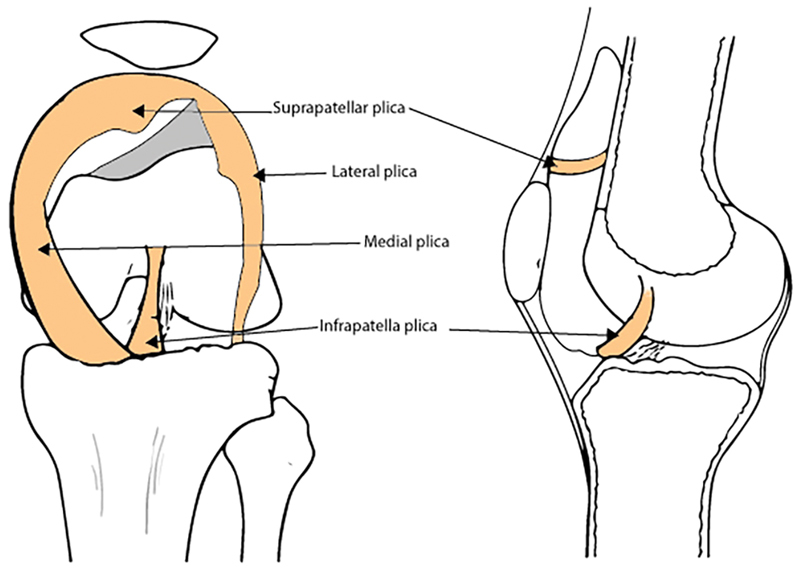
|image=Knee plicae.jpg | |image=Knee plicae.jpg | ||
|caption=The location of the synovial plica in the knee joint | |caption=The location of the synovial plica in the knee joint | ||
|synonym=Synovial plica syndrome | |synonym=Synovial plica syndrome | ||
|pathophysiology=Fibrotic taut plica | |pathophysiology=Fibrotic taut plica | ||
|clinicalfeatures=Anterior and medial knee pain | |clinicalfeatures=Anterior and medial knee pain, positive special tests. | ||
|diagnosis=Clinical and arthroscopic diagnosis | |diagnosis=Clinical and arthroscopic diagnosis | ||
|tests=Imaging is done to exclude other causes of pain. Arthroscopy. | |tests=Imaging is done to exclude other causes of pain. Arthroscopy. | ||
| Line 38: | Line 40: | ||
==Clinical Features== | ==Clinical Features== | ||
[[File:Knee plica inspection.mp4|thumb|Visible clicking on knee inspection.<ref name=":0">{{Special}}{{Open access icon}} {{Cite journal|last=Lee|first=Paul|last2=Nixion|first2=Amy|last3=Chandratreya|first3=Amit|last4=Murray|first4=Judith|date=2017-01|title=Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain|url=http://www.thieme-connect.de/DOI/DOI?10.1055/s-0037-1598047|journal=The Surgery Journal|language=en|volume=03|issue=01|pages=e9–e16|doi=10.1055/s-0037-1598047|issn=2378-5128|pmc=PMC5553487|pmid=28825013}}</ref>]] | [[File:Knee plica inspection.mp4|thumb|Visible clicking on knee inspection.<ref name=":0">{{Special}}{{Open access icon}} {{Cite journal|last=Lee|first=Paul|last2=Nixion|first2=Amy|last3=Chandratreya|first3=Amit|last4=Murray|first4=Judith|date=2017-01|title=Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain|url=http://www.thieme-connect.de/DOI/DOI?10.1055/s-0037-1598047|journal=The Surgery Journal|language=en|volume=03|issue=01|pages=e9–e16|doi=10.1055/s-0037-1598047|issn=2378-5128|pmc=PMC5553487|pmid=28825013}}</ref>]] | ||
The clinical features are often identical to other intra-articular knee pathologies. | The clinical features are often very similar or identical to other intra-articular knee pathologies. | ||
=== History === | === History === | ||
Revision as of 18:10, 25 April 2022
Plica Syndrome is a painful knee condition due to a synovial plica becoming a source of pain due to inflammation. The medial plica is the most commonly symptomatic.
Anatomy
The plicae are embryonic remnants of the normal joint compartment separations that fold inwards and are present in most knees. They are normally a thin (almost transparent), vascular, and pliable band of tissue. They originate from the synovial lining and cross the synovial joint.
Plicae can be found in the suprapatellar, medial, infrapatellar, or lateral compartments of the knee.
Suprapatellar plica - found between the suprapatellar bursa and the knee joint.
Medial plica (synonyms: medial shelf, plica synovialis mediopatellaris, plica alaris elongata, lion's bands, or Aoki edge) - originates from the medial wall of the knee joint, runs down and around the medial femoral condyle, and inserts into the synovium around the infrapatellar fat pad. They are classified as being absent, vestigial, shelf-life, reduplicated, fenestrated, and high-riding.
Infrapatellar plica (synonym: ligamentum mucosum) - originates from the intercondylar notch and inserts into the synovium around the infrapatellar fat pad.
Lateral plica - this is very rare.
Epidemiology
The prevalence is unknown. It is most commonly reported in runners.
Pathophysiology
A plica can become pathological through an inflammatory process. This can occur from direct blunt trauma, repetitive injury, or from irritation from another knee abnormality such as osteochondritis dissecans or inflammatory arthritis. Abnormal knee valgus may also be a factor.
This results in it becoming fibrotic, avascular, and inelastic. It can even become hyalinised. This taut nonpliable band can rub or bowstring over the medial femoral condyle or it can become trapped between the patella and femoral condyle causing impingement.
The medial plica is most commonly symptomatic.
Clinical Features
The clinical features are often very similar or identical to other intra-articular knee pathologies.
History
The symptoms are usually nonspecific anterior or anteromedial knee pain (parapatellar), often following direct trauma or a repetitive injury.
The pain is often worse with sitting for long periods (called the theatre sign) or after sleeping. It is also often worse with squatting, kneeling, or walking upstairs. '
There may be mechanical symptoms such as clicking, catching, clunking, grinding, giving way, or popping with knee flexion and extension.
Examination
On examination for medial plica syndrome there may be slight swelling medial to the patellar margin.
The plica fold is located around the joint lines in the anterior knee compartment. The plica feel like a ribbon of tissue which can be rolled over the medial femoral condyle. The band of tissue runs either parallel or at a slight oblique angle to the medial border of the patellar. Flexing the knee to 90 degrees may make this easier to palpate. Record any tenderness.
Special tests have wide range of reported sensitive and specificity.[1]
Medial patellar plica test: The patient is supine. Apply pressure over the inferomedial border of the patellofemoral joint. This pushes the plica between the medial patella and medial femoral condyle. Maintain the pressure and passively flex the knee from 0 to 90 degrees. A positive test is provocation of pain at this extended position that is relieved at 90 degrees of flexion.
Hughston's plica test: The patient is supine with a relaxed extended knee. Place one hand around the heel and the palm of the other hand over the lateral patella border with fingers over the medial femoral condyle. Passively flex and extend the knee while internally rotating the tibia and pushing the patella medially. A positive test is pain and/or popping in the knee, usually at 30-60 degrees towards extension.
Strutter test: The patient is seated with the knee flexed to 90 degrees. Place two fingers over the centre of the patella. The patient actively extends their leg. A positive test is the patella jumping or stuttering during extension, usually at 45-70 degrees of extension.
A full knee examination should also be performed.
Investigations
The main role of imaging is to exclude other conditions. Investigations are also done to investigate for possible causes of plica irritation - patella subluxation, osteochondritis dissecans, fractures, chondromalacia, etc. Inflammatory arthritis should also be considered.
Arthrography, ultrasound, and MRI are all unreliable at identifying abnormal plicae. They are not required for the initial diagnosis and management.
Arthroscopy is the gold standard for diagnosis.
Differential Diagnosis
- Meniscal Knee Injuries - usually an acute event, mechanical symptoms more common, effusion, positive meniscus provocation tests
- Patellar Subluxation - usually more giving way, pain both medial and lateral. Tenderness more often along medial patella edge or adductor tubercle. Positive apprehension test.
- Hoffa fat pad syndrome
- Patellofemoral Joint Osteoarthritis (but can co-exist) - positive grind test
- Patellofemoral Pain Syndrome - doesn't usually have mechanical symptoms, and pain localised to the medial or lateral patellar facets in extension.
- Snapping ITB syndrome (but can co-exist, usually lateral)
- Ligament instability, such as ACL, MCL
- Patellar Tendinopathy - usually in a running or jumping sport, positive Royal London Hospital test.
- Pes Anserinus Pain Syndrome - pain and tenderness at anatomical pes
- Osteochondritis Dissecans - knee radiographs or MRI can help to distinguish.
- Chondromatosis
- Pigmented villonodular synovitis
- Inflammatory arthritis (but can co-exist)
Treatment
There is limited evidence to guide best treatment. Activity modification, analgesia, limb strengthening, supportive foot wear, weight reduction when relevant, and knee joint corticosteroid injection are often considered.
Surgically the plica can be removed but this should only be done when all other causes are excluded and the patient has had an adequate trial of conservative management because incompletely resected plicae can fibrose can cause symptoms.[1]
References
Papers of particular interest have been highlighted as: ◆ of special interest ◆◆ of outstanding interest
- ↑ 1.0 1.1 1.2 ◆
 Lee, Paul; Nixion, Amy; Chandratreya, Amit; Murray, Judith (2017-01). "Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain". The Surgery Journal (in English). 03 (01): e9–e16. doi:10.1055/s-0037-1598047. ISSN 2378-5128. PMC 5553487. PMID 28825013. Check date values in:
Lee, Paul; Nixion, Amy; Chandratreya, Amit; Murray, Judith (2017-01). "Synovial Plica Syndrome of the Knee: A Commonly Overlooked Cause of Anterior Knee Pain". The Surgery Journal (in English). 03 (01): e9–e16. doi:10.1055/s-0037-1598047. ISSN 2378-5128. PMC 5553487. PMID 28825013. Check date values in: |date=(help)CS1 maint: PMC format (link)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,