Radiofrequency Neurotomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
[[File:C arm.jpg|200px|thumb|right|A C-arm is used to guide needle placement under fluoroscopy]] | [[File:C arm.jpg|200px|thumb|right|A C-arm is used to guide needle placement under fluoroscopy]] | ||
Radiofrequency neurotomy involves an alternating current of high frequency radio waves. The waves produce ion movement which creates friction and the energy is dissipated as heat. Heating nerve tissue >45 degrees causes neural blockade, and heating to 60-100 degrees induces protein coagulation and tissue death. Conventional RF lesion done at 80-85 degrees for 60-90 seconds. Placement is confirmed normally by fluoroscopy. Sensory +/- motor testing can be done but this is controversial and is not generally done in New Zealand. The most important thing is having the patient awake so they can inform you of any unwanted symptoms has the probe heats up. When using traditional radiofrequency, probe placement '''must''' be parallel to the target nerve. This is the technique used in New Zealand, but unfortunately many centres overseas do not do this and this greatly reduces benefit. Pain often recurs after ~400 days but can be repeated. | Radiofrequency neurotomy involves an alternating current of high frequency radio waves. The waves produce ion movement which creates friction and the energy is dissipated as heat. Heating nerve tissue >45 degrees causes neural blockade, and heating to 60-100 degrees induces protein coagulation and tissue death. Conventional RF lesion done at 80-85 degrees for 60-90 seconds. Placement is confirmed normally by fluoroscopy. Sensory +/- motor testing can be done but this is controversial and is not generally done in New Zealand. The most important thing is having the patient awake so they can inform you of any unwanted symptoms has the probe heats up. When using traditional radiofrequency, probe placement '''must''' be parallel to the target nerve. This is the technique used in New Zealand, but unfortunately many centres overseas do not do this and this greatly reduces benefit. Pain often recurs after ~400 days when it comes to medial branch neurotomy, but the procedure can be repeated. | ||
==Indications== | ==Indications== | ||
Revision as of 10:04, 12 July 2020
Radiofrequency neurotomy involves an alternating current of high frequency radio waves. The waves produce ion movement which creates friction and the energy is dissipated as heat. Heating nerve tissue >45 degrees causes neural blockade, and heating to 60-100 degrees induces protein coagulation and tissue death. Conventional RF lesion done at 80-85 degrees for 60-90 seconds. Placement is confirmed normally by fluoroscopy. Sensory +/- motor testing can be done but this is controversial and is not generally done in New Zealand. The most important thing is having the patient awake so they can inform you of any unwanted symptoms has the probe heats up. When using traditional radiofrequency, probe placement must be parallel to the target nerve. This is the technique used in New Zealand, but unfortunately many centres overseas do not do this and this greatly reduces benefit. Pain often recurs after ~400 days when it comes to medial branch neurotomy, but the procedure can be repeated.
Indications
- Generally for nociceptive pain: shut off nociceptive afferents from the painful structure (but not selective).
- Diagnosis should be confirmed with two positive diagnostic blocks. A single positive block can have a high false positive due to the placebo effect.
- RF is not indicated for central pain, spinal cord pathology, serious psychological factors, or when confident pain ratings are not possible.
- In New Zealand it is mostly used for the treatment of confirmed chronic facet joint pain.
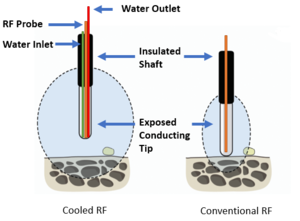
Cooled vs Conventional Radiofrequency
Image modified from Patel 2016[1]
Cooled radiofrequency probes have a special tip allowing cold saline to run through it. It is cooled, but not cold. The saline decreases charring of structures immediately adjacent and allows the extension of the heated field. Energy transfer to a relatively large field (8-10mm), even distal to the probe tip. Energy transfer through a conventional probe is only 3-4mm, and does not extend distal to the probe. With a conventional probe, heating must be done adjacent to any nerve. This is not necessary with a cooled probe. Go to the articles in the see also section for the evidence behind its utility. It is superior to conventional radiofrequency for sacroiliac joint (due to the variable nerve course) and lumbar disc denervation (due to the larger field), but is equal when it comes to lumbar facet joint denervation when done with correct technique.
See Also
- Sacroiliac Joint Precision Treatment
- Lumbar Facet Joint Precision Treatment
- Lumbar Disc Precision Treatment
References
- ↑ Patel N. Twelve-Month Follow-Up of a Randomized Trial Assessing Cooled Radiofrequency Denervation as a Treatment for Sacroiliac Region Pain. Pain Pract. 2016;16(2):154-167. doi:10.1111/papr.12269