Sacroiliac Joint Injection
| |
| Sacroiliac Joint Injection | |
|---|---|
| Indication | Sacroiliac joint pain or dysfunction, sacroiliitis / ankylosing spondylitis, SIJ arthritis |
| Needle | 21-25 gauge 70mm needle |
| Steroid | optional 40mg triamcinolone |
| Volume | Less than 2.5mL. The joint is "leaky" is 20-30%. |
Sacroiliac joint pain is common, and the structure is the source of pain in 16-30% of cases of chronic low back pain. The area can be injected at the bedside, but the gold standard is fluoroscopic guidance. Joint access is not always straightforward and failure to enter the joint is common. See Sacroiliac Joint Precision Treatment for more information about precision treatments for this structure.
Anatomy
- Main article: Sacroiliac Joint Anatomy
The sacroiliac joint is around 1-2mm wide and is formed within S1, S2, and S3. The concave sacral surface joins with the convex ilium surface. The joint has an interlocking mechanism due to an irregular sacral surface. The capsule is often indistinguishable from the surrounding ligaments. The strongest ligament is the interosseous ligament. Other ligaments are the anterior and posterior sacroiliac ligaments, the sacrotuberous ligament which attaches to the coccygeal vertebrae and the ischial tuberosity, and the sacrospinous ligament which joins the ischial spine to the sacrum and coccyx. The anterior joint is thought to be innervated by the ventral rami of L4 and L5, and the posterior joint by the lateral branches of the posterior rami of L5-S4. The superior gluteal nerve contributes.
Indications
Diagnostic block for sacroiliitis / ankylosing spondylitis, SIJ arthritis, SIJ dysfunction, gout, rheumatoid arthritis, psoriasis, congenital deformity
Contraindications
Relative contraindications: Bleeding diatheses, fracture, malignancy
Pre-Procedural Evaluation
Sacroiliac joint pain can't be reliably diagnosed through physical examination or imaging.
Before the injection assess any axial CT imaging available to determine what the orientation of the posteroinferior aspect of the joint is.
Technique
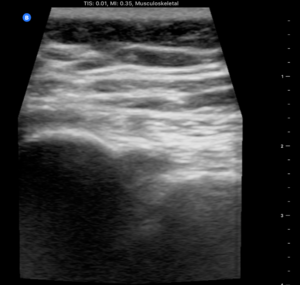
Ultrasound Guided
USS has been shown to have up to 90% success rate[1] and even if not intraarticular then USS ensures peri-articular injection which is believed to be effective.[2]
Landmarks: Patient in prone position. Bony landmarks of PSIS, spinous process L5.
USS landmarks: probe in transverse/axial view from L5, down to the sacral median crest. Probe then goes lateral over the sacrum until the PSIS is visible. The notch in between represents the joint in an axial view. The dorsal SIJ ligaments should be visible connecting the sacrum to the ilium.
Mark out the probe position with permanent marker.
Wipe down area, sterile field: skin prep, sterile jelly, sterile probe.
- Needle placement
- Medial to lateral approach: place probe in position then needle enters skin in midline - approximately 2cm from the heel of the probe and has a shallow trajectory towards probe. Needle tip will appear in joint when under the middle of the probe.
- Caudal to cranial approach: The other option is to enter the needle caudally to the marker on the probe and aim cranially and laterally (15deg) until needle tip enters joint in the midline of the probe. The ultrasound probe placement for this approach is shown in the attached video in the video section.
Local anaesthetic: 27gauge needle USS guidance around and on top of the dorsal ligaments.
Corticosteroid: 21gauge 70mm needle into joint and inject. Note the tactile sensation of pushing through leather then the release once in joint. Joint can take up to 2mm of steroid then will feel resistance.
Landmark Guided
This is not recommended. You can inject the dorsal sacroiliac ligaments but not the joint itself without ultrasound or fluoroscopic guidance. Because of the obliquity of the three dimensional anatomy blind injection is often unsuccessful [2]
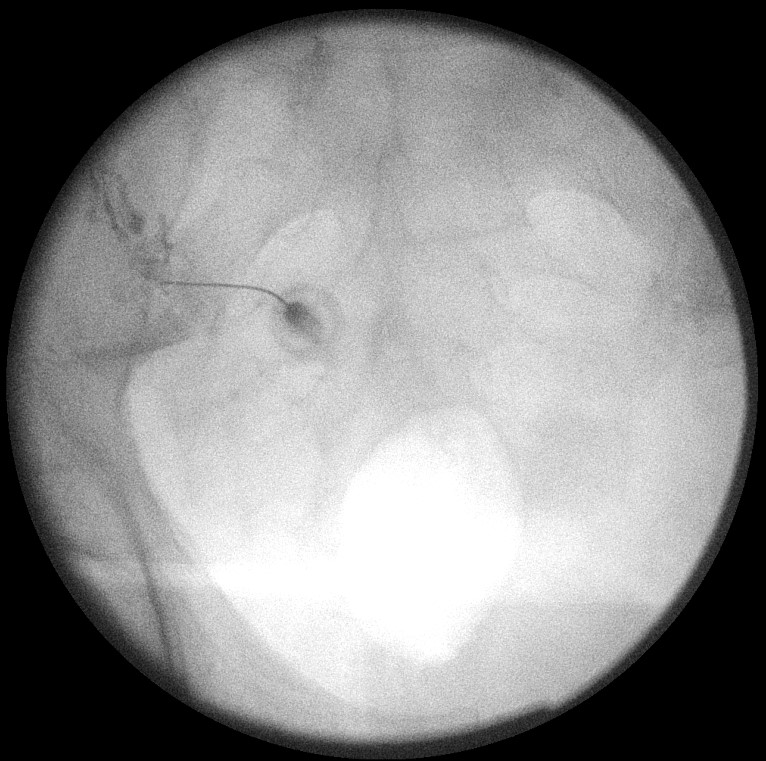
Fluoroscopy Guided
This is a difficult technique. The sacroiliac joint is sinuous and there is great variability between individuals. Prior axial CT imaging can help with working out the orientation of the posteroinferior aspect of the joint is to determine the needle direction. The posterior aspect of the joint, where you direct your needle, is usually the most medial line on an AP view. Osteophytes may cover the posterior joint - they usually grow from lateral to medial. The synovial space is usually only around 1mm in right to left dimensions.
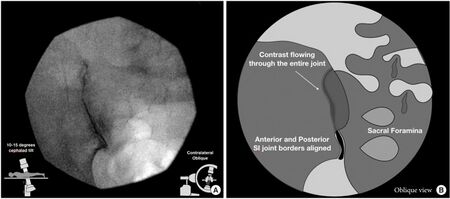
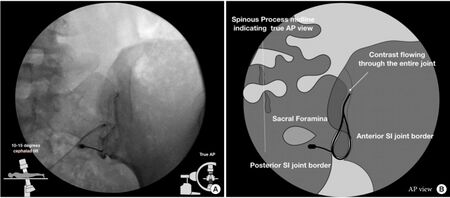
Classic Oblique Approach
- Preparation
- Pre-procedure evaluation with provocation testing
- Patient positioned prone with a pillow under the pelvis
- Prep and drape in a sterile manner
- Target visualisation
- Identify the inferior pole of the target SI joint. Under AP view the SIJ shows multiple sinuous lines that run cranio-caudally. The most medial line is the posterior joint margin.
- The SIJ is usually entered at the inferior posterior aspect. However dorsal osteophytes usually encroach the joint from lateral to medial, and a slight medial to lateral entry may increase the success rate.
- Rotate the C-arm obliquely, usually 5-20 degrees contralateral oblique, so that the anterior and posterior joint margins are superimposed at the caudal 1/3rd of the joint. Then rotate the C-arm in order to separate the anterior and posterior joint margins. The rotation is adjusted until the medial joint line of the medial silhouette is crisp, which means that the beam is aimed towards the posterior access point of the inferior joint space. The joint space should be hyperlucent.
- Use 10-25 degrees of cephalad tilt to isolate the posterior joint place. This tilting displaces the posterior joint plane caudally relative to the anterior joint plane. Make sure that the superior pubic ramus doesn't obscure clear visualisation.
- Select a target 1-2cm cephalad to the inferior end of the joint, and mark the skin here.
- Needle placement
- Optionally infiltrate skin with lidocaine to form a wheal
- Advance the spinal needle towards the joint. Aim initially at the sacrum medial to the joint line to avoid overpenetration.
- When the needle hits the bone, withdraw it slightly and redirect towards the joint space. There should be a loss of resistance and a slight "give". Save image showing the needle tip location.
- Check needle placement on lateral view. The needle should be at S2-3 and at the ventral one third of the sacrum
- Check needle placement in AP view with or without some obliquity.
- Injection
- Inject a small volume of contrast under live fluoroscopy looking for an arthrogram with filling of the inferior recess of the capsule. Save image. If contrast isn't able to be injected the withdraw needle slightly, rotate, and re-attempt.
- The joint is leaky in about 20-30% of patients. Flow outside the SIJ reduces the specificity of the injection.
- Check AP and lateral views for capsule disruption
- For diagnosis: inject local anaesthetic e.g. lidocaine 2% 1-1.5mL. For possible therapeutic benefit add corticosteroid for a maximum volume of 1.5-2mL.
- Withdraw needle, apply dressing
Posteroanterior Approach
One RCT found that the PA approach was superior to the oblique approach.[3]
Post-Procedural Care
Evaluate 30-60 minutes post procedure with provocative testing. In the event of sensory and/or motor deficit then the injection lacks specificity and is non-diagnostic.
Complications
Infection - risk 1:10,000. Fatty atrophy. Skin depigmentation. Risks mitigated if sterile field and steroid not injected subcutaneously.
Aftercare
Post procedure: dressings, icepack, education, exercises, pain diary.
Videos
Resources
References
- ↑ Klauser et al.. Feasibility of ultrasound-guided sacroiliac joint injection considering sonoanatomic landmarks at two different levels in cadavers and patients. Arthritis and rheumatism 2008. 59:1618-24. PMID: 18975358. DOI.
- ↑ 2.0 2.1 Hartung et al.. Ultrasound-guided sacroiliac joint injection in patients with established sacroiliitis: precise IA injection verified by MRI scanning does not predict clinical outcome. Rheumatology (Oxford, England) 2010. 49:1479-82. PMID: 20019067. DOI.
- ↑ 3.0 3.1 3.2 Chauhan, Gaurav; Hehar, Prabhdeep; Loomba, Vivek; Upadhyay, Aman (2019-06). "A Randomized Controlled Trial of Fluoroscopically-Guided Sacroiliac Joint Injections: A Comparison of the Posteroanterior and Classical Oblique Techniques". Neurospine. 16 (2): 317–324. doi:10.14245/ns.1836122.061. ISSN 2586-6583. PMC 6603830. PMID 30531656. Check date values in:
|date=(help)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,