Scaphoid Fracture
The scaphoid (also known as the carpal navicular) is perhaps the most important of the eight carpal bones. The scaphoid links the carpal bones closest to the radius and ulna, the so-called the “proximal row,” to those articulating with the metacarpals, the “distal row.” Owing to its tenuous blood supply, the scaphoid is particularly susceptible to osteonecrosis (and ensuing post-traumatic arthrosis) after fracture. Unfortunately, the scaphoid is also the most commonly fractured of the eight carpal bones (Figure 1). Fracture is usually caused by a fall on an outstretched hand (a mechanism also associated with distal radius fractures and radial head fractures).
Structure and Function
The scaphoid can be morphologically divided into three anatomic regions: proximal third (proximal pole), central third (waist), and distal third (distal pole). A tuberosity on the distal palmar aspect serves as an attachment site for the transverse carpal ligament. Nearly 2/3 of all scaphoid fractures occur at the waist, with 15% occurring at the proximal pole, 10% at the distal pole, and 8% at the tuberosity.
The scaphoid (Figure 2) articulates with the radius and four carpal bones (lunate, trapezium, trapezoid, and capitate). To accommodate so many articulations, 80% of the scaphoid is covered with cartilage.
The scaphoid is supported by the radioscapholunate ligament which stabilizes the scapholunate articulation and acts as a neurovascular conduit. The scaphoid does not have any tendinous attachments.
The scaphoid receives its primary blood supply from the dorsal scaphoid branches of the radial artery, which enter the scaphoid at a point near the distal pole. As such, the scaphoid is perfused in the distal to proximal direction ("retrograde blood supply").
Because of this retrograde blood supply, an injury to the scaphoid waist (i.e. the middle third of the bone) can interrupt blood supply to the proximal pole. (This is analogous to femoral neck fractures and resulting femoral head ischemia: just as the vessels to the femoral head must traverse the femoral neck, the blood supply to the proximal pole of the scaphoid must traverse the waist).
Epidemiology
The scaphoid is the most commonly fractured carpal bone. Fractures of the scaphoid often occur in physically active individuals, and have two to four times greater incidence in men than woman, with peak prevalence between 15-25 years of age. The most common mechanism of injury is a fall onto an outstretched hand.
The true incidence of scaphoid fractures has been difficult to calculate particularly because many of these injuries are undiagnosed. One estimate is that scaphoid fractures represent 1 out of 100,000 people per year.
The prevalences of involved fracture site is as follows:
- Waist area: 60-85%
- Distal third: 25%
- Proximal third: 5-15%
Clinical Features
Patients with scaphoid fractures will often present with radial sided wrist pain (worsened with gripping or squeezing), variable swelling and limited range of motion. Because scaphoid fractures may occur without bruising or visible deformity, patients may assume a less serious injury and delay seeking evaluation. Scaphoid fracture usually results from fall onto an outstretched hand generally during a sports-related event. The patient describes radial-sided pain but there may be relatively little pain.
During examination, it is important to always compare the injured to the uninjured wrist. Clinical exam has high sensitivity but low specificity. See Carpenter et al for a comprehensive review from 2014.[1]
| Test and Study Quality | Description and Positive Findings | Population | Reference Standard | Sens | Spec | + LR | - LR |
|---|---|---|---|---|---|---|---|
| Snuffbox tenderness[3] | Examiner palpates anatomic snuffbox. Positive if pain is elicited | 85 patients presenting to emergency department with mechanism of injury suggesting possible scaphoid fracture | Radiographic confirmation of scaphoid fracture | 100% | 98% | 50.0 | 0.0 |
| Pain with resisted supination[3] | Examiner holds patient’s hand in handshake position and directs patient to resist supination of forearm. Positive if pain is elicited | 100% | 98% | 50.0 | 0.0 | ||
| Pain with longitudinal compression of thumb[3] | Examiner holds patient’s thumb and applies long-axis compression through metacarpal bone into scaphoid. Positive if pain is elicited | 98% | 98% | 49.0 | 0.02 | ||
| Anatomic snuffbox tenderness[4] | Examiner palpates anatomic snuffbox. Positive if pain is elicited | 221 patients with a suspected scaphoid injury | 100% | 29% | 1.41 | 0.0 | |
| Scaphoid tubercle tenderness[4] | Examiner applies pressure to scaphoid tubercle. Positive if pain is elicited | 83% | 51% | 1.69 | 0.33 | ||
| Scaphoid compression tenderness[4] | Examiner holds patient’s thumb and applies long axis compression through metacarpal bone into scaphoid. Positive if pain is elicited | 100% | 80% | 5.0 | 0.0 |
Differential Diagnosis
- Radial styloid fracture. Here, the tenderness is more proximal; radiographs should make the diagnosis.
- Distal radius fracture. Tenderness localizes to distal radius and deformity may be present; radiographs should make the diagnosis.
- Scapholunate instability. In this condition, the tenderness is more toward the ulnar side of the hand (over the scapholunate ligament) and radiographs should show a gap between scaphoid and lunate (scapholunate dissociation: the Terry Thomas sign).
- Flexor carpi radialis tendon injury. This can be diagnosed by noting pain elicited with resisted wrist extension.
- De Quervain Tendinopathy. A positive Finkelstein's test may help make the diagnosis.
- Carpometacarpal joint arthritis. Here, radiographs should make the diagnosis, but recall that a patient with arthritis can suffer a superimposed injury.
As noted, fracture of the scaphoid is usually caused by a fall on an outstretched hand, the same mechanism associated with distal radius fractures and radial head fractures. The astute clinician must be mindful of these potentially associated injuries.
Red Flags
A fall on the outstretched wrist is itself a "red flag" and should raise suspicion for a scaphoid fracture. When there is tenderness in the anatomic snuff box, even if radiographs appear negative, a scaphoid fracture is even more likely.
Imaging
Plain Radiographs
Plain radiographs are essential for all patients with suspected scaphoid fractures. A scaphoid series should be done which is four projections and is positionally different from the wrist series. Standard radiographs include anteroposterior (AP), lateral, oblique and scaphoid views. The scaphoid view is a posteroanterior (PA) view of the wrist, with the wrist positioned in 45 degrees of ulnar deviation and pronated obliquely at 45 degrees.
Features include:[5]
- visualisation of the fracture +/- displacement
- soft tissue swelling and lateral displacement of the adjacent fat pads
- scaphoid fat pad sign: obliteration or lateral displacement of a straight/convex lucent line on the lateral aspect of the scaphoid 11
- associated scapholunate ligament disruption (Terry Thomas sign) which can be accentuated with a clenched fist view
The first sign of avascular necrosis is slight sclerosis.
See radiopaedia for radiology cases.[5]
Initial radiographs can miss 5-20% of fractures in the acute setting. Because initial radiographs of a scaphoid fracture may appear normal, patients with pain in the snuff box and a fall on the outstretched hand should be immobilised and sent for additional imaging studies.
MRI
The international standard for the initial assessment appears to be early MRI in the presence of clinical features and a normal radiograph, or CT if MRI is not available. In New Zealand neither of these imaging modalities is available in primary care. MRI is preferred due to to its superior sensitivity and sensitivity, and also as it can pick up other injuries. The downside other than cost to MRI is that is can detect clinically insignificant abnormalities as well, prompting unnecessary worry to say nothing of unnecessary treatment
In some areas there may be rapid access to a specialist clinic. Otherwise the patient should be offered a private MRI.
Treatment
Initial Treatment
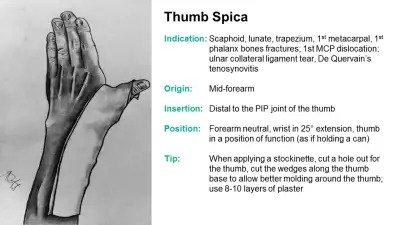
The lack of availability of MRI or CT in primary care in New Zealand has implication on management. If the patient is not able to access early MRI, the standard practice is treat any FOOSH injury with scaphoid tenderness in spite of a normal radiograph as a possible fracture, and immobilise in Plaster of Paris for 10 days and then organise a follow up xray. At that point, the absence of fracture line or healing response on x-ray at 10-14 days, coupled with an absence of tenderness on exam reasonably excludes the diagnosis of fracture.
With casting there should be slight palmar flexion and radial deviation. Usually the thumb is not included. Initial immobilisation reduces the chance that a non-displaced occult fracture becomes a displaced fracture, and in turn, minimises the risk of blood supply disruption.
Refer to orthopaedics for all proximal scaphoid fractures or fractures that are displaced by 1mm or more, as well as patients with acute complete scapholunate ligament rupture.
Mid-waist or Distal Fracture
Mid-waist or distal fracture: Below elbow cast without the thumb. At one week change to fibreglass if POP was used initially. At 6 weeks remove the cast and x-ray. If the patient is still uncomfortable then request a CT to assess healing.
Scaphoid Tubercle Fracture
Apply a below elbow cast for 4-5 weeks for comfort. Non-urgent orthopaedic assessment is recommended.
Proximal Scaphoid Fracture
Consider surgery if displacement of 1mm or more
Surgery
Comminuted, displaced or unstable scaphoid fractures benefit from surgical fixation. The precise indications for surgery (that is, how much linear or angular displacement is enough?) are not known.
The favoured technique is open reduction internal fixation with screws (Figure 6). The choice of fixation depends on a multitude of factors, such as the location of the fracture, configuration of the fracture, functional concerns, and patient factors.
Ligamentous Injuries
If there is a partial scapholunate ligament injury or extrinsic dorsal ligamentous injury then treat with a compression bandage and refer for physiotherapy for splinting and rehabilitation.
If there is complete scapholunate ligament rupture (scapholunate dissociation) then refer to orthopaedics for consideration of surgery. In this condition there is a gap between the scaphoid and lunate of ≥ 3 mm. A clenched fist view can be used to confirm.
Hand Physiotherapy
Hand physiotherapy should be offered following scaphoid injuries.
Prognosis
Incorrect management can lead to delayed union, non-union, or avascular necrosis. Delayed union or non-union is usually due to delayed or inadequate stabilisation, but can also be due to fracture instability.
Scaphoid fractures (especially if not recognized and therefore not treated) can result in post-traumatic arthritis. Once arthritis is evident at the radiocarpal joint there are salvage surgical procedures that can be performed. These include a proximal row carpectomy, scaphoid excision and midcarpal arthrodesis, or a total wrist arthrodesis.
Miscellany
Scaphoid derives from the Greek word skaphos, which means “a boat.” The English word "skiff" has a similar origin. The scaphoid is also referred to as the carpal navicular (coming from navis, the Latin word for "boat,” from which we get the English word "navy," for example). Given that there is also a boat-like bone in the foot, it is probably best to refer to the bone in the hand as the scaphoid and the one in the foot as the navicular.
Regardless of length of immobilization after a scaphoid fracture, appropriate physical and occupational therapy is needed after removal of the cast or splint to optimize range of motion and function.
Smoking is strongly associated with nonunion after surgical fixation of the scaphoid.
Further Reading
References
Part or all of this article or section is derived from Scaphoid Fractures by Orthopaedia.com, used under CC-BY-NC-SA
- ↑ 1.0 1.1 Carpenter CR, Pines JM, Schuur JD, Muir M, Calfee RP, Raja AS. Adult scaphoid fracture. Acad Emerg Med. 2014 Feb;21(2):101-21. doi: 10.1111/acem.12317. PMID: 24673666.
- ↑ Cleland, Joshua, Shane Koppenhaver, and Frank H. Netter. Netter's orthopaedic clinical examination : an evidence-based approach. Philadelphia, Pa: Saunders/Elsevier, 2011.
- ↑ 3.0 3.1 3.2 Waeckerle JF. A prospective study identifying the sensitivity of radiographic findings and the efficacy of clinical findings in carpal navicular fractures. Ann Emerg Med. 1987;16:733-737
- ↑ 4.0 4.1 4.2 Grover R. Clinical assessment of scaphoid injuries and the detection of fractures. J Hand Surg [Br]. 1996;21:341-343
- ↑ 5.0 5.1 https://radiopaedia.org/articles/scaphoid-fracture
- ↑ Clementson et al.. Acute scaphoid fractures: guidelines for diagnosis and treatment. EFORT open reviews 2020. 5:96-103. PMID: 32175096. DOI. Full Text.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,