Scaphotrapeziotrapezoid (STT) Joint Injection
| |
| Scaphotrapeziotrapezoid (STT) Joint Injection | |
|---|---|
| Indication | Scaphotrapeziotrapezoid Joint Pain |
| Syringe | 2mL |
| Needle | 25-gauge 38mm |
| Steroid | 20mg triamcinolone |
| Local | 0.5mL lidocaine |
| Volume | 1mL |
Anatomy
The Scaphotrapeziotrapezoid (STT) or triscaphe joint is the joint that is shared between the scaphoid, trapezium, and trapezoid wrist bones. The STT joint may communicate with the rest of the mid-carpal articulation. In patients with inflammatory arthritis or osteoarthritis, the midcarpal articulation (including the STT joint) may communicate with the radiocarpal articulation and/or the flexor carpi radialis sheath.[1]
Indications and Efficacy
- Main article: Scaphotrapeziotrapezoid Joint Pain
Scaphotrapeziotrapezoid (STT) joint osteoarthritis is the second most common pattern of wrist arthritis. The typical clinical picture is activity-related dorsal or radial sided wrist pain in older patients along with reduced grip strength and variable motion loss. The diagnosis of STT joint pain is challenging. Ultrasound guided injection of the joint can aid in making the diagnosis of pain arising from this joint.
Technique
A cadaver study found that ultrasound was 100% accurate, and landmark guidance was 80% accurate.[1]
Ultrasound Guided
The following is a technique described by Smith et al. In their cadaver study, 30% (6 of 20) had overflow of latex into the radiocarpal articulation or flexor carpi radialis tendon sheath. This may affect diagnostic specificity. In 5 of the 6 cases, overflow was observed by the clinician during ultrasonography. [1]
- Palmar approach, with palm facing ceiling
- Identify the STT joint
- Place the transducer parallel to the long axis of the metacarpal of the thumb.
- Translate the transducer proximally to identify the carpometacarpal joint.
- Translate the probe further proximally still to identify the STT joint, the thick palmar scaphotrapezoidal ligament, and the joint capsule.
- Visualise the joint space between the scaphoid and trapezium, just radial to the flexor carpi radialis. The scaphoid can be confirmed by seeing it's waist.
- Visualise the superficial palmar branch of the radial artery within the subcutaneous tissue over the scaphoid tubercle.
- Optimise visualisation of the joint and capsuloligamentous complex by using radial deviation to palmarflex the scaphoid and ulnar deviation to dorsiflex it.
- Move the transducer to the centre of the joint on the display screen
- Needle approach
- Use an out-of-plane (short-axis) approach.
- Place the needle into the centre of the radial side of the transducer's long axix.
- Advance the needle into the STT joint by passing it between the adjacent cortices of the scaphoid and trapezium. This keeps the needle radial and deep to the superficial palmar branch of the radial artery.
- Inject 1mL of solution under direct sonographic visualisation.
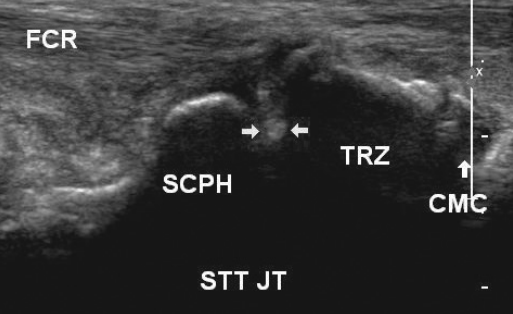
The transducer is over the STT joint, almost parallel to the first metacarpal. The needle is advanced out-of-plane in a radial-to-ulnar direction.
©2011 by the American Institute of Ultrasound in Medicine[1]On ultrasound the needle is an echogenic dot (horizontal arrows) between the scaphoid (SCPH) and trapezium (TRZ). Also seen are the carpometacarpal joint (CMC) to the right of the STT joint (STT JT), and the flexor carpi radialis tendon (FCR). Bottom is deep; left, proximal; right, distal; and top, superficial.
©2011 by the American Institute of Ultrasound in Medicine[1]
Landmark Guided
The following is a technique described by Smith et al.[1]
- Dorsal approach with hand pronated flat on surface
- Palpate the STT joint just radial to the extensor pollicis longus tendon at the base of the anatomic snuff box.
- Palpate the radial artery to determine course
- Mobilise the thumb metacarpal-phalangeal joint to ensure that the STT joint is being palpated and not the carpometacarpal joint.
- Advance the needle perpendicular to the skin in a palmar direction until the capsule is felt to be penetrated by feeling a distinct puncture.
- Take care to avoid puncture of the radial artery
Landmark guided scaphotrapeziotrapezoid (STT)joint injection using a dorsal approach. The needle is advanced from a dorsal approach with slight ulnar angulation.
©2011 by the American Institute of Ultrasound in Medicine[1]
Complications
Radial artery puncture, skin atrophy.
Videos
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,
![The transducer is over the STT joint, almost parallel to the first metacarpal. The needle is advanced out-of-plane in a radial-to-ulnar direction. ©2011 by the American Institute of Ultrasound in Medicine[1]](/w/img_auth.php/7/7e/STT_joint_ultrasound_tranducer_placement_smith.png)
![Landmark guided scaphotrapeziotrapezoid (STT)joint injection using a dorsal approach. The needle is advanced from a dorsal approach with slight ulnar angulation. ©2011 by the American Institute of Ultrasound in Medicine[1]](/w/img_auth.php/thumb/1/16/STT_joint_landmark_injection_smith.png/545px-STT_joint_landmark_injection_smith.png)


