Sjogren's Syndrome: Difference between revisions
(Created page with "Sjögren's syndrome (SS) is a chronic autoimmune disease that is characterised by reduced lacrimal and salivary gland function resulting in dry eyes and dry mouth. It can also...") |
mNo edit summary |
||
| (12 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
Sjögren's syndrome (SS) is a chronic autoimmune disease that is characterised by | {{Authors | ||
|Authors=Jeremy | |||
}} | |||
{{Condition | |||
|quality=Partial | |||
|image=Sjogrens Syndrome.jpg | |||
|synonym=Sjogren's disease | |||
|epidemiology=Prevalence 0.04%. Onset middle age particularly in women. | |||
|causes=Autoimmune disease | |||
|pathophysiology=Cyclical innate and adaptive immune system activation with lymphocytic infiltration of affected tissue | |||
|clinicalfeatures=Glandular and extraglandular disease | |||
|diagnosis=Objective findings of dry mouth or dry eyes plus serologic or histologic findings. | |||
|tests=ANA, Anti-Ro, Anti-La, RF, biopsy, MRI or USS | |||
|prognosis=Normal life expectancy | |||
}} | |||
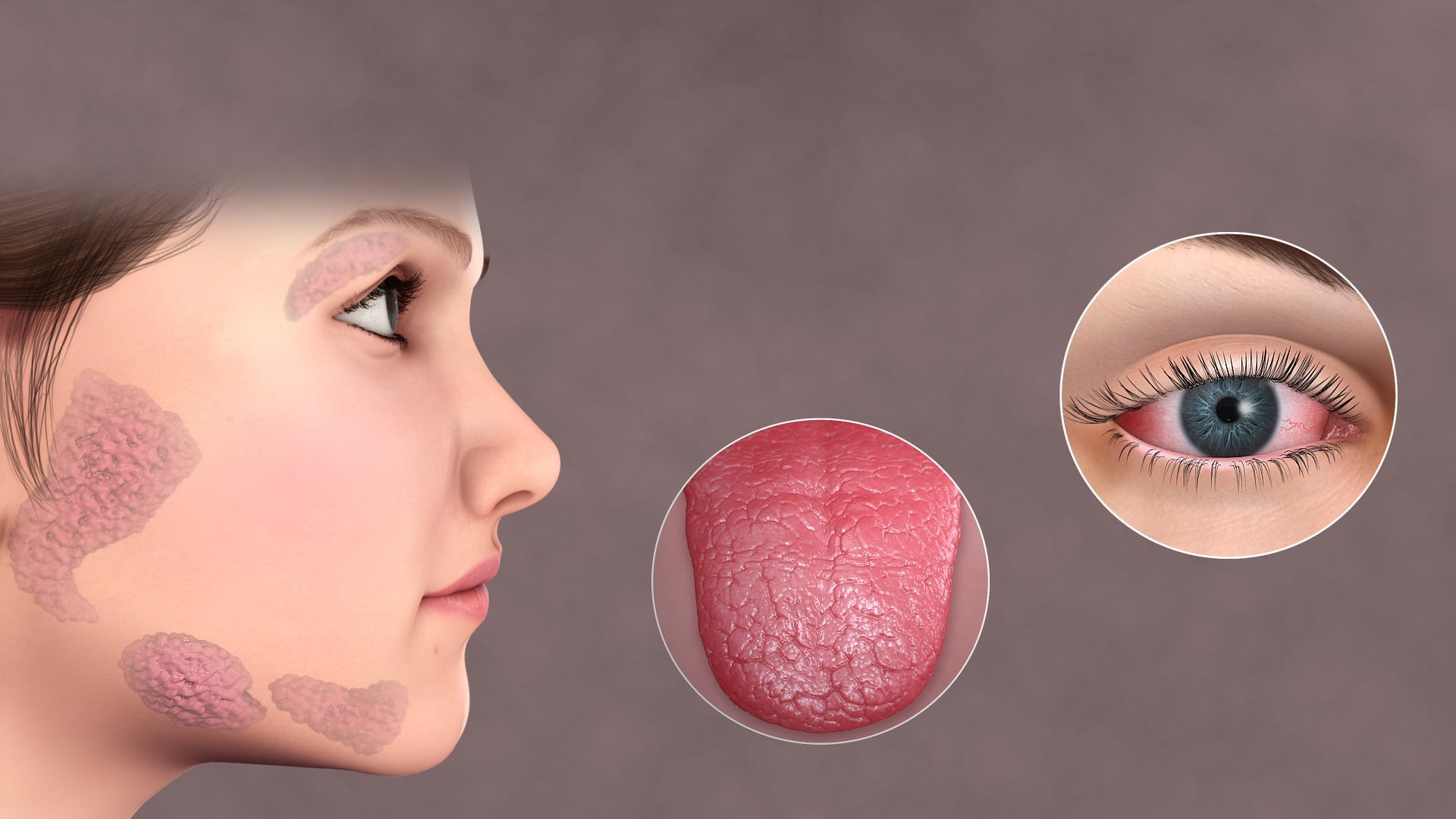
Sjögren's syndrome (SS) is a chronic autoimmune disease that is characterised by lymphocytic infiltration of the salivary, lacrimal, and other exocrine glands leading to dry eyes and dry mouth along with autoantibodies. It can also result in skin disease, arthritis, nephritis, cytopaenia, pneumonitis, vasculitis, peripheral neuropathy, myelopathy, and cognitive dysfunction. The clinical features are divided into exocrine glandular features and extraglandular features. | |||
== Definitions == | |||
* Sjogren's disease - synonym for SS | |||
* Sicca syndrome - synonym for SS | |||
* Sicca complex - dryness of the eyes and mouth. Doesn't specify autoimmunity | |||
* Keratoconjunctivitis sicca (KCS) - ocular findings of SS | |||
* Dry eye syndrome (DES) - can be due to conditions such as SS and meibomian gland dysfunction. Only 10% of patients have SS. | |||
* Mikulicz syndrome - parotid and lacrimal gland enlargement from any cause. Including SS or other conditions such as IgG4 related disease. | |||
== Epidemiology == | |||
SS is most common in women, the female to male ratio often exceeds 10:1. It usually is diagnosed between 40-60 but it can occur in younger and older individuals as well.<ref name=":0">Hochberg. Sjogren syndrome (chapter 147) In: Rheumatology. 2019</ref> The overall prevalence is estimated at 43 per 100,000 people (0.043%).<ref>{{Cite journal|last=Qin|first=Baodong|last2=Wang|first2=Jiaqi|last3=Yang|first3=Zaixing|last4=Yang|first4=Min|last5=Ma|first5=Ning|last6=Huang|first6=Fenglou|last7=Zhong|first7=Renqian|date=2015-11|title=Epidemiology of primary Sjögren's syndrome: a systematic review and meta-analysis|url=https://pubmed.ncbi.nlm.nih.gov/24938285|journal=Annals of the Rheumatic Diseases|volume=74|issue=11|pages=1983–1989|doi=10.1136/annrheumdis-2014-205375|issn=1468-2060|pmid=24938285}}</ref> Dry eye and mouth occurs in up to 30% of older adults. This can be due to medication side effects and age-related atrophy of gland tissue. | |||
== Pathogenesis == | == Pathogenesis == | ||
The pathogenesis is one of targeted inflammation of the lacrimal and salivary glands with B-lymphocyte hyperactivity.<ref name=":0" /> | |||
Both genetic and non-genetic factors are thought to be involved. It is thought that SS occurs following an environmental trigger, likely viral (but no single virus has been implicated), in a genetically susceptible individual. The immune response involves both innate and adaptive immunity leading to autoimmunity and chronic inflammation. There is a cycle of mutual stimulation of the innate and acquired immune systems resulting in glandular injury. | Both genetic and non-genetic factors are thought to be involved. It is thought that SS occurs following an environmental trigger, likely viral (but no single virus has been implicated), in a genetically susceptible individual. The immune response involves both innate and adaptive immunity leading to autoimmunity and chronic inflammation. There is a cycle of mutual stimulation of the innate and acquired immune systems resulting in glandular injury. | ||
The pathologic lesion is a lymphocytic infiltration of affected organs. The most frequently affected tissues are the lacrimal and salivary glands | The pathologic lesion is a lymphocytic infiltration of affected organs. The most frequently affected tissues are the lacrimal and salivary glands whereby there is focal aggregation of lymphocytes that start around the ducts and spread to the entire lobule. Infiltrates can also occur in extraglandular sites. Other mechanisms contribute to glandular dysfunction including antibodies to the muscarinic receptors that impair neural innervation of the gland as well as deleterious effects of cytokines on neurotransmitter release. | ||
Specific autoantibodies are found in SS, particularly anti-Ro/SSA and anti-La/SSB in 60-80% of individuals. ANA antibodies are positive in around 90% of patients. High RF factor is also common. Autoantibodies can be found many years before the onset of SS. Autoantibodies alone are not sufficient for disease induction. | Specific autoantibodies are found in SS, particularly anti-Ro/SSA and anti-La/SSB in 60-80% of individuals. ANA antibodies are positive in around 90% of patients. High RF factor is also common. Autoantibodies can be found many years before the onset of SS. Autoantibodies alone are not sufficient for disease induction. | ||
== Clinical Presentation == | |||
SS occurs on a spectrum with a range of presentations. Symptoms can include fatigue, arthralgia, polyarthritis, renal, neurologic, cutaneous, endocrine, hepatic, vasculitis, pulmonary, and haematologic manifestations. | |||
On the mild to moderate side, patients have dry eyes and mouth along with fatigue, cognitive dysfunction, and myalgia. The diagnosis is confirmed by positive antibodies and/or gland biopsy. Without laboratory or histological studies the presentation may be identical to [[fibromyalgia]] or even patients with depression who have anticholinergic side effects from medication. | |||
On the severe end patients may have frank salivary gland swelling and adenopathy. There may be cryoglobulinaemia, low complement, Hodgkin lymphoma, and extraglandular disease. Antibodies may again be positive. | |||
In a minority of patients there is primary extraglandular involvement with limited eye or mouth symptoms. The diagnosis may be made, e.g. with positive antibodies, during workup of neuropathies, nephropathies, interstitial pneumonitis, or haematologic abnormalities. | |||
== Diagnosis == | |||
There is no single test. The diagnosis is made with having both objective clinical and laboratory features, following exclusion of other causes. The diagnosis can't be made with the presence of autoantibodies and no compatible symptoms. | |||
'''Objective clinical findings of mouth or eye dryness:''' this includes one of abnormal Schirmer test of either eye, abnormal sialometry or Saxon test for the glands, or radiological evidence such as on MRI, CT, or US. | |||
'''Serological or histological findings''': Anti-Ro/SSA +/- Anti-La antibodies or positive labial salivary gland biopsy showing focal lymphocytic sialednitis. In the presence of isolated anti-La antibodies, biopsy is required to confirm the diagnosis. A diagnosis of secondary SS can be made without antibodies or biopsy in the presence of a well-established systemic rheumatological disease such as SLE or [[Rheumatoid Arthritis|RA]]. Also acceptable are positive anticentromere antibodies without systemic sclerosis or findings of ANA greater or equal to 1:320 along with positive RF. | |||
In individuals with isolated extraglandular disease, the diagnosis can be made with positive biopsy and anti-Ro antibodies. | |||
{| class="wikitable" | |||
|+2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren Syndrome<ref>Shiboski CH, Shiboski SC, Seror R, et al; International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism Classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheum. 2017;69(1):35-45.</ref> | |||
| colspan="2" |The classification of primary Sjögren syndrome applies to any individual who meets the inclusion criteria,* does not have any of the conditions listed as exclusion criteria,<sup>†</sup> and has a score of ≥4 when the weights from the five | |||
criteria items below are summed. | |||
|- | |||
!Item | |||
!Weight or Score | |||
|- | |||
|Labial salivary gland with focal lymphocytic sialadenitis and | |||
focus score of ≥1 foci/4 mm <sup>‡</sup> | |||
|3 | |||
|- | |||
|Anti-SSA/Ro positive | |||
|3 | |||
|- | |||
|Ocular staining score ≥5 (or van Bijsterveld score ≥4) in at | |||
least one eye <sup>§∥</sup> | |||
|1 | |||
|- | |||
|Schirmer test ≤5 mm/5 minutes in at least one eye <sup>§</sup> | |||
|1 | |||
|- | |||
|Unstimulated whole saliva flow rate ≤0.1 mL/min <sup>§§¶ </sup> | |||
|1 | |||
|- | |||
| colspan="2" style="font-size:0.75rem; border-top:solid #a2a9b1 1px!important;"|*These inclusion criteria are applicable to any patient with at least one symptom of ocular or oral | |||
dryness, defined as a positive response to at least one of the following questions: | |||
<ol> | |||
<li>Have you had daily, persistent, troublesome dry eyes for more than 3 months?</li> | |||
<li>Do you have a recurrent sensation of sand or gravel in the eyes?</li> | |||
<li>Do you use tear substitutes more than three times a day?</li> | |||
<li>Have you had a daily feeling of dry mouth for more than 3 months?</li> | |||
<li>Do you frequently drink liquids to aid in swallowing dry food?</li> | |||
</ol> | |||
or in whom there is suspicion of Sjögren syndrome (SS) from the European League Against Rheumatism<br> | |||
SS Disease Activity Index questionnaire (at least one domain with a positive item).<br> | |||
†Exclusion criteria include prior diagnosis of any of the following conditions, which would exclude diagnosis of SS and participation in SS studies or therapeutic trials because of overlapping clinical features or interference with criteria tests: (1) history of head and neck radiation treatment, (2) active hepatitis C infection (with confirmation by PCR), (3) AIDS, (4) sarcoidosis, (5) amyloidosis, (6) graft-versus-host disease, or (7) IgG4-related disease.<br> | |||
‡The histopathologic examination should be performed by a pathologist with expertise in the diagnosis of focal lymphocytic sialadenitis and focus score count using the protocol described by Daniels et al.<ref>Daniels TE, Cox D, Shiboski CH, et al. Associations between salivary gland histopathologic diagnoses | |||
and phenotypic features of Sjogren’s syndrome among 1,726 registry participants. Arthritis Rheum. | |||
2011;63:2021-2130.</ref><br> | |||
§Patients who are normally taking anticholinergic drugs should be evaluated for objective signs of salivary hypofunction and ocular dryness after a sufficient interval without these medications for these components to be a valid measure of oral and ocular dryness.<br> | |||
∥Ocular Staining Score described by Whitcher et al<ref>Whitcher JP, Shiboski CH, Shiboski SC, et al. A simplified quantitative method for assessing keratoconjunctivitis sicca from the Sjogren’s Syndrome International Registry. Am J Ophthalmol. 2010;149:405-415</ref>; van Bijsterveld score described by van Bijsterveld.<ref>Van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol. 1969;82:10-14.</ref><br> | |||
§¶Unstimulated whole saliva flow rate measurement described by Navazesh and Kumar.<ref>avazesh M, Kumar SK, University of Southern California School of Dentistry. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139(suppl):35S-40S.</ref> | |||
|} | |||
== Differential Diagnosis == | |||
{{DDX Box|ddx-title=Differential Diagnosis of SS|ddx-text=*Age-related Sicca Syndrome | |||
*IgG4-related disease | |||
*Eosinophilic sialodochitis | |||
*Benign lymphoepithelial sialadenitis and dacryoadenitis | |||
*Lymphona and other haematologic malignancy | |||
*Sarcoidosis | |||
*Hepatitis C | |||
*HIV | |||
*Graft-versus-host disease | |||
*Sicca induced by immune checkpoint inhibitors | |||
*Systemic vasculitis}}{{DDX Box|ddx-title=Differential Diagnosis of Dry Eye|ddx-text=<strong> Primarily evaporative</strong> | |||
* Eyelid and ocular surface disease | |||
* Meibomian gland dysfunction | |||
* Poor eyelid congruity | |||
* Facial nerve paralysis | |||
* Low blink rate (e.g., Parkinson disease, video terminal use) | |||
* Extrinsic causes that enhance evaporation | |||
** Trachoma (vitamin A deficiency) | |||
** Use of topical anesthetic drops | |||
** Excessive use of preservative-containing drops | |||
** Contact lens wear | |||
** Allergic conjunctivitis | |||
<strong> Primarily aqueous deficient</strong> | |||
* Sjögren syndrome | |||
* Other forms of lacrimal gland disease | |||
* Aging | |||
* Inflammatory diseases (e.g., acquired immunodeficiency syndrome, sarcoidosis, lymphoma, graft-versus-host disease) | |||
* Lacrimal gland duct obstruction from various forms of cicatrizing conjunctivitis | |||
* Ocular sensory loss leading to reflex hyposecretion and a diminished blink rate | |||
* Corneal surgery | |||
* Diabetes mellitus | |||
* Neurotrophic keratitis | |||
* Chronic contact lens wear | |||
* Loss of lacrimal secretory motor function | |||
*Drugs (e.g., antihistamines, beta blockers, antispasmodics, diuretics) | |||
* Central seventh nerve damage}}{{DDX Box|ddx-title=Differential Diagnosis of Xerostomia|ddx-text=*Drug side effect (e.g., single or multiple prescription of drugs with anticholinergic, diuretic, antihypertensive, anxiolytic, or antihistamine effects) | |||
*Salivary gland diseases, including Sjögren syndrome | |||
*Poorly controlled diabetes mellitus | |||
*Dehydration | |||
*Mouth breathing, nasal obstruction | |||
*Head and neck irradiation (including high doses of radioactive iodine for thyroid cancer) | |||
*Psychological factors}}{{DDX Box|ddx-title=Differential Diagnosis of Salivary Gland Enlargmenet|ddx-text=<strong>Infectious</strong> | |||
* Viral infections (mumps, Epstein-Barr virus, hepatitis C, human immunodeficiency) | |||
* Bacterial | |||
* Acute suppurative parotitis | |||
* Tuberculosis | |||
* Fungal | |||
<strong>Autoimmune</strong> | |||
* Sjögren syndrome | |||
* Granulomatous polyangiitis | |||
<strong>Inflammatory</strong> | |||
* IgG4-related disease (including Küttner tumor) | |||
* Allergic parotitis (sialodochitis fibrinosa) | |||
* Chronic recurrent parotitis | |||
* Kimura disease | |||
<strong>Metabolic (causing sialadenosis, which is characterized by painless, bilaterally | |||
symmetric parotid enlargement that is soft and nontender on palpation)</strong> | |||
* Uncontrolled diabetes mellitus | |||
* Bulimia | |||
* Alcoholism with liver disease | |||
* Hyperlipoproteinemia | |||
<strong>Neoplastic</strong> | |||
* Lymphoma | |||
* Leukemia | |||
* Warthin tumor (papillary cystadenoma lymphomatosum) | |||
* Diffuse hyperplastic oncocytic hyperplasia | |||
<strong>Granulomatous</strong> | |||
* Sarcoidosis | |||
<strong>Iatrogenic or self-induced</strong> | |||
* Radioactive iodine | |||
* Pneumoparotitis (wind instrument players, glass blowers)}} | |||
== Management == | |||
Management is similar for primary and secondary SS | |||
=== General Measures === | |||
For mild SS without extraglandular disease systemic therapy is not usually required. Secretagogues plus local therapy for ocular and oral symptoms can be used such as artificial tears. | |||
[[Smoking and Chronic Pain|Smoking]] increases the risk of dental decay and other oral complications as well as reduces the efficacy of medications such as hydroxychloroquine. It also aggravates small airway disease. Medications that exacerbate drying side effects should be avoided. | |||
Pregnancy counseling should be provided. The most serious adverse fetal outcome in SS is congenital heart block. Other complications are more common such as fetal loss, IUGR, and premature deliver. | |||
Patietns are at increased risk of complications from surgery requiring general anaesthesia. Anticholinergic drugs and the low-humidity environment of the operating theatre predisposes to ocular surface, mucosal, and dental damage. There is increased risk of atelectasis. | |||
=== Pharmacologic === | |||
Pilocarpine and cevimeline are examples of muscarinic agonists used as secretagogues. | |||
For moderate to severe disease systemic therapy is usually used. The approach is similar to SLE and [[Rheumatoid Arthritis|RA]]. Systemic therapy options include glucocorticoids, hydroxychloroquine, methotrexate, leflunomide, azathioprine, sulfasalazine, mycophenolate, cyclosporine, cyclophosphamide, and rituximab. | |||
== References == | |||
[[Category:Rheumatology]] | [[Category:Rheumatology]] | ||
{{References}} | |||
{{Reliable sources}} | |||
Latest revision as of 18:34, 12 March 2023
Sjögren's syndrome (SS) is a chronic autoimmune disease that is characterised by lymphocytic infiltration of the salivary, lacrimal, and other exocrine glands leading to dry eyes and dry mouth along with autoantibodies. It can also result in skin disease, arthritis, nephritis, cytopaenia, pneumonitis, vasculitis, peripheral neuropathy, myelopathy, and cognitive dysfunction. The clinical features are divided into exocrine glandular features and extraglandular features.
Definitions
- Sjogren's disease - synonym for SS
- Sicca syndrome - synonym for SS
- Sicca complex - dryness of the eyes and mouth. Doesn't specify autoimmunity
- Keratoconjunctivitis sicca (KCS) - ocular findings of SS
- Dry eye syndrome (DES) - can be due to conditions such as SS and meibomian gland dysfunction. Only 10% of patients have SS.
- Mikulicz syndrome - parotid and lacrimal gland enlargement from any cause. Including SS or other conditions such as IgG4 related disease.
Epidemiology
SS is most common in women, the female to male ratio often exceeds 10:1. It usually is diagnosed between 40-60 but it can occur in younger and older individuals as well.[1] The overall prevalence is estimated at 43 per 100,000 people (0.043%).[2] Dry eye and mouth occurs in up to 30% of older adults. This can be due to medication side effects and age-related atrophy of gland tissue.
Pathogenesis
The pathogenesis is one of targeted inflammation of the lacrimal and salivary glands with B-lymphocyte hyperactivity.[1]
Both genetic and non-genetic factors are thought to be involved. It is thought that SS occurs following an environmental trigger, likely viral (but no single virus has been implicated), in a genetically susceptible individual. The immune response involves both innate and adaptive immunity leading to autoimmunity and chronic inflammation. There is a cycle of mutual stimulation of the innate and acquired immune systems resulting in glandular injury.
The pathologic lesion is a lymphocytic infiltration of affected organs. The most frequently affected tissues are the lacrimal and salivary glands whereby there is focal aggregation of lymphocytes that start around the ducts and spread to the entire lobule. Infiltrates can also occur in extraglandular sites. Other mechanisms contribute to glandular dysfunction including antibodies to the muscarinic receptors that impair neural innervation of the gland as well as deleterious effects of cytokines on neurotransmitter release.
Specific autoantibodies are found in SS, particularly anti-Ro/SSA and anti-La/SSB in 60-80% of individuals. ANA antibodies are positive in around 90% of patients. High RF factor is also common. Autoantibodies can be found many years before the onset of SS. Autoantibodies alone are not sufficient for disease induction.
Clinical Presentation
SS occurs on a spectrum with a range of presentations. Symptoms can include fatigue, arthralgia, polyarthritis, renal, neurologic, cutaneous, endocrine, hepatic, vasculitis, pulmonary, and haematologic manifestations.
On the mild to moderate side, patients have dry eyes and mouth along with fatigue, cognitive dysfunction, and myalgia. The diagnosis is confirmed by positive antibodies and/or gland biopsy. Without laboratory or histological studies the presentation may be identical to fibromyalgia or even patients with depression who have anticholinergic side effects from medication.
On the severe end patients may have frank salivary gland swelling and adenopathy. There may be cryoglobulinaemia, low complement, Hodgkin lymphoma, and extraglandular disease. Antibodies may again be positive.
In a minority of patients there is primary extraglandular involvement with limited eye or mouth symptoms. The diagnosis may be made, e.g. with positive antibodies, during workup of neuropathies, nephropathies, interstitial pneumonitis, or haematologic abnormalities.
Diagnosis
There is no single test. The diagnosis is made with having both objective clinical and laboratory features, following exclusion of other causes. The diagnosis can't be made with the presence of autoantibodies and no compatible symptoms.
Objective clinical findings of mouth or eye dryness: this includes one of abnormal Schirmer test of either eye, abnormal sialometry or Saxon test for the glands, or radiological evidence such as on MRI, CT, or US.
Serological or histological findings: Anti-Ro/SSA +/- Anti-La antibodies or positive labial salivary gland biopsy showing focal lymphocytic sialednitis. In the presence of isolated anti-La antibodies, biopsy is required to confirm the diagnosis. A diagnosis of secondary SS can be made without antibodies or biopsy in the presence of a well-established systemic rheumatological disease such as SLE or RA. Also acceptable are positive anticentromere antibodies without systemic sclerosis or findings of ANA greater or equal to 1:320 along with positive RF.
In individuals with isolated extraglandular disease, the diagnosis can be made with positive biopsy and anti-Ro antibodies.
| The classification of primary Sjögren syndrome applies to any individual who meets the inclusion criteria,* does not have any of the conditions listed as exclusion criteria,† and has a score of ≥4 when the weights from the five
criteria items below are summed. | |
| Item | Weight or Score |
|---|---|
| Labial salivary gland with focal lymphocytic sialadenitis and
focus score of ≥1 foci/4 mm ‡ |
3 |
| Anti-SSA/Ro positive | 3 |
| Ocular staining score ≥5 (or van Bijsterveld score ≥4) in at
least one eye §∥ |
1 |
| Schirmer test ≤5 mm/5 minutes in at least one eye § | 1 |
| Unstimulated whole saliva flow rate ≤0.1 mL/min §§¶ | 1 |
| *These inclusion criteria are applicable to any patient with at least one symptom of ocular or oral
dryness, defined as a positive response to at least one of the following questions:
or in whom there is suspicion of Sjögren syndrome (SS) from the European League Against Rheumatism | |
Differential Diagnosis
- Age-related Sicca Syndrome
- IgG4-related disease
- Eosinophilic sialodochitis
- Benign lymphoepithelial sialadenitis and dacryoadenitis
- Lymphona and other haematologic malignancy
- Sarcoidosis
- Hepatitis C
- HIV
- Graft-versus-host disease
- Sicca induced by immune checkpoint inhibitors
- Systemic vasculitis
Primarily evaporative
- Eyelid and ocular surface disease
- Meibomian gland dysfunction
- Poor eyelid congruity
- Facial nerve paralysis
- Low blink rate (e.g., Parkinson disease, video terminal use)
- Extrinsic causes that enhance evaporation
- Trachoma (vitamin A deficiency)
- Use of topical anesthetic drops
- Excessive use of preservative-containing drops
- Contact lens wear
- Allergic conjunctivitis
Primarily aqueous deficient
- Sjögren syndrome
- Other forms of lacrimal gland disease
- Aging
- Inflammatory diseases (e.g., acquired immunodeficiency syndrome, sarcoidosis, lymphoma, graft-versus-host disease)
- Lacrimal gland duct obstruction from various forms of cicatrizing conjunctivitis
- Ocular sensory loss leading to reflex hyposecretion and a diminished blink rate
- Corneal surgery
- Diabetes mellitus
- Neurotrophic keratitis
- Chronic contact lens wear
- Loss of lacrimal secretory motor function
- Drugs (e.g., antihistamines, beta blockers, antispasmodics, diuretics)
- Central seventh nerve damage
- Drug side effect (e.g., single or multiple prescription of drugs with anticholinergic, diuretic, antihypertensive, anxiolytic, or antihistamine effects)
- Salivary gland diseases, including Sjögren syndrome
- Poorly controlled diabetes mellitus
- Dehydration
- Mouth breathing, nasal obstruction
- Head and neck irradiation (including high doses of radioactive iodine for thyroid cancer)
- Psychological factors
Infectious
- Viral infections (mumps, Epstein-Barr virus, hepatitis C, human immunodeficiency)
- Bacterial
- Acute suppurative parotitis
- Tuberculosis
- Fungal
Autoimmune
- Sjögren syndrome
- Granulomatous polyangiitis
Inflammatory
- IgG4-related disease (including Küttner tumor)
- Allergic parotitis (sialodochitis fibrinosa)
- Chronic recurrent parotitis
- Kimura disease
Metabolic (causing sialadenosis, which is characterized by painless, bilaterally symmetric parotid enlargement that is soft and nontender on palpation)
- Uncontrolled diabetes mellitus
- Bulimia
- Alcoholism with liver disease
- Hyperlipoproteinemia
Neoplastic
- Lymphoma
- Leukemia
- Warthin tumor (papillary cystadenoma lymphomatosum)
- Diffuse hyperplastic oncocytic hyperplasia
Granulomatous
- Sarcoidosis
Iatrogenic or self-induced
- Radioactive iodine
- Pneumoparotitis (wind instrument players, glass blowers)
Management
Management is similar for primary and secondary SS
General Measures
For mild SS without extraglandular disease systemic therapy is not usually required. Secretagogues plus local therapy for ocular and oral symptoms can be used such as artificial tears.
Smoking increases the risk of dental decay and other oral complications as well as reduces the efficacy of medications such as hydroxychloroquine. It also aggravates small airway disease. Medications that exacerbate drying side effects should be avoided.
Pregnancy counseling should be provided. The most serious adverse fetal outcome in SS is congenital heart block. Other complications are more common such as fetal loss, IUGR, and premature deliver.
Patietns are at increased risk of complications from surgery requiring general anaesthesia. Anticholinergic drugs and the low-humidity environment of the operating theatre predisposes to ocular surface, mucosal, and dental damage. There is increased risk of atelectasis.
Pharmacologic
Pilocarpine and cevimeline are examples of muscarinic agonists used as secretagogues.
For moderate to severe disease systemic therapy is usually used. The approach is similar to SLE and RA. Systemic therapy options include glucocorticoids, hydroxychloroquine, methotrexate, leflunomide, azathioprine, sulfasalazine, mycophenolate, cyclosporine, cyclophosphamide, and rituximab.
References
- ↑ 1.0 1.1 Hochberg. Sjogren syndrome (chapter 147) In: Rheumatology. 2019
- ↑ Qin, Baodong; Wang, Jiaqi; Yang, Zaixing; Yang, Min; Ma, Ning; Huang, Fenglou; Zhong, Renqian (2015-11). "Epidemiology of primary Sjögren's syndrome: a systematic review and meta-analysis". Annals of the Rheumatic Diseases. 74 (11): 1983–1989. doi:10.1136/annrheumdis-2014-205375. ISSN 1468-2060. PMID 24938285. Check date values in:
|date=(help) - ↑ Shiboski CH, Shiboski SC, Seror R, et al; International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism Classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheum. 2017;69(1):35-45.
- ↑ Daniels TE, Cox D, Shiboski CH, et al. Associations between salivary gland histopathologic diagnoses and phenotypic features of Sjogren’s syndrome among 1,726 registry participants. Arthritis Rheum. 2011;63:2021-2130.
- ↑ Whitcher JP, Shiboski CH, Shiboski SC, et al. A simplified quantitative method for assessing keratoconjunctivitis sicca from the Sjogren’s Syndrome International Registry. Am J Ophthalmol. 2010;149:405-415
- ↑ Van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol. 1969;82:10-14.
- ↑ avazesh M, Kumar SK, University of Southern California School of Dentistry. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139(suppl):35S-40S.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,