Spinal Cord Anatomy
The spinal cord starts below the foramen magnum, and ends at the tip of the conus medullaris. It ends between the T12 to L2-3 disc level, typically around L1 or the L1-2 disc. It is contained within the thecal sac. The spinal cord has a tubular shape. On cross section it is elliptical in the cervical region, and round in the thoracic region. There are two enlargements at the areas of limb innervation - the cervical enlargement at C5-T1 for upper limb innervation, and a smaller lumbar enlargement at T9-L2 for lower limb and pelvis innervation. There are 31 spinal segments along the spinal cord. These are the 8 cervical, 12 thoracic, five lumbar, five sacral, and one coccygeal segments. The filum terminalis is a thin band of connective tissue that extends from the tip of the conus medullaris down to the first coccygeal segment through the caudal end of the thecal sac.[1]
This article is a general overview of spinal cord anatomy. See nociception and basic neurophysiology for a more detailed overview on neurophysiology.
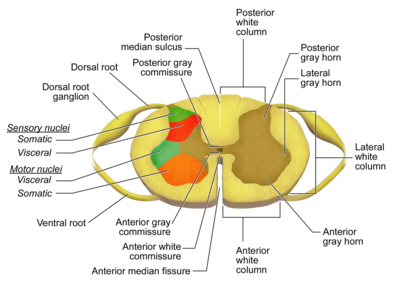
Fissures and Sulci
A deep ventral median fissure and a shallower dorsal median sulcus and septum posteriorly divides the spinal cord into right and left halves that are almost completely separated. Dorsal nerve roots travel to the cord on the posterior surface of the cord through the dorsolateral sulci. Ventral nerve roots travel from the anterior surface of the cord through the ventrolateral sulci. The topography of the cord surface can be visualised by axial T2 weighted gradient echo MRI sequences and CT myelograms.[1]
Grey Matter
Unlike the brain where the grey matter is located peripherally, the spinal cord has its grey matter centrally and is H- or butterfly-shaped. On MRI the grey matter is hyperintense on T2, and hypointense on T1. The peripheral white matter columns are hyperintense to grey on T1. The grey matter has ventral and dorsal horns that run along the length of the cord. There are also small lateral horns from around T1-L1. The dorsal horns receive primary afferent fibres from the dorsal roots of the spinal nerves and are primarily involved in sensory processing. The ventral horns transmit motor neurons. The lateral horns have autonomic nuclei and interneurons. Connecting the two arms of the H around the central canal are the ventral and dorsal gray matter commissures that run horizontally. The central canal is located between the ventral one-third and dorsal two-thirds in the cervical and thoracic region, and is more central in the lumbar region. On MRI it is a thin with a non-enhancing fluid signal.[1]
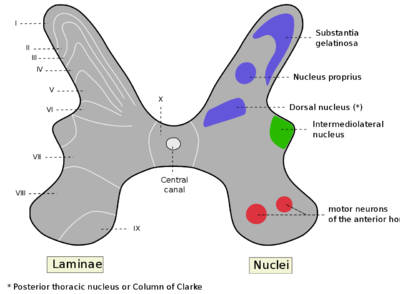
There are ten layers of grey matter classified as laminae I through X called the Laminae of Rexed. Fibres that carry specific types of information follow distinct pathways. Pain and noxious stimuli mostly terminate in Laminae I and II. Touch information terminates in Laminae IV or on the processes of cells in Laminae V. Stretch receptors from muscle spindles and tendon organs terminate in parts of Laminae V, VI, VII, and so on.
| Lamina | Nucleus | First Neuron | Second Neuron | Function |
|---|---|---|---|---|
| Dorsal Column | ||||
| I | Marginal zone | Aδ, C | NS, WDR | Noxious or thermal stimuli, sends information via the lateral spinothalamic tract |
| II | Substantia gelatinosa of Rolando | C, Aδ | NS, WDR | Sensory-related stimuli (noxious and non-noxious), and moderates the sensation of pain. Location of Lissauer tract. |
| III | Nucleus proprius | Aβ, Aδ, C | LTM | Proprioception and light touch sense |
| IV | Nucleus proprius | Aβ, Aδ | NS, WDR | Non-noxious stimuli information and processing |
| V | Nucleus proprius is upper part. Neck of the dorsal horn | Aβ, Aδ, (C) | WDR, NS | Afferent cutaneous, muscle and joint mechanical nociceptors as well as visceral nociceptors. Travels to the brain via the lateral spinothalamic tracts. Also receives descending information via the corticospinal and rubrospinal tracts. The Lamina has wide dynamic range tract neurons, interneurons and propriospinal neurons. Viscerosomatic pain signal convergence often occurs in this lamina due to the presence of wide dynamic range tract neurons resulting in pain referral. |
| VI | Base of the dorsal horn | Aβ | WDR | Interneurons involved in the modulation of spinal reflexes and reception of sensory information from muscle spindles that are involved with proprioception. Information travels to the brain through the ipsilateral spinocerebellar pathways where it can modulate muscle tone accordingly. Only present in the cervical and lumbosacral enlargements. |
| Lateral Column | ||||
| VII | intermediomedial nucleus, intermediolateral nucleus, posterior thoracic nucleus in the thoracic and upper lumbar region | Visceral information, function and regulation of the autonomic nervous system. | ||
| VIII | motor interneurons; Commissural nucleus | Aβ | Involved in modulation of motor output to skeletal muscles. Changes in configuration depending on the segmental level. Most prominent in cervical and lumbar levels. | |
| IX | Aβ | Clusters of large alpha motor neurons (striated muscles), and small gamma motor neurons (muscle spindles). Configuration changes depending on the segmental level. | ||
| Central Canal | ||||
| X | Spinal cord nucleus | Aβ, (Aδ) | NS | Central area of grey matter surrounding the central canal. Known as the grey commissure, where axons decussate. |
| NS: Nociceptive-specific, WDR: Wide-dynamic range, LTM: Low-threshold mechanosensitive | ||||
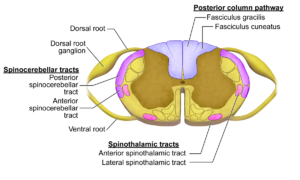
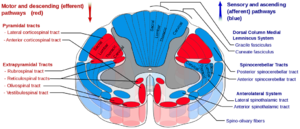
White Matter
The white matter contains three columns otherwise known as funiculi. They are the ventral (anterior), lateral, and dorsal (posterior) columns. They contain nerve axon bundles making up the neural pathways. The ventral columns are located between the ventral median fissure and ventral nerve roots. The lateral columns are between the ventrolateral and dorsolateral sulci in the location of where the ventral nerve roots exit and the dorsal nerve roots enter the cord. The dorsal columns are between the dorsal median sulcus and dorsolateral sulci on each side. Through these columns travel the ascending sensory and descending motor pathways. The most well known columns are the corticospinal tract, the dorsal columns, and the spinothalamic tract.[1]
Descending Pathways
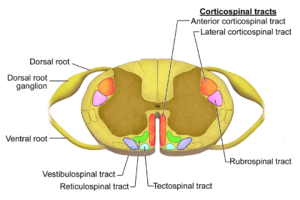
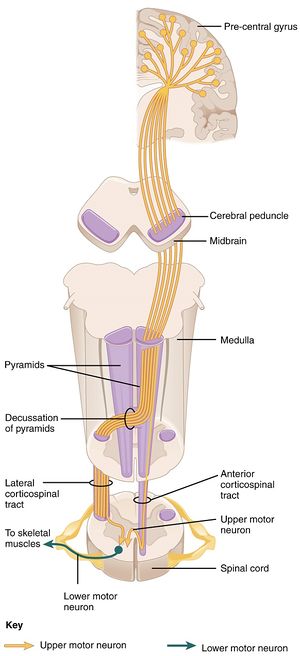
Corticospinal Tract
The corticospinal tract contains descending motor axons that control fine movements and the most important motor pathways. The axons are from upper motor neurons. More than 50% of these stem from the primary motor cortex, and the remainder come from the premotor cortex, supplementary motor area, and sensory cortex. From the brain they travel through the cerebral white matter, posterior limb of the internal capsule, cerebral peduncle, and the ventral pons. In the medulla, 75-90% of the nerve fibres decussate in the pyramid and then travel caudally becoming the lateral corticospinal tract in the lateral column. These lateral corticospinal tract neurons synapse in the ventral horn and then exit the spinal cord. The remaining axons that don't decussate, travel caudally as the anterior corticospinal tract. These fibres cross over to the contralateral side in each spinal cord segment, and supply motor neurons in the ventral horn.[1]
Injury to neurons in the motor cortex and corticospinal tract manifests as upper motor neuron deficits. While injury to the neurons in the ventral horns and peripheral nerves manifests as lower motor neuron deficits. There is a laminar somatotopic arrangement of axons that is similar in the corticospinal and spinothalamic tracts. Cervical and thoracic axons innervating the upper limbs and thorax are found medially. Lumbar and sacral axons innervating the abdomen and lower extremities are found laterally. This is why injury to the central spinal cord first affects the upper extremities.[1]
| Feature | UMN Deficit | LMN Deficit |
|---|---|---|
| Lesion location | Proximal to anterior horn (motor cortex, brainstem, spinal cord) | Anterior horn cell or distal to anterior horn cell (root, plexus, peripheral nerve) |
| Muscle tone | Increased (spastic paresis) | Decreased (flaccid paralysis) |
| Muscle bulk | Maintained or mildly atrophic | Severely atrophic |
| Weakness | In legs, greater in flexors than in extensors; in arms, greater in extensors than in flexors, producing a pyramidal pattern of weakness | Depends on location: uniform spinal cord weakness in all muscle groups of the segment; peripheral nerve weakness of specific muscle groups |
| Reflexes | Increased | Areflexia |
| Babinski sign | Positive: upgoing plantar response | Negative |
| Fasciculations | No | Yes |
Ascending Pathways
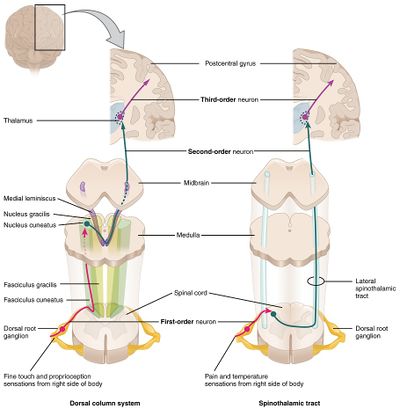
Dorsal Columns
The dorsal column is the location of the tracts carrying information for proprioception, vibration sense, and fine-touch sensation. There are two large ascending tracts, the medial fasciculus gracilis, and the lateral fasciculus cuneatus. The fasciculus gracilis starts at the distal cord and contains fibres that carry sensory input from the lower extremities and lower trunk, i.e. the medial sacral and lumbar fibres. The fasciculus cuneatus starts in the thoracic region and contains fibres that carry sensory input from the upper extremities and upper trunk, i.e. the lateral thoracic and cervical fibres. Fibres in the dorsal column first receive input from the dorsal root ganglion, and the travel proximally ipsilaterally. They then synapse in their relevant nuclei (gracilis or cuneatus) and decussate in the medulla. After decussation the fibres of the dorsal column form the medial lemniscus, ascend through the brainstem, and synapse in the ventral posterior nucleus of the thalamus. They tend finally terminate in the primary somatosensory cortex of the postcentral gyrus.
Like the corticospinal tracts, the fibres of the dorsal columns have a somatotopic arrangement. The arrangement from medial to lateral is sacral, lumbar, thoracic, and cervical.[1]
Spinothalamic Tract
The spinothalamic tract transmits information regarding pain, temperature, and crude touch. Small-diameter unmyelinated axons from the dorsal root ganglion that carry pain, temperature, and crude touch sensation information enter the cord and synapse immediately in the dorsal horn. Second order neurons are located in the dorsal horn and carry pain and temperature sense. They cross over at the anterior spinal commissure and ascend the spinothalamic tract in the contralateral anterolateral white matter.[1]
The spinothalamic tract is the only tract that decussates at the spinal cord level. The crossing fibres ascend at least two to three spinal segments before reaching the contralateral side. Clinically this means that injury to the spinothalamic tract manifests as contralateral loss of pain and temperature sense that starts a few segmetns below the level of the lesion. The somatotopic organisation of fibres in the spinothalamic tract from medial to lateral is cervical, thoracic, lumbar, and sacral. This is opposite the dorsal column arrangement.[1]
Spinal Cord Blood Supply
The spinal cord has its vascular supply supplied by a single anterior spinal artery and a pair of posterior spinal arteries. The anterior spinal artery is formed from the branches of the vertebral artery. The posterior spinal arteries are formed from either the posterior inferior cerebellar artery or vertebral arteries. The anterior spinal artery travels in the ventral midline sulcus of the spinal cord. The posterior spinal arteries travel along the right and left dorsolateral sulci. There is a plexus formed from both vessels that surrounds the cord. There are reinforcing medullary branches from the posteroinferior cerebellar, vertebral, deep cervical, intercostal, and lumbar arteries.[1]
The primary blood supply to the lumbar and sacral cord segments is the artery of Adamkiewicz. This artery typically arises from the left side of the aorta between T9 and L2. There is often a hairpin loop before it joins the anterior spinal artery.[1]
The anterior spinal artery supplies the anterior two thirds of the spinal cord, while the posterior cerebral arteries supply the posterior one third. There are watershed regions typically located around the middle to lower thoracic cord. Hypoperfusion states for example cardiac aortic surgery can lead to ischaemia in these areas.[1]
Videos
See Also
- Incomplete Cord Syndromes
- Basic Neurophysiology
- Noted Anatomist, detailed videos on spinal cord anatomy
References
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,