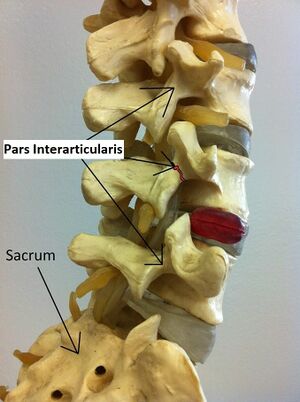
Spondylolysis
Spondylolysis, also known as a pars defect, is a unilateral or bilateral fracture in the pars interarticularis of a vertebra. It typically affects the L4 or L5 vertebra. With bilateral defects the vertebral body can slide anteriorly in a condition called spondylolisthesis.
Anatomy
The function of the pars interarticularis is to transmit forces from the inferior articular process and the spinous process to the pedicle and vertebral body. It helps to resist anterior translation, torsion, and flexion of the intervertebral joint.
Pathophysiology
When the lumbar spine flexes there is more stress on the disc, and with extension there is more stress on the facet joints. Compound extension plus rotation increases this stress, leading to stress fracture.
The pars interarticularis is the thinnest part of the vertebra and in many people is only thick enough to withstand average loads of daily living, with higher loads leading to fracture. It is susceptible to fatigue fracture with repeated loads in compression or axial rotation and this is the most common mechanism of fracture. However it can also fracture following a single acute overload.
The defect runs obliquely from the superior border to the lateral border of the lamina. Sometimes it extends into the pedicle or lamina. It is generally located between the capsules of the above and below zygapophysial joints, and so can appear to communicate with these joints on arthrography. Bony stability is lost, but if the ligaments are functional they compensate adequately.
Without full bony healing, the defect is filled with fibrous tissue, i.e. a non-bony fibrous union. The fibrous tissue contains nerve fibres and free nerve endings, and so is anatomically capable of producing pain.
Spondylolysis is an acquired fracture. It was previously thought to be congenital but this was proven to be incorrect through multiple avenues of evidence: it doesn't occur in infants, the prevalence increases with age, the prevalence is associated with certain activities, it doesn't occur in non-ambulatory individuals, osseous debris fills the defect, and the lamina only has one ossification centre.[1]
In individuals where the defect is the cause of pain, the possible mechanisms of pain are movement of the lamina straining the fibrous tissue of the defect, and in cases of bilateral defects there may be a flail lamina which can distort the associated zygapophysial joint.[1]
Epidemiology
The overall prevalence is around 6%.[2] It is particularly common in sports people who do twisting movements or compound twisting with flexion or extension. Fast cricket bowlers are the classically affected group, but they are more common in multiple different sports such as gymnastics, dancing, diving, weightlifting, figure skating, volleyball, soccer, and racquet sports.
The L5 vertebral is the most commonly affected in 85-95% of cases, and L4 is the second most common in 5-15% of cases. It can rarely affect levels as high as L1.[2] It is bilateral in 80% of cases, and is in multiple levels in 4% of cases.
It usually presents in early adolescence. Initial studies showed a male predilection, but now with greater female involvement in sport there is a near equal prevalence in some but not all studies
Around 50-81% of individuals with spondylolysis have associated spondylolisthesis.[2]
Clinical Features and Relationship to Pain
Spondylolysis is equally common in symptomatic and asymptomatic adults. It is thought that in some individuals it may cause pain, but simply identifying the defect on x-ray does not allow one to state that it is the source of their pain (LR is close to 1).[1]
Patients may complain of an aching low back that is exacerbated by hyperextension and relieved by rest, sometimes pain radiation into the buttocks and posterior thighs.[2] Neurological symptoms can occur rarely as the pars forms the posterior roof of the neural foramina.[3]
Examination findings include lumbosacral tenderness, hamstring tightness, and the positive one-legged hyperextension test. The latter test involves standing on one leg and bending backwards looking for pain in the ipsilateral back, but I could not find published data on reliability or validity.[3]
During the adolescent growth spurt there may be progression of spondylolysis to spondylolisthesis, and this may be associated with persistent back pain, flattening of the lumbar lordosis, and the Phalen-Dickson sign which is a knee-flexed/hip-flexed gait.
These features in no way allows differentiation with other sources of mechanical low back pain. There are also no proven features on history or exam that are valid in identifying the defect as the source of pain.[1]
Investigations
An AP and lateral radiograph of the lumbar spine is usually the first study obtained, and detects most fractures, but cannot generally determine their age. The lateral view detects most abnormalities while the AP view detects other abnormalities such as transitional vertebra. The oblique view or "scotty dog" view was the traditionally recommended view but is no longer recommended due to limited sensitivity and greater radiation exposure with it doubling the radiation for little additional information. The fracture line can fall out of plane of the x-ray beam.[4][5]
Some authors say x-rays are not required in the absence of red flag symptoms.[1] In adolescents it may be prudent todo radiographs as back pain is less common and red flag conditions may be more important.
Advanced imaging such as MRI or SPECT are generally second line. However, some authors advocate for MRI to be used early in the diagnostic process.[2]
Imaging does not diagnose the source of pain, it only shows the fracture, which may or may not be painful. The defect can only be confirmed to be a source of pain through local anaesthetic infiltration of the defect, called a pars block.
Treatment
In most cases treatment is conservative with simple analgesia, physical therapy, and time. A short period of rest may be indicated in acute fracture in adolescents. In sportspeople can usually report to full sport in 3 months after a graded increase of activity, looking for being pain-free at each stage of activity increase.
Bony healing is not necessary for a good outcome, and isn't possible in some cases. Many patients have a non-bony fibrous union and have a good functional recovery.
If proven to be a source of chronic pain through a pars block, surgical fusion may be indicated.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Bogduk et al. Imaging In: Management of Acute and Chronic Low Back Pain. Elsevier 2002.
- ↑ 2.0 2.1 2.2 2.3 2.4 Syrmou, E et al. “Spondylolysis: a review and reappraisal.” Hippokratia vol. 14,1 (2010): 17-21. Full Text
- ↑ 3.0 3.1 Pierre A d'Hemecourt. Spondylolysis and spondylolisthesis in child and adolescent athletes: Clinical presentation, imaging, and diagnosis. Uptodate. May 11, 2020.
- ↑ Libson E, Bloom RA, Dinari G. Symptomatic and asymptomatic spondylolysis and spondylolisthesis in young adults. Int Orthop. 1982;6(4):259-61. doi: 10.1007/BF00267148. PMID: 6222997.
- ↑ Saifuddin A, White J, Tucker S, Taylor BA. Orientation of lumbar pars defects: implications for radiological detection and surgical management. J Bone Joint Surg Br. 1998 Mar;80(2):208-11. doi: 10.1302/0301-620x.80b2.8219. PMID: 9546445.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,