Superior Gluteal Nerve Entrapment
| |
| Superior Gluteal Nerve Entrapment | |
|---|---|
| Causes | Usually iatrogenic |
| Clinical Features | Triad of buttock pain, weakness of hip abductors, and tenderness just lateral to the sciatic notch |
The superior gluteal nerve can injured following injection, surgery, or become entraped between the piriformis and gluteus medius. This condition can cause pseudo-sciatica and hip abductor weakness.
Anatomy
The superior gluteal nerve is derived from the posterior branches of the L4-S1 ventral rami. It passes through the sciatic notch above the piriformis muscle., and turns superiorly passing between piriformis and gluteus medius. It is located under the gluteus maximus muscle. It runs with the superior gluteal artery and vein above the gluteus minimus. It innervates the gluteus medius (upper branch), and gluteus minimus and tensor fascia lata muscles (larger inferior branch). It also innervates the superior femoral neck. There are no superficial sensory fibres. The superior gluteal nerve can be as close as 19mm medial to the greater trochanter, and so the "safe" intramuscular injection area may be quite small.[1]
The inferior gluteal nerves on the other hand is derived from the L5-S2 nerve roots and only supplies the gluteus maximus muscle.[2]
Pathophysiology
Injury is most commonly iatrogenic. Direct lateral hip surgery can injury the inferior branches, and anterolateral or anterior hip surgery can injury the branches to the tensor fascia lata. Percutaneous insertion of iliosacral screws can also cause injury.[1] The superior gluteal nerve can be injured by an incorrectly placed intramuscular injection. It can also be compressed by pelvic masses for example colorectal cancer or an iliac artery aneurysm.[2]
The nerve can also be injured following a bending, lifting, or twisting injury, or a fall on the buttock. Forced internal rotation and extension of the leg with mechanical load (e.g. with in a head-on MVA with the knee extended) can also cause injury.[1]
Clinical Features
History
The patients have pain in the lower back and buttock, with a milder pain down the back of the leg extending to the popliteal fossa, or sometimes down to the foot. The pain generally comes on with prolonged sitting (more than 20-30 mins), leaning forward, or twisting to the contralateral side. The pain is worse with standing and walking, and better with short duration of sitting. They may sit with their weight on the contralateral buttock or cross their legs in order to reduce the pressure on the nerve.[1] There may be a deep aching pain, especially in the presence of a pelvic tumour. [2]
Examination
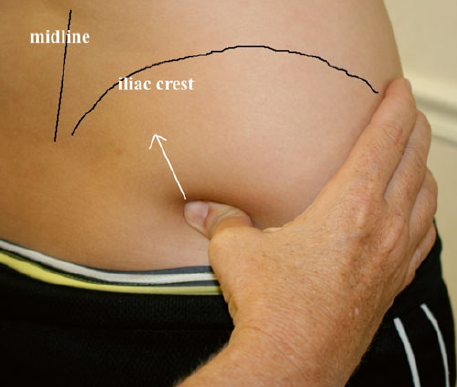
With the patient standing and flexed at the hips, holding onto the exam table, place your hands on the superior edge of the iliac crest. Drop your thumbs to the PSIS, and then laterally to the iliac fossa. Push medially and superiorly between the piriformis and gluteus medius. This is the sciatic notch and location of the superior gluteal nerve. Palpation here should reproduce the pain.[1]
Patients have atrophy and weakness of the gluteus medius, minimus, and tensor fascia lata. This manifests as weakness of hip abduction and external rotation. The patient will have a Trendelenburg gait. They may have difficulty getting out of a chair or climbing stairs. Physical examination findings may be subtle in milder cases. Inferior gluteal nerve injury by contrast, only results of atrophy of the gluteus maximus, manifesting as weakness of leg extension.[2][1]
There isn't usually any sensory change, unless there is additional injury to the posterior femoral cutaneous nerve.[2]
Investigations
Electrophysiology studies may be helpful.[2]
The superior gluteal nerve can sometimes be seen on MRI on coronal and sagittal sequences at the site where it exits the suprapiriformis foramen.[1]
Differential Diagnosis
Sacroiliac pathology is the main differential. A distinguishing features is that in sacroiliac pathology there is tenderness medial to the PSIS, while in superior gluteal nerve pathology there is tenderness more laterally in the iliac fossa.[1]
Myofascial pain is in the differential, but with careful palpation there is usually tenderness between the two muscles of gluteus medius and piriformis.[1]
- Lumbar spine disorders
- Sacroiliac pathology
- Piriformis or gluteus medius spasm
- Sciatic entrapment
- Hip Osteoarthritis
- Maigne syndrome/Thoracolumbar syndrome or Superior Cluneal Nerve Entrapment
- Middle Cluneal Nerve Entrapment
- Posterior Femoral Cutaneous Nerve Entrapment
Diagnosis
Triad of buttock pain, weakness of hip abductors, and tenderness just lateral to the sciatic notch.[1]
Treatment
Injections
For landmark guided injection, position the patient standing, flexed at the hips, and holding on the the exam table. Straddle the injection site with two fingers and advance the needle in a caudal to cranial, lateral to medial direct. Advance the needle to the periosteum.[1]
There are no documented ultrasound guided injection techniques but the superior gluteal artery and piriformis muscle can be seen with ultrasound.[1]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Trescot, Andrea. Peripheral nerve entrapments : clinical diagnosis and management. Switzerland: Springer, 2016.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Craig. Entrapment neuropathies of the lower extremity. PM & R : the journal of injury, function, and rehabilitation 2013. 5:S31-40. PMID: 23542774. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,


