Synovial Joint: Difference between revisions
(Redirected page to Synovial Joints) Tag: New redirect |
(Removed redirect to Synovial Joints) Tag: Removed redirect |
||
| Line 1: | Line 1: | ||
# | {{Curriculum}}{{partial}} | ||
[[File:Synovial joint.jpg|thumb|A synovial joint without a meniscoid.]] | |||
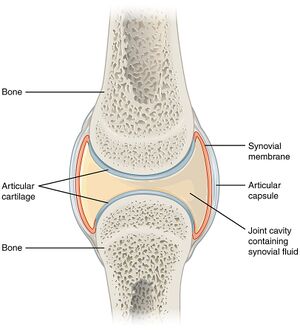
The cardinal feature of a synovial joint is that it is capable of substantial movement, such as with sliding in bending. This is in contrast to fibrocartilaginous and cartilaginous joints where the amplitude of movement is significantly lower. | |||
== Overview of Synovial Joint Structure == | |||
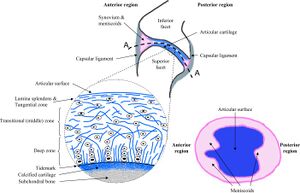
[[File:Facet joint components.jpg|thumb|Facet joint structure, magnified view of the articular cartilage, and cut-through view through the joint. Copyright © 2011 by ASME<ref>Jaumard, Nicolas V et al. “Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions.” Journal of biomechanical engineering vol. 133,7 (2011): 071010. doi:10.1115/1.4004493</ref>]] | |||
'''Joint Space''': There must be some form of ''space'' between the two bones which allows the synovial joint to move. The space is quite narrow. The bones may be shaped in such a way to allow certain movements. For example flat surfaces allow sliding. | |||
'''Cartilage''': The most common effect that occurs at the joint is compression. When muscles act on the joint to move the joint they also exert a compression load across the joint space. The two bones are therefore subjected to phasic (intermittent) compression. Bones on their own are not well designed for phasic loads, but rather are better suited towards static loads. To protect against intermittent compression forces, the joint surfaces are lined with cartilage which provides a cushion or buffer. Cartilage is softer and somewhat more resilient than bone and can dissipate compression forces. | |||
'''Synovial Fluid''': A second hazard is friction. With movement in a gliding fashion, there is friction, which could result in stripping of the cartilage layers. To protect against friction the joint contains synovial fluid. This allows gliding movements between the joint surfaces. The synovial fluid layer is only one molecule thick, which is enough to provide the required anti-friction effects. | |||
'''Synovial Membrane''': The next design issue is that the synovial fluid has to be contained within the joint space and maintained at a suitable quality. Synovial membrane provides these functions. This structure is a sleeve of tissue that surrounds the joint space peripherally, and encloses the space in a thin membrane. The cells of the synovial membrane maintain the quality of the synovial fluid by removing debris and recycling used components back into the bloodstream. | |||
'''Synovial Membrane Blood Vessels''': The blood vessels located on the outer aspect of the synovial membrane have the role of synovial fluid production. Water and protein passes from the blood vessels, across the synovial membrane, and into the joint space. Various cells within the synovial membrane modify the synovial fluid to give the required structure. | |||
'''Joint Capsule''': The synovial membrane is delicate and is easily torn. It is supported on its outer surface by a joint capsule. This is relatively strong fibrous tissue that surrounds the joint space as another sleeve. The synovial membrane extends from the edge of the articular cartilage of one bone to the edge of the articular cartilage of the opposing bone. The capsule attaches further up along the neck of the two opposing bones. The main role of the capsule is protection of the synovial membrane, but also provides some mechanical stability. | |||
'''Inclusions''': Synovial joints can have intra-articular inclusions. A fibro-adipose meniscoid is a washer-like extension of the synovial membrane and capsule that extends into the joint cavity. The meniscoid has fatty tissue, with loose collagen and blood vessels at its core, coated by an extension of the synovial membrane. The function of the meniscoid is to subdivide the joint into two cavities. This results in lubricating fluid being present within each compartment. | |||
Meniscoids are very common, and tend to be found in joints that have substantial sliding movements. During sliding the joint essentially subluxes, and there is unopposed cartilage. The meniscoid leaves the joint cavity and maintains the lubricating layer on the unopposed cartilage. When the joint returns to its neutral position, it does so with the joint surfaces having their lubricating layer being kept in place., and the meniscoid then re-enters the joint cavity. | |||
'''Ligaments''': The joint can be reinforced externally by ligaments. Ligaments may blend with the outer surface of the capsule, or stand alone leaving a space between the deep surface of the ligament and the capsule. Ligaments aren't an essential component of synovial joints, but are a common feature. The function of ligaments are to stabilise the joint against undesired movements. | |||
'''Blood Vessels, Lymphatics, Nerves''': The tissues of the joints have a blood supply with an arterial and venous supply. Lymphatic vessels drain excess fluid from the joint or synovial space. A nerve supply endows the joint and ligaments which monitor position and provide an alerting mechanism against threatened damage if there is excessive strain. | |||
== Articular Cartilage == | |||
Articular cartilage is a tissue that can resist, absorb, dissipate, and transmit ''intermittent'' compression. This is in contrast to bone which is better at resisting static compression. The cartilage retains its form and remains available for the next phase of compression. It also provides a smooth surface over which a joint can glide. | |||
Articular cartilage is on average 2 to 4mm thick (retropatellar up to 7 to 8mm), and it doesn't have blood vessels, nerves, or lymphatics. | |||
=== Zonal Regions === | |||
[[File:Articular cartilage zones.jpg|thumb|Schematic, cross-sectional diagram of healthy articular cartilage: cellular organization in the zones of articular cartilage]] | |||
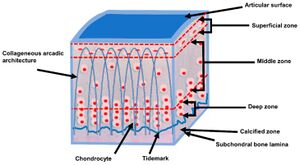
There are different classification systems to describe the four layers within articular cartilage. At the bottom of the deep layer is the tidemark. The tidemark is the boundary between uncalcified matrix above and calcified matrix below. | |||
* Numerical system: identifies layers from I to IV from superficial to deep. | |||
* Topographical system: identifies layers as superficial, middle, deep, and calcified layers. The calcified layer has received a deposit of calcium and is trying to transform into bone like the subchondral bone underlying it. | |||
* Cellular orientation system: identifies layers as tangential in the superficial layer because they run tangential to the surface, transitional in the middle layer because they are clumped and scattered, and radial in the deep layer because they are arranged in radial columns. The fourth layer is again called calcified. | |||
{| class="wikitable" | |||
|+Zonal regions of articular cartilage<ref name=":0">Eschweiler J, Horn N, Rath B, Betsch M, Baroncini A, Tingart M, Migliorini F. The Biomechanics of Cartilage-An Overview. Life (Basel). 2021 Apr 1;11(4):302. doi: 10.3390/life11040302. PMID: 33915881; PMCID: PMC8065530.</ref> | |||
!Zone | |||
!Name | |||
!Description | |||
!Functional Behaviour | |||
|- | |||
|Zone I | |||
|superficial (tangential) zone | |||
|10% to 20% of AC thickness. The collagen fibres of this zone are packed tightly and aligned parallel to the articular surface. The chondrocytes in the superficial zone are flatter and smaller and generally have a greater density than that of the cells deeper in the matrix. It protects deeper layers from shear stresses. The zona superficialis has most of the water and very little proteoglycans. In general, the cells are not very active, which means that there is little wear and tear. The zone can also be used as a barrier against large molecules, for example antibodies | |||
|Responsible for the behaviour of the cartilage under stress. It deforms more strongly and is therefore less rigid than the underlying zones. If this zone is disturbed tissue permeability increases, leading to greater fluid exchange of the cartilage with its surroundings and during compression, this leads to greater mechanical stress on the macromolecular network. The cells here also produce lubricin. | |||
|- | |||
|Zone II | |||
|middle (transitional) zone | |||
|40% to 60% of the total AC volume, and it contains proteoglycans and thicker collagen fibrils. In this layer, the collagen is organized obliquely. Chondrocytes are spherical and at low density | |||
|First line of resistance against compressive forces. The upper aspect produces lubricin. | |||
|- | |||
|Zone III | |||
|deep (radial) zone | |||
|Approximately 30% of the AC volume. The deep zone contains the largest diameter collagen fibrils in a radial disposition, the highest proteoglycan content, and the lowest water concentration. The chondrocytes are typically arranged in a columnar orientation, parallel to the collagen fibers and perpendicular to the joint line. | |||
|Responsible for providing the greatest resistance to compressive forces, given that collagen fibrils are arranged perpendicular to the articular surface. This creates a arcade formation. These arcades are to be created by the attempt to transfer the initial fibril network to a higher order, whereby the arcadic structure supports the overlying load. | |||
|- | |||
|Interface | |||
|tide mark | |||
|Distinguishes the deep zone from the calcified cartilage. This irregularly salty layer lies between the Zonae radiata and calcificata and separates the lime-poor from the lime-rich cartilage. This has been described as the mineralization front of the cartilage. The layer is thought to arise by causing the collagen bundles to twist before going deeper to penetrate the zona calcificata and the bone tissue | |||
|Consists of a band of fibrils attached to the collagen fibers which are anchored in the lime-poor layer, and thus prevent them from tearing off cartilage from bone | |||
|- | |||
|Zone IV | |||
|calcified zone | |||
|Plays an integral role in securing the cartilage to bone by anchoring the collagen fibrils of the deep zone to subchondral bone. In this zone, the cell population is scarce and chondrocytes are hypertrophic | |||
|Numerous protrusions, hollows, and interlacing, which gives an excellent resistance to shear forces to prevent the cartilage detaching from the underlying bone | |||
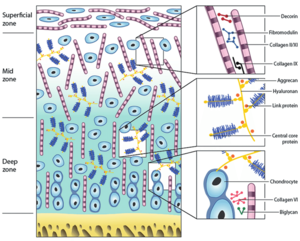
|}[[File:Zones and constituents of articular cartilage.png|thumb|Zones and constituents of articular cartilage. A schematic representation of the different matrix components and their organization throughout articular cartilage. ]]The cellular arrangement reflects the function of each layer. The superficial layer has cells arranged tangentially because it is subjected to both compression and friction. In cross-section these superficial cells are discoid. In comparison, the middle layer cells are spherical in cross-section. | |||
The collagen within the matrix has a certain arrangement. It passes upwards through the matrix and surrounds cells in an arcadic manner. This disposition retains the matrix in discrete regions. In the superficial layer the final arch contains a layer of collagen that run parallel to the cells in the direction of greatest insult. | |||
Cellular density is highest at the superficial layer, with reducing density down to the deep layer. | |||
=== Components of Articular Cartilage === | |||
The critical component of cartilage is water. The proteoglycans include aggrecan, dermatosulphate proteoglycans, and fibromodulin. The main collagen type found is type II. Non-collagenous proteins include structural glycoproteins and matrix metalloproteinases. | |||
{| class="wikitable" | |||
|+General Composition of Articular Cartilage.<ref name=":0" /> | |||
!Component of Articular Cartilage | |||
!Percentage | |||
! | |||
|- | |||
|'''Water''' | |||
|70 - 80% | |||
| | |||
|- | |||
|'''Chondrocytes''' | |||
|1 - 10% | |||
| | |||
|- | |||
|'''Collagen''' | |||
|12 - 14% | |||
| | |||
|- | |||
| - Type II | |||
|10 - 12% | |||
| | |||
|- | |||
| - Type IX | |||
|~1% | |||
| | |||
|- | |||
| - Type XI | |||
|~1% | |||
| | |||
|- | |||
|'''Proteoglycans''' | |||
|7 - 9% | |||
| | |||
|- | |||
| - Hyaluronic acid—proteoglycans—aggregates | |||
|6 - 8% | |||
| | |||
|- | |||
| - Other proteoglycans | |||
|~1% | |||
| | |||
|- | |||
|'''Mineralic materials''' | |||
|<4% | |||
| | |||
|- | |||
|'''Matrix metalloproteinases''' | |||
|<1% | |||
| | |||
|} | |||
'''Water''' | |||
The matrix is composed of water, proteoglycans, collagen, and non-collagenous proteins. Water is found in the joint and water alone can withstand intermittent compression. Water is compressible but with compression it has the undesired effect of flowing and dissipating. Water is therefore held in place thermodynamically and electrostatically by proteoglycans. Proteoglycans are retained in turn by collagen. The collagen is responsible for maintaining the articular cartilage in a form to resist the next phase of compression. | |||
In other words water is retained by proteoglycans, and proteoglycans are bound by collagen. Proteoglycans and collagen are produced by cells. Non-collagenous proteins are also produced that function to hold the components together and regulate them. Chondrocytes are therefore required to afford the cartilage its mechanical properties. | |||
'''Chondrocytes''' | |||
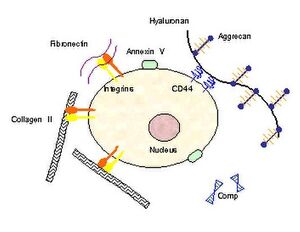
[[File:Chondrocyte receptors.jpg|thumb|A chondrocyte with surface membrane mechanoreceptors (annexins, CD44, integrins) that are sensitive to pressure and stretching of the cell membrane. ]] | |||
There is a zone of matrix that immediately surrounds the cells known as peri-cellular matrix. Then there is a region of matrix surrounding the cell but more displaced known as the territorial matrix. The matrix in between cells or clusters of cells is known as interterritorial matrix. Collagen is the dominant constituent in the interterritorial matrix. In the pericellular matrix the dominant constituents are proteoglycans and hyaluronic acid. | |||
Cyclic compressive loading is important for nutrition to the chondrocytes and waste removal because cartilage is an avascular tissue. Waste is removed with compression, and nutrients diffuse in from synovial fluid with removal of compression. Excessive loading may negatively influence the cells resulting in cell apoptosis and destruction of the matrix.<ref name=":1">Roughley, P.J., Mort, J.S. The role of aggrecan in normal and osteoarthritic cartilage. ''J EXP ORTOP'' 1, 8 (2014). <nowiki>https://doi.org/10.1186/s40634-014-0008-7</nowiki></ref> | |||
Chondrocytes have mechanoreceptors on their surface. These receptors sense and transform the mechanical signal into biochemical signals that results in the synthesis and degradation of the components of the cartilaginous extracellular matrix. The processes include the synthesis of collagens, proteoglycans, proteases, protease inhibitors, transcription factors, cytokines, and growth factors. The balance between the anabolic and catabolic processes is influenced by the type of loading that the cartilage experiences. High strain rates cause tissue damage, degradation, decreased matrix production, and apoptosis. While decreased mechanical loading leads to a loss of matrix production. Low frequency oscillatory loads are beneficial, while static loads are detrimental. | |||
'''Aggrecan and Aggregated Proteoglycans''' | |||
[[File:Cartilage extracellular matrix.png|left|thumb|Components of the extracellular matrix. Proteoglycan aggregates contains a central filament of hyaluronic acid to which multiple aggrecans are attached through link proteins. The glycosaminoglycans carry numerous negative charges. The interstices of this porous solid matrix are filled with water and dissolved ions]] | |||
There are three macroclasses of proteins in articular cartilage: collagens (mostly type II collagen); proteoglycans (mostly aggrecan); and other non-collagenous proteins (link protein, fibronectin, matrix protein) and smaller proteoglycans (biglycan, decorin, fibromodulin).<ref name=":0" /> | |||
Aggrecan being the major proteoglycan in articular cartilage contains a core protein with numerous covalently attached sulfated glycosaminoglycan (GAG) chains. These GAGs are in the form of chondroitin sulfate and keratan sulfate. A greater proteoglycan concentration provides greater resistance to shear forces. The highest density is found in the middle zone. | |||
Aggrecan doesn't exist in isolation but rather in the form of proteoglycan aggregates. Each aggregate contains a central filament of hyaluronic acid with multiple aggrecan molecules attached non-covalently via one terminus of their core proteins. A link protein stabilises the interaction between the aggrecan and hyaluronic acid.<ref name=":1" /> | |||
[[File:Aggrecan domains.png|thumb|The proteoglycan aggregate is depicted as a central hyaluronan (HA) filament with aggrecan and link proteins (LP) attached to it. The domains of the aggrecan core protein are indicated. G1, G2 and G3, globular regions; IGD, interglobular domain (Between G1 and G2, not labelled); KS, keratan sulfate-rich domain; CS1 and CS2, chondroitin sulfate-rich domains]] | |||
The core protein of aggrecan contains three disulfide-bonded globular regions which are termed G1, G2, and G3. There are what are called "extended domains" between G1 and G2 called E1 (also called interglobular domain); and between G2 and G3 called E2. <ref name=":1" /> | |||
The proximal G1 region resembles an immunoglobulin and is called the immunoglobulin fold (Ig fold). This end is responsible for linking to hyaluronic acid and held to it by a similarly shaped link protein. | |||
The function of G2 is unknown but is structurally similar to G1. There is a short interglobular region (sometimes called E1) between G1 and G2, and this region is a prominent site of proteolysis.<ref name=":1" /><blockquote> | |||
The interglobular region between G2 and G3 is longer (sometimes called E2). It is here that the water trapping glycosaminoglycans chondroitin sulfate and keratan sulfate are attached to the protein core. The term water trapping is used because there the binding process is by both electrostatic and thermodynamic forces. Most keratan sulfate is found in the proximal end of E2, which is called the KS region. All of the chondroitin sulfate is found in the terminal three quarters of E2, of which there are the CS1 and CS2 regions. This area also contains some keratan sulfate.<ref name=":1" /></blockquote> | |||
The G3 region is involved in normal transit of the aggrecan within the chondrocyte and its secretion into the matrix. It also has a role in anchoring aggrecan within the tissue through binding to other proteins such as fibulins and tenascins. G3 is absent in many mature aggrecan molecules due to its protelytic cleavage,<ref name=":1" /> but mutations that abolish binding of G3 to fibulins and tenascins leads to familial osteochondritis dissecans.<ref name=":5">Hochberg, Marc C., et al. ''Rheumatology''. Philadelphia, PA: Elsevier, 2019.</ref> | |||
'''Dermatosulphate Proteoglycans''' | |||
Interspersed throughout the matrix are a variety of other proteoglycans. The dermatosulphate proteoglycans are biglycan and decorin. Bogduk includes fibromodulin in this group. These are proteoglycans with a protein core from which stem glycosaminoglycans. | |||
* ''Biglycan'' has two glycosaminoglycan chains and it acts as an inhibitor of fibrinogen. Repair involves activation of fibrinogen and deposition of fibrin. | |||
* ''Decorin'' can interact with collagen and inhibit fibrillogenesis. Fibrillogenesis is the manufacture of thicker collagen fibres. Decorin can also bind to chondronectin and growth factors such as TGF. It has a wide range of effects including cell growth, differentiation, proliferation, adhesion, spread and migration, and has pro-inflammatory and anti-fibrosis effects.<ref>Zhang, Wen et al. “Decorin is a pivotal effector in the extracellular matrix and tumour microenvironment.” ''Oncotarget'' vol. 9,4 5480-5491. 3 Jan. 2018, doi:10.18632/oncotarget.23869</ref> | |||
* ''Fibromodulin'' has a protein core and small glycosaminoglycan chain. Fibromodulin sits on the surface of collagen fibres and regulates their assembly. It inhibits the deposition of proto-collagen fibres onto existing collagen fibres. | |||
'''Collagens''' | |||
There are a variety of collagens in cartilage that come from various chemical classes of collagen. | |||
Class 1 collagens are the fibril forming collagens, those that can make strings. The main example in articular cartilage is type II collagen which comprises some 90% to 95% of the collagen and is responsible for the tensile strength of the tissue. Type XI collagen is responsible for controlling fibril diameter. Type VI is found in the territorial matrix. | |||
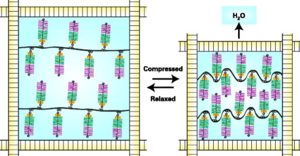
Class 3 collagens are those that form short helices. Type IX collagen is responsible for bridging between itself and type II. Type X is found in zone IV.[[File:Aggrecan function.png|thumb|The equilibrium between the swelling of the aggrecans and the tensile forces of surrounding collagen.|alt=|left]]Collagen maintains the volume and shape of the matrix because by winding around and entrapping the proteoglycan aggregates it restricts the swelling of the proteoglycans with water imbibement to about 20% of their maximum. | |||
In their relaxed state the aggregates swell as the anionic chondroitin sulfate and keratan sulfate GAG chains draw in water. An equilibrium is reached whereby the swelling is in balance with the tensile forces of the collagen fibrils. With compression, water is displaced, and the GAG chains are brought closer together. This increases their swelling potential and balances the applied load. The increased swelling potential is dissipated when the load is removed, the aggrecan re-swells, and the original equilibrium is restored.<ref name=":1" /> | |||
The most important property of collagen is its tensile strength. Collagen buckles when it is compressed. The tensile strength properties of collagen is complementary to proteoglycans which ensure compressive strength, elasticity, and the lifespan of articular cartilage. <ref name=":0" /> | |||
For optimal cartilage function and the ability to reach this equilibrium, the cartilage requires a high concentration of aggrecan, a high degree of aggrecan sulfation, and the capacity to form large aggregates. All three of these properties are impaired in osteoarthritis.<ref name=":1" /> | |||
'''Non-collagenous Proteins''' | |||
The structural glycoproteins are molecules found on the surface of cells referred to as adhesion molecules. They bind chondroblasts to type II collagen. We see an interaction between the cells that produce the matrix and the matrix components itself. The best known structural glycoproteins are chondronectin and anchorin. | |||
Cartilage oligomerix protein (COMP) is also known as thrombospondin 5. It's exact function remains unclear but it appears to be an important regulator of extracellular matrix assembly and stabilisation of the matrix through interacting between collagen fibrils and matrix components. It has been studied as both a diagnostic and prognostic indicator of osteoarthritis; it is significantly upregulated in early osteoarthritis even long before diagnosis.<ref>Tseng, Susan et al. “Cartilage Oligomeric Matrix Protein (COMP): A Biomarker of Arthritis.” ''Biomarker insights'' vol. 4 33-44. 17 Feb. 2009, doi:10.4137/bmi.s645</ref> | |||
'''MMPs''' | |||
Some of the best known proteolytic enzymes are the matrix metalloproteinases (MMPs), and as indicated by their name occur in the matrix. Metallo refers that these enzymes require zinc as a component that allows them to act on the proteins. Calcium is involved in this interaction. | |||
MMPs are secreted in an inactive form, with proteolytic loss of the propeptide leading to activation in the matrix. For example MMP-1, -2, and -3 are produced as pro-collagenase, pro-gelatinase, and pro-stromelysin, respectively. In contrast, the membrane type MMPs (MT-MMPs) and stomelysin-3 (MMP-11) are secreted as active enzymes. Most MMPs are produced by different connective tissue cells after stimulation by a variety of mediators.<ref>Brandon J. Rose, David L. Kooyman, "A Tale of Two Joints: The Role of Matrix Metalloproteases in Cartilage Biology", ''Disease Markers'', vol. 2016, Article ID 4895050, 7 pages, 2016. <nowiki>https://doi.org/10.1155/2016/4895050</nowiki></ref> | |||
There are some 29 MMPs, and they are divided into four main groups:<ref name=":5" /> | |||
# ''<u>Collagenases</u>'': (e.g. MMP-1, -8, -13). These enzymes cleave fibrillar collagens at a single site to produce fragments of three quarters and one quarter of the original size. MMP-13 has the broadest substrate specificity. They have strong activity for cleavage of type II collagen, but other molecules such as types IV and IX collagen, perlecan, osteonectin, and proteoglycan. MMP-1 and MMP-13 are synthesised by macrophages, fibroblasts, and chondrocytes upon stimulation by inflammatory mediators. MMP-8 is predominantly released by neutrophils upon stimulation but also by chondrocytes. All three are present in diseased cartilage. | |||
# ''<u>Gelatinases</u>'': (MMP-2 and -9) These act on breakdown products of type IV and V collagen and elastin. MMP-2 is the most widely expressed. | |||
# ''<u>Stromelysins</u>'': (e.g. MMP-3). These acts on a wide array of extracellular molecules including various collagens, fibronectin, laminin, elastin, and various proteoglycans. | |||
# ''<u>MT-MMPs</u>'' (e.g. MMP-14): MMP-14 can initiate activation cascades on the cell surface that activate procollagenases. | |||
'''ADAMTS and ADAMS''' | |||
Relatives of the MMPs are the ADAMTS enzymes (short for A Disintegrin And Metalloproteinase with Thrombospondin Motifs) and ADAMs (A Disintegrin And Metalloproteinases). These enzymes are also dependent on zinc. These enzymes were more recently discovered. There are 20 ADAMTS and 33 ADAMS enzymes, with a large number of them having effects on cartilage. | |||
ADAMTS enzymes are involved in both the synthesis and degradation of the extracellular matrix. ADAMTS enzymes include:<ref name=":5" /> | |||
# ''<u>Procollagen propeptidases</u>'' (ADAMTS-2, -3, and -14) that are involved in the maturation of triple helical collagen fibrils | |||
# ''<u>Aggrecanases</u>'' (ADAMTS-1, -4, -5, -9, and -15) that are involved in aggrecan cleavage along with MMPs. ADAMTS5 is about 1,000 times more potent than ADAMTS4.<ref name=":2" /> | |||
ADAMTS enzymes are also involved in the cleavage of oligomerix matrix protein, have roles in cartilage metabolism, as well as in chondrocyte differentiation and proliferation. The role that the various ADAMTS and ADAMS enzymes play in joint health and disease is still being studied.<ref name=":2">Yang CY, Chanalaris A, Troeberg L. ADAMTS and ADAM metalloproteinases in osteoarthritis - looking beyond the 'usual suspects'. Osteoarthritis Cartilage. 2017 Jul;25(7):1000-1009. doi: 10.1016/j.joca.2017.02.791. Epub 2017 Feb 13. PMID: 28216310; PMCID: PMC5473942.</ref> | |||
ADAMs are usually membrane-anchored proteinases. It is thought that they play a role in signalling pathways in chondrocytes to fine-tune tissue homeostasis.<ref>Yang, C-Y et al. “ADAMTS and ADAM metalloproteinases in osteoarthritis - looking beyond the 'usual suspects'.” ''Osteoarthritis and cartilage'' vol. 25,7 (2017): 1000-1009. doi:10.1016/j.joca.2017.02.791</ref> | |||
'''Serine Proteinases''' | |||
Serine proteinases are understudied despite there being almost as many of these as there are MMPs. They are thought to be involved in regulation of cell signalling, modulation of the activity of growth factors, promotion of inflammatory processes, modulation of chemokines, and as a protective feedback mechanism in maintaining cartilage homeostasis.<ref name=":5" /> | |||
=== Matrix Synthesis and Degradation === | |||
The chondrocytes slowly but constantly act to have effects in both the synthesis and degradation of the extracellular matrix. Degradation is an important aspect as it allows for old components to be removed to making way for refreshed components. In the normal state there is a balance between synthesis and degradation. If the balance tips to favouring degradation, then degenerative changes occur. | |||
Synthesis is promoted by various growth factors including transforming growth factor (TGF), basic fibroblast growth factor (bFGF), and insulin like growth factor (IGF). Degradation occurs through the action of metalloproteases. MMP-13 plays a central role in degrading type II collagen, while ADAMT-4 and -5 are primary agents that degrade aggrecan. Tumour necrosis factor α interleukin-1 (IL-1) promote the action of metalloproteinases, but degradation also occurs through superoxide (O<sub>2</sub><sup>−</sup>) and nitric oxide. | |||
'''Synthesis''' | |||
The chondroblast produces the components of the extracellular matrix. The endoplasmic reticulum within the chondroblast synthesises the various collagens and other proteins of the matrix such as fibromodulin and decorin. At the base of the golgi apparatus there is some endoplasmic reticulum that forms the protein component of the proteoglycans. The carbohydrate component is added to the protein core by the golgi apparatus. Anchorin is an adhesion molecule that sits on the surface of the chondroblast. | |||
The chondroblast can be stimulated by a variety of factors to produce collagen and proteoglycans.<ref name=":5" /> | |||
* ''Fibroblast growth factor'' (FGF) is an extrinsic regulator that comes from outside the cell and stimulates the nucleus of the chondroblast to produce the protein and proteoglycan components of the matrix. | |||
* ''Insulin like growth factor'' (IGF) also comes from the outside, and activates the nucleus by a second messenger to produce the components of the matrix. | |||
* ''Transforming growth factor'' (TGF) is produced by the cell itself, and is bound to collagen through decorin. While TGF is buried within the proteoglycans surrounding collagen it can't escape and has no influence. If the proteoglycans are removed and the collagen is exposed, so is TGF, and floats back to the cell where it enhances the effect of FGF through a positive feedback loop. This activates the cell to produce materials, with a preferential effect for the production of proteoglycans, which closes the loop by enclosing collagen and blocking the effect of TGF. | |||
* ''Bone morphogenic proteins'' (BMPs): these have direct effects on chondrocytes and are involved in promoting matrix deposition in osteoarthritis (e.g. osteophytosis). | |||
'''Degradation''' | |||
Cartilage produce many enzymes that can destroy the matrix. The complete collection of proteases is called the degradome and includes around 588 different proteinases. These include the Matrix Metalloproteinases (MMPs), the A Disintegrin And Metalloproteinase Domain with Thrombospondin Motifs (ADAMTS) family, and the serine proteinases. With the primary structural components of cartilage matrix being collagen and aggrecan, MMP-13 and ADAMTS-4 and -5 play a central role in cartilage degradation. | |||
The ADAMTS are important in the initial degradation of cartilage matrix. ADAMTS-4 and ADAMTS-5 can cleave the interglobular domain between G1 and G2, leaving a shortened aggrecan with decreased numbers of fixed charged groups. This is thought to be a key step in the pathologic loss of aggrecan. They can also cleave several sites close to the G3 domain. Following cleavage between G1 and G2, the G1 domain remains bound to hyaluronic acid can then be cleaved by MMPs. Also of note, the combined action of the ADAMTs aggrecanases and MMPs results in the release of a soluble bioactive peptide that promotes further cartilage breakdown.<ref name=":5" /> | |||
MMP-1 and MMP-13 are both relatively specific for action on type II collagen. They act on type II collagen up towards one end. Once the collagen molecule is split, gelatinase acts on the products. MMP-13 is thought to also be involved in matrix turnover in healthy cartilage. MMP-13 (Collagenase-3) is considered to be the major catabolic effector in osteoarthritis, while MMP-1 is thought to be the primary collagenase in rheumatoid arthritis. MMP-13 It has been extensively studied and selective MMP-13 inhibitors for treating osteoarthritis are being developed.<ref name=":2" /> The role of MMP-1 in osteoarthritis may vary depending on the joint.<ref>Kevorkian L, Young DA, Darrah C, Donell ST, Shepstone L, Porter S, Brockbank SM, Edwards DR, Parker AE, Clark IM. Expression profiling of metalloproteinases and their inhibitors in cartilage. Arthritis Rheum. 2004 Jan;50(1):131-41. doi: 10.1002/art.11433. PMID: 14730609.</ref> | |||
The other components of the matrix are acted on by MMP-3 (stromelysin). MMP-3 is the most highly expressed MMP gene in normal cartilage and remains comparatively high in osteoarthritis. MMP-3 can also cleave aggrecan molecules between G1 and G2. Other processes operate to liberate the link protein and head end of the aggrecan molecule. These products leak into the synovial fluid and removed via transportation through lymph. MMP-3 can act on other collagens within the matrix such as type XI and IX and the terminal ends of type II collagen. MMP-3 can also act on smaller collagens found around the cell such as type XI, and other proteins such as fibronectin. MMP-3 is a good general debriding enzyme. In osteoarthritis there appears to be an excessive degradation of the matrix. | |||
A feature of aging cartilage is the accumulation of hyaluronic acid chains that bear the old remnant head end of the aggrecan molecule, that isn't removed, and this remnant prevents the binding of fresh aggrecan molecules. This contributes to the compromise of articular cartilage with age. | |||
In healthy articular cartilage there the extracellular matrix is slowly but continuously refreshed. Old collagen is removed and replaced by new collagen; old proteoglycans are removed and replaced by new proteoglycans. There is a balance between synthesis and degradation of the matrix. | |||
Tissue inhibitors of metalloproteinases (TIMP) can control the activation of the MMPs and ADAMTS enzymes preventing uninhibited action of these enzymes. With reduced activity of TIMPs there may be excessive degradation for the amount of synthesis occurring. | |||
Cytokines that have an effect on the chondroblast and promote degradation include interleukin (IL), tumour necrosis factor α (TNF), and interferon (IFN). These mediators have two sorts of effects. There is a lesser effect of stimulation of the production of degradative enzymes. The dominant effect is the inhibition of the synthesis of the proteins, collagens, and proteoglycans. Superoxide radicals and nitric oxide also promote degradation. Inflammatory effects do not explain all of the features of the genesis of osteoarthritis. | |||
== Synovial Membrane == | |||
'''Intima and Subintima''' | |||
The term synovium refers to the soft tissue lining of diarthrodial joints, tendon sheaths, and bursae. It contains a surface layer called the intima, and underlying tissue called the subintima. Between the intimal surfaces is a small amount of fluid that is usually rich in hyaluronic acid. The synovium provides a non-adherent surface between tissue elements.<ref>Smith, Malcolm D. “The normal synovium.” ''The open rheumatology journal'' vol. 5 (2011): 100-6. doi:10.2174/1874312901105010100</ref> | |||
The intima contains macrophages and fibroblasts and is two to three layers of cells thick. The cells aren't continuous like epithelium. Between them runs an amorphous matrix. The gaps between the cells allow easy communication through the intima. | |||
The subintima consists of a loose network of collagen fibres; blood vessels; fat globules; and a variety of cells including mast cells, fibroblasts, and macrophages. | |||
The blood vessels within the subintima produce most of the components by volume of synovial fluid. There is a transudate of fluid and proteins that passes into the joint space to start to produce synovial fluid.. | |||
'''Synovial macrophages''' | |||
These are also known as macrophage-like synoviocytes (MLS), or type A synoviocytes. These are essentially macrophages. Previously they were thought to arise from bone marrow, but in reality they are derived from embryonic precursor cells and maintained by independent slow proliferation. <ref name=":3">Tu J, Hong W, Zhang P, Wang X, Körner H, Wei W. Ontology and Function of Fibroblast-Like and Macrophage-Like Synoviocytes: How Do They Talk to Each Other and Can They Be Targeted for Rheumatoid Arthritis Therapy? Front Immunol. 2018 Jun 26;9:1467. doi: 10.3389/fimmu.2018.01467. PMID: 29997624; PMCID: PMC6028561.</ref> | |||
They remove debris from the synovial fluid such as degraded aggrecans and other material that interfere with the lubricating property. | |||
They also produce prostaglandins that can affect vasodilation or constriction of the subintimal blood vessels, thereby regulating the production of synovial fluid. For example in inflamed joints, prostaglandin production results in an effusion. | |||
Synovial lining macrophages share certain features in common with epithelial cells. They express tight junction proteins, and provide an anti-inflammatory barrier around the joint that impairs immune cell traffic in a steady state. During arthritis this barrier "cracks" open.<ref name=":4">Collison, J. Synovial macrophages shield the joints. ''Nat Rev Rheumatol'' 15, 573 (2019). <nowiki>https://doi.org/10.1038/s41584-019-0295-6</nowiki></ref> Macrophages make up the minority of cells in normal intima, except in inflammatory arthritis where they make up 80% of the intima.<ref name=":4" /> | |||
These cells are also involved in the immune system as antigen presenting cells. | |||
'''Synovial fibroblasts''' | |||
These are also known as fibroblast-like synoviocytes (FLS), or type B synoviocytes. They are more abundant than synovial macrophages. They are thought to arise from mesenchymal stem cells. <ref name=":3" /> | |||
Fibroblasts produce inhibitors of phagocytic enzymes that are in turn produced by macrophages, and thereby prevent excessive activity. | |||
Fibroblasts also secrete lubricin, the obsolete term for this was lubricating glycoprotein (LGP). It is also known as superficial zone protein. Lubricin is the cardinal component of synovial fluid and provides an anti-friction property. Hyaluronic acid and proteins on their own do not have an anti-friction property. Lubricin is also expressed by superficial zone chondrocytes and to a lesser extent intermediate zone chondrocytes.<ref>Jay GD, Waller KA. The biology of lubricin: near frictionless joint motion. Matrix Biol. 2014 Oct;39:17-24. doi: 10.1016/j.matbio.2014.08.008. Epub 2014 Aug 27. PMID: 25172828.</ref> | |||
These cells also produce hyaluronan (note previously thought that this was produced by macrophages).<ref name=":4" /> | |||
FLS are involved in many pathological aspects of rheumatoid arthritis and promote synovitis, pannus growth, and cartilage/bone destruction. | |||
== Joint Lubrication == | |||
{{See also|Cartilage Biomechanics}} | |||
The ability of synovial fluid to lubricate the surface of cartilage depends on Lubricin (superficial zone protein), a glycoprotein located on the surface of the synovium and cartilage. | |||
Hyaluronan is the main factor that is responsible for retaining a constant volume of fluid during exercise. The fluid cushions the synovial tissue and acts as a reservoir for lubricant for the cartilage. Mechanical stimulation of synovial fibroblasts is likely a key factor for stimulating the synthesis of hyaluronan. So when there is a large volume of synovial fluid, there is decreased mechanical stimulation and hence reduced synthesis, and vice versa. | |||
Joint effusions can be created by two mechanisms, but they are not necessarily distinct. [[Osteoarthritis]] can display both mechanisms. | |||
# Mechanical irritation: such as in osteoarthritis, there is excessive production of hyaluronan by synovial fibroblasts through frictional forces. | |||
# Synovitis: this occurs through the accumulation of exudate, i.e. inflammatory oedema through increased vascular permeability. | |||
== List of {{PAGENAME}} == | |||
{{#ask: | |||
[[Has joint type::Synovial Joint]] | |||
|?Has joint secondary type=Joint type | |||
|?Has joint bones=Bones | |||
|?Has joint ligaments=Ligaments | |||
|?Has joint muscles=Muscles | |||
|?Has joint innervation=Innervation | |||
|?Has joint vasculature=Vasculature | |||
|?Has joint rom=ROM | |||
|?Has joint volume=Volume | |||
|mainlabel = [[Synovial Joint]] | |||
}} | |||
== Resources == | |||
{{Members link}} | |||
== See Also == | |||
* [[Articular Nociceptors]] | |||
== References == | |||
[[Category:Tissues]] | |||
<references /> | |||
[[Category:Joint Types]] | |||
Revision as of 21:20, 1 May 2022
The cardinal feature of a synovial joint is that it is capable of substantial movement, such as with sliding in bending. This is in contrast to fibrocartilaginous and cartilaginous joints where the amplitude of movement is significantly lower.
Overview of Synovial Joint Structure
Joint Space: There must be some form of space between the two bones which allows the synovial joint to move. The space is quite narrow. The bones may be shaped in such a way to allow certain movements. For example flat surfaces allow sliding.
Cartilage: The most common effect that occurs at the joint is compression. When muscles act on the joint to move the joint they also exert a compression load across the joint space. The two bones are therefore subjected to phasic (intermittent) compression. Bones on their own are not well designed for phasic loads, but rather are better suited towards static loads. To protect against intermittent compression forces, the joint surfaces are lined with cartilage which provides a cushion or buffer. Cartilage is softer and somewhat more resilient than bone and can dissipate compression forces.
Synovial Fluid: A second hazard is friction. With movement in a gliding fashion, there is friction, which could result in stripping of the cartilage layers. To protect against friction the joint contains synovial fluid. This allows gliding movements between the joint surfaces. The synovial fluid layer is only one molecule thick, which is enough to provide the required anti-friction effects.
Synovial Membrane: The next design issue is that the synovial fluid has to be contained within the joint space and maintained at a suitable quality. Synovial membrane provides these functions. This structure is a sleeve of tissue that surrounds the joint space peripherally, and encloses the space in a thin membrane. The cells of the synovial membrane maintain the quality of the synovial fluid by removing debris and recycling used components back into the bloodstream.
Synovial Membrane Blood Vessels: The blood vessels located on the outer aspect of the synovial membrane have the role of synovial fluid production. Water and protein passes from the blood vessels, across the synovial membrane, and into the joint space. Various cells within the synovial membrane modify the synovial fluid to give the required structure.
Joint Capsule: The synovial membrane is delicate and is easily torn. It is supported on its outer surface by a joint capsule. This is relatively strong fibrous tissue that surrounds the joint space as another sleeve. The synovial membrane extends from the edge of the articular cartilage of one bone to the edge of the articular cartilage of the opposing bone. The capsule attaches further up along the neck of the two opposing bones. The main role of the capsule is protection of the synovial membrane, but also provides some mechanical stability.
Inclusions: Synovial joints can have intra-articular inclusions. A fibro-adipose meniscoid is a washer-like extension of the synovial membrane and capsule that extends into the joint cavity. The meniscoid has fatty tissue, with loose collagen and blood vessels at its core, coated by an extension of the synovial membrane. The function of the meniscoid is to subdivide the joint into two cavities. This results in lubricating fluid being present within each compartment.
Meniscoids are very common, and tend to be found in joints that have substantial sliding movements. During sliding the joint essentially subluxes, and there is unopposed cartilage. The meniscoid leaves the joint cavity and maintains the lubricating layer on the unopposed cartilage. When the joint returns to its neutral position, it does so with the joint surfaces having their lubricating layer being kept in place., and the meniscoid then re-enters the joint cavity.
Ligaments: The joint can be reinforced externally by ligaments. Ligaments may blend with the outer surface of the capsule, or stand alone leaving a space between the deep surface of the ligament and the capsule. Ligaments aren't an essential component of synovial joints, but are a common feature. The function of ligaments are to stabilise the joint against undesired movements.
Blood Vessels, Lymphatics, Nerves: The tissues of the joints have a blood supply with an arterial and venous supply. Lymphatic vessels drain excess fluid from the joint or synovial space. A nerve supply endows the joint and ligaments which monitor position and provide an alerting mechanism against threatened damage if there is excessive strain.
Articular Cartilage
Articular cartilage is a tissue that can resist, absorb, dissipate, and transmit intermittent compression. This is in contrast to bone which is better at resisting static compression. The cartilage retains its form and remains available for the next phase of compression. It also provides a smooth surface over which a joint can glide.
Articular cartilage is on average 2 to 4mm thick (retropatellar up to 7 to 8mm), and it doesn't have blood vessels, nerves, or lymphatics.
Zonal Regions
There are different classification systems to describe the four layers within articular cartilage. At the bottom of the deep layer is the tidemark. The tidemark is the boundary between uncalcified matrix above and calcified matrix below.
- Numerical system: identifies layers from I to IV from superficial to deep.
- Topographical system: identifies layers as superficial, middle, deep, and calcified layers. The calcified layer has received a deposit of calcium and is trying to transform into bone like the subchondral bone underlying it.
- Cellular orientation system: identifies layers as tangential in the superficial layer because they run tangential to the surface, transitional in the middle layer because they are clumped and scattered, and radial in the deep layer because they are arranged in radial columns. The fourth layer is again called calcified.
| Zone | Name | Description | Functional Behaviour |
|---|---|---|---|
| Zone I | superficial (tangential) zone | 10% to 20% of AC thickness. The collagen fibres of this zone are packed tightly and aligned parallel to the articular surface. The chondrocytes in the superficial zone are flatter and smaller and generally have a greater density than that of the cells deeper in the matrix. It protects deeper layers from shear stresses. The zona superficialis has most of the water and very little proteoglycans. In general, the cells are not very active, which means that there is little wear and tear. The zone can also be used as a barrier against large molecules, for example antibodies | Responsible for the behaviour of the cartilage under stress. It deforms more strongly and is therefore less rigid than the underlying zones. If this zone is disturbed tissue permeability increases, leading to greater fluid exchange of the cartilage with its surroundings and during compression, this leads to greater mechanical stress on the macromolecular network. The cells here also produce lubricin. |
| Zone II | middle (transitional) zone | 40% to 60% of the total AC volume, and it contains proteoglycans and thicker collagen fibrils. In this layer, the collagen is organized obliquely. Chondrocytes are spherical and at low density | First line of resistance against compressive forces. The upper aspect produces lubricin. |
| Zone III | deep (radial) zone | Approximately 30% of the AC volume. The deep zone contains the largest diameter collagen fibrils in a radial disposition, the highest proteoglycan content, and the lowest water concentration. The chondrocytes are typically arranged in a columnar orientation, parallel to the collagen fibers and perpendicular to the joint line. | Responsible for providing the greatest resistance to compressive forces, given that collagen fibrils are arranged perpendicular to the articular surface. This creates a arcade formation. These arcades are to be created by the attempt to transfer the initial fibril network to a higher order, whereby the arcadic structure supports the overlying load. |
| Interface | tide mark | Distinguishes the deep zone from the calcified cartilage. This irregularly salty layer lies between the Zonae radiata and calcificata and separates the lime-poor from the lime-rich cartilage. This has been described as the mineralization front of the cartilage. The layer is thought to arise by causing the collagen bundles to twist before going deeper to penetrate the zona calcificata and the bone tissue | Consists of a band of fibrils attached to the collagen fibers which are anchored in the lime-poor layer, and thus prevent them from tearing off cartilage from bone |
| Zone IV | calcified zone | Plays an integral role in securing the cartilage to bone by anchoring the collagen fibrils of the deep zone to subchondral bone. In this zone, the cell population is scarce and chondrocytes are hypertrophic | Numerous protrusions, hollows, and interlacing, which gives an excellent resistance to shear forces to prevent the cartilage detaching from the underlying bone |
The cellular arrangement reflects the function of each layer. The superficial layer has cells arranged tangentially because it is subjected to both compression and friction. In cross-section these superficial cells are discoid. In comparison, the middle layer cells are spherical in cross-section.
The collagen within the matrix has a certain arrangement. It passes upwards through the matrix and surrounds cells in an arcadic manner. This disposition retains the matrix in discrete regions. In the superficial layer the final arch contains a layer of collagen that run parallel to the cells in the direction of greatest insult.
Cellular density is highest at the superficial layer, with reducing density down to the deep layer.
Components of Articular Cartilage
The critical component of cartilage is water. The proteoglycans include aggrecan, dermatosulphate proteoglycans, and fibromodulin. The main collagen type found is type II. Non-collagenous proteins include structural glycoproteins and matrix metalloproteinases.
| Component of Articular Cartilage | Percentage | |
|---|---|---|
| Water | 70 - 80% | |
| Chondrocytes | 1 - 10% | |
| Collagen | 12 - 14% | |
| - Type II | 10 - 12% | |
| - Type IX | ~1% | |
| - Type XI | ~1% | |
| Proteoglycans | 7 - 9% | |
| - Hyaluronic acid—proteoglycans—aggregates | 6 - 8% | |
| - Other proteoglycans | ~1% | |
| Mineralic materials | <4% | |
| Matrix metalloproteinases | <1% |
Water
The matrix is composed of water, proteoglycans, collagen, and non-collagenous proteins. Water is found in the joint and water alone can withstand intermittent compression. Water is compressible but with compression it has the undesired effect of flowing and dissipating. Water is therefore held in place thermodynamically and electrostatically by proteoglycans. Proteoglycans are retained in turn by collagen. The collagen is responsible for maintaining the articular cartilage in a form to resist the next phase of compression.
In other words water is retained by proteoglycans, and proteoglycans are bound by collagen. Proteoglycans and collagen are produced by cells. Non-collagenous proteins are also produced that function to hold the components together and regulate them. Chondrocytes are therefore required to afford the cartilage its mechanical properties.
Chondrocytes
There is a zone of matrix that immediately surrounds the cells known as peri-cellular matrix. Then there is a region of matrix surrounding the cell but more displaced known as the territorial matrix. The matrix in between cells or clusters of cells is known as interterritorial matrix. Collagen is the dominant constituent in the interterritorial matrix. In the pericellular matrix the dominant constituents are proteoglycans and hyaluronic acid.
Cyclic compressive loading is important for nutrition to the chondrocytes and waste removal because cartilage is an avascular tissue. Waste is removed with compression, and nutrients diffuse in from synovial fluid with removal of compression. Excessive loading may negatively influence the cells resulting in cell apoptosis and destruction of the matrix.[3]
Chondrocytes have mechanoreceptors on their surface. These receptors sense and transform the mechanical signal into biochemical signals that results in the synthesis and degradation of the components of the cartilaginous extracellular matrix. The processes include the synthesis of collagens, proteoglycans, proteases, protease inhibitors, transcription factors, cytokines, and growth factors. The balance between the anabolic and catabolic processes is influenced by the type of loading that the cartilage experiences. High strain rates cause tissue damage, degradation, decreased matrix production, and apoptosis. While decreased mechanical loading leads to a loss of matrix production. Low frequency oscillatory loads are beneficial, while static loads are detrimental.
Aggrecan and Aggregated Proteoglycans
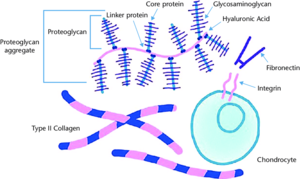
There are three macroclasses of proteins in articular cartilage: collagens (mostly type II collagen); proteoglycans (mostly aggrecan); and other non-collagenous proteins (link protein, fibronectin, matrix protein) and smaller proteoglycans (biglycan, decorin, fibromodulin).[2]
Aggrecan being the major proteoglycan in articular cartilage contains a core protein with numerous covalently attached sulfated glycosaminoglycan (GAG) chains. These GAGs are in the form of chondroitin sulfate and keratan sulfate. A greater proteoglycan concentration provides greater resistance to shear forces. The highest density is found in the middle zone.
Aggrecan doesn't exist in isolation but rather in the form of proteoglycan aggregates. Each aggregate contains a central filament of hyaluronic acid with multiple aggrecan molecules attached non-covalently via one terminus of their core proteins. A link protein stabilises the interaction between the aggrecan and hyaluronic acid.[3]

The core protein of aggrecan contains three disulfide-bonded globular regions which are termed G1, G2, and G3. There are what are called "extended domains" between G1 and G2 called E1 (also called interglobular domain); and between G2 and G3 called E2. [3]
The proximal G1 region resembles an immunoglobulin and is called the immunoglobulin fold (Ig fold). This end is responsible for linking to hyaluronic acid and held to it by a similarly shaped link protein.
The function of G2 is unknown but is structurally similar to G1. There is a short interglobular region (sometimes called E1) between G1 and G2, and this region is a prominent site of proteolysis.[3]
The interglobular region between G2 and G3 is longer (sometimes called E2). It is here that the water trapping glycosaminoglycans chondroitin sulfate and keratan sulfate are attached to the protein core. The term water trapping is used because there the binding process is by both electrostatic and thermodynamic forces. Most keratan sulfate is found in the proximal end of E2, which is called the KS region. All of the chondroitin sulfate is found in the terminal three quarters of E2, of which there are the CS1 and CS2 regions. This area also contains some keratan sulfate.[3]
The G3 region is involved in normal transit of the aggrecan within the chondrocyte and its secretion into the matrix. It also has a role in anchoring aggrecan within the tissue through binding to other proteins such as fibulins and tenascins. G3 is absent in many mature aggrecan molecules due to its protelytic cleavage,[3] but mutations that abolish binding of G3 to fibulins and tenascins leads to familial osteochondritis dissecans.[4]
Dermatosulphate Proteoglycans
Interspersed throughout the matrix are a variety of other proteoglycans. The dermatosulphate proteoglycans are biglycan and decorin. Bogduk includes fibromodulin in this group. These are proteoglycans with a protein core from which stem glycosaminoglycans.
- Biglycan has two glycosaminoglycan chains and it acts as an inhibitor of fibrinogen. Repair involves activation of fibrinogen and deposition of fibrin.
- Decorin can interact with collagen and inhibit fibrillogenesis. Fibrillogenesis is the manufacture of thicker collagen fibres. Decorin can also bind to chondronectin and growth factors such as TGF. It has a wide range of effects including cell growth, differentiation, proliferation, adhesion, spread and migration, and has pro-inflammatory and anti-fibrosis effects.[5]
- Fibromodulin has a protein core and small glycosaminoglycan chain. Fibromodulin sits on the surface of collagen fibres and regulates their assembly. It inhibits the deposition of proto-collagen fibres onto existing collagen fibres.
Collagens
There are a variety of collagens in cartilage that come from various chemical classes of collagen.
Class 1 collagens are the fibril forming collagens, those that can make strings. The main example in articular cartilage is type II collagen which comprises some 90% to 95% of the collagen and is responsible for the tensile strength of the tissue. Type XI collagen is responsible for controlling fibril diameter. Type VI is found in the territorial matrix.
Class 3 collagens are those that form short helices. Type IX collagen is responsible for bridging between itself and type II. Type X is found in zone IV.
Collagen maintains the volume and shape of the matrix because by winding around and entrapping the proteoglycan aggregates it restricts the swelling of the proteoglycans with water imbibement to about 20% of their maximum.
In their relaxed state the aggregates swell as the anionic chondroitin sulfate and keratan sulfate GAG chains draw in water. An equilibrium is reached whereby the swelling is in balance with the tensile forces of the collagen fibrils. With compression, water is displaced, and the GAG chains are brought closer together. This increases their swelling potential and balances the applied load. The increased swelling potential is dissipated when the load is removed, the aggrecan re-swells, and the original equilibrium is restored.[3]
The most important property of collagen is its tensile strength. Collagen buckles when it is compressed. The tensile strength properties of collagen is complementary to proteoglycans which ensure compressive strength, elasticity, and the lifespan of articular cartilage. [2]
For optimal cartilage function and the ability to reach this equilibrium, the cartilage requires a high concentration of aggrecan, a high degree of aggrecan sulfation, and the capacity to form large aggregates. All three of these properties are impaired in osteoarthritis.[3]
Non-collagenous Proteins
The structural glycoproteins are molecules found on the surface of cells referred to as adhesion molecules. They bind chondroblasts to type II collagen. We see an interaction between the cells that produce the matrix and the matrix components itself. The best known structural glycoproteins are chondronectin and anchorin.
Cartilage oligomerix protein (COMP) is also known as thrombospondin 5. It's exact function remains unclear but it appears to be an important regulator of extracellular matrix assembly and stabilisation of the matrix through interacting between collagen fibrils and matrix components. It has been studied as both a diagnostic and prognostic indicator of osteoarthritis; it is significantly upregulated in early osteoarthritis even long before diagnosis.[6]
MMPs
Some of the best known proteolytic enzymes are the matrix metalloproteinases (MMPs), and as indicated by their name occur in the matrix. Metallo refers that these enzymes require zinc as a component that allows them to act on the proteins. Calcium is involved in this interaction.
MMPs are secreted in an inactive form, with proteolytic loss of the propeptide leading to activation in the matrix. For example MMP-1, -2, and -3 are produced as pro-collagenase, pro-gelatinase, and pro-stromelysin, respectively. In contrast, the membrane type MMPs (MT-MMPs) and stomelysin-3 (MMP-11) are secreted as active enzymes. Most MMPs are produced by different connective tissue cells after stimulation by a variety of mediators.[7]
There are some 29 MMPs, and they are divided into four main groups:[4]
- Collagenases: (e.g. MMP-1, -8, -13). These enzymes cleave fibrillar collagens at a single site to produce fragments of three quarters and one quarter of the original size. MMP-13 has the broadest substrate specificity. They have strong activity for cleavage of type II collagen, but other molecules such as types IV and IX collagen, perlecan, osteonectin, and proteoglycan. MMP-1 and MMP-13 are synthesised by macrophages, fibroblasts, and chondrocytes upon stimulation by inflammatory mediators. MMP-8 is predominantly released by neutrophils upon stimulation but also by chondrocytes. All three are present in diseased cartilage.
- Gelatinases: (MMP-2 and -9) These act on breakdown products of type IV and V collagen and elastin. MMP-2 is the most widely expressed.
- Stromelysins: (e.g. MMP-3). These acts on a wide array of extracellular molecules including various collagens, fibronectin, laminin, elastin, and various proteoglycans.
- MT-MMPs (e.g. MMP-14): MMP-14 can initiate activation cascades on the cell surface that activate procollagenases.
ADAMTS and ADAMS
Relatives of the MMPs are the ADAMTS enzymes (short for A Disintegrin And Metalloproteinase with Thrombospondin Motifs) and ADAMs (A Disintegrin And Metalloproteinases). These enzymes are also dependent on zinc. These enzymes were more recently discovered. There are 20 ADAMTS and 33 ADAMS enzymes, with a large number of them having effects on cartilage.
ADAMTS enzymes are involved in both the synthesis and degradation of the extracellular matrix. ADAMTS enzymes include:[4]
- Procollagen propeptidases (ADAMTS-2, -3, and -14) that are involved in the maturation of triple helical collagen fibrils
- Aggrecanases (ADAMTS-1, -4, -5, -9, and -15) that are involved in aggrecan cleavage along with MMPs. ADAMTS5 is about 1,000 times more potent than ADAMTS4.[8]
ADAMTS enzymes are also involved in the cleavage of oligomerix matrix protein, have roles in cartilage metabolism, as well as in chondrocyte differentiation and proliferation. The role that the various ADAMTS and ADAMS enzymes play in joint health and disease is still being studied.[8]
ADAMs are usually membrane-anchored proteinases. It is thought that they play a role in signalling pathways in chondrocytes to fine-tune tissue homeostasis.[9]
Serine Proteinases
Serine proteinases are understudied despite there being almost as many of these as there are MMPs. They are thought to be involved in regulation of cell signalling, modulation of the activity of growth factors, promotion of inflammatory processes, modulation of chemokines, and as a protective feedback mechanism in maintaining cartilage homeostasis.[4]
Matrix Synthesis and Degradation
The chondrocytes slowly but constantly act to have effects in both the synthesis and degradation of the extracellular matrix. Degradation is an important aspect as it allows for old components to be removed to making way for refreshed components. In the normal state there is a balance between synthesis and degradation. If the balance tips to favouring degradation, then degenerative changes occur.
Synthesis is promoted by various growth factors including transforming growth factor (TGF), basic fibroblast growth factor (bFGF), and insulin like growth factor (IGF). Degradation occurs through the action of metalloproteases. MMP-13 plays a central role in degrading type II collagen, while ADAMT-4 and -5 are primary agents that degrade aggrecan. Tumour necrosis factor α interleukin-1 (IL-1) promote the action of metalloproteinases, but degradation also occurs through superoxide (O2−) and nitric oxide.
Synthesis
The chondroblast produces the components of the extracellular matrix. The endoplasmic reticulum within the chondroblast synthesises the various collagens and other proteins of the matrix such as fibromodulin and decorin. At the base of the golgi apparatus there is some endoplasmic reticulum that forms the protein component of the proteoglycans. The carbohydrate component is added to the protein core by the golgi apparatus. Anchorin is an adhesion molecule that sits on the surface of the chondroblast.
The chondroblast can be stimulated by a variety of factors to produce collagen and proteoglycans.[4]
- Fibroblast growth factor (FGF) is an extrinsic regulator that comes from outside the cell and stimulates the nucleus of the chondroblast to produce the protein and proteoglycan components of the matrix.
- Insulin like growth factor (IGF) also comes from the outside, and activates the nucleus by a second messenger to produce the components of the matrix.
- Transforming growth factor (TGF) is produced by the cell itself, and is bound to collagen through decorin. While TGF is buried within the proteoglycans surrounding collagen it can't escape and has no influence. If the proteoglycans are removed and the collagen is exposed, so is TGF, and floats back to the cell where it enhances the effect of FGF through a positive feedback loop. This activates the cell to produce materials, with a preferential effect for the production of proteoglycans, which closes the loop by enclosing collagen and blocking the effect of TGF.
- Bone morphogenic proteins (BMPs): these have direct effects on chondrocytes and are involved in promoting matrix deposition in osteoarthritis (e.g. osteophytosis).
Degradation
Cartilage produce many enzymes that can destroy the matrix. The complete collection of proteases is called the degradome and includes around 588 different proteinases. These include the Matrix Metalloproteinases (MMPs), the A Disintegrin And Metalloproteinase Domain with Thrombospondin Motifs (ADAMTS) family, and the serine proteinases. With the primary structural components of cartilage matrix being collagen and aggrecan, MMP-13 and ADAMTS-4 and -5 play a central role in cartilage degradation.
The ADAMTS are important in the initial degradation of cartilage matrix. ADAMTS-4 and ADAMTS-5 can cleave the interglobular domain between G1 and G2, leaving a shortened aggrecan with decreased numbers of fixed charged groups. This is thought to be a key step in the pathologic loss of aggrecan. They can also cleave several sites close to the G3 domain. Following cleavage between G1 and G2, the G1 domain remains bound to hyaluronic acid can then be cleaved by MMPs. Also of note, the combined action of the ADAMTs aggrecanases and MMPs results in the release of a soluble bioactive peptide that promotes further cartilage breakdown.[4]
MMP-1 and MMP-13 are both relatively specific for action on type II collagen. They act on type II collagen up towards one end. Once the collagen molecule is split, gelatinase acts on the products. MMP-13 is thought to also be involved in matrix turnover in healthy cartilage. MMP-13 (Collagenase-3) is considered to be the major catabolic effector in osteoarthritis, while MMP-1 is thought to be the primary collagenase in rheumatoid arthritis. MMP-13 It has been extensively studied and selective MMP-13 inhibitors for treating osteoarthritis are being developed.[8] The role of MMP-1 in osteoarthritis may vary depending on the joint.[10]
The other components of the matrix are acted on by MMP-3 (stromelysin). MMP-3 is the most highly expressed MMP gene in normal cartilage and remains comparatively high in osteoarthritis. MMP-3 can also cleave aggrecan molecules between G1 and G2. Other processes operate to liberate the link protein and head end of the aggrecan molecule. These products leak into the synovial fluid and removed via transportation through lymph. MMP-3 can act on other collagens within the matrix such as type XI and IX and the terminal ends of type II collagen. MMP-3 can also act on smaller collagens found around the cell such as type XI, and other proteins such as fibronectin. MMP-3 is a good general debriding enzyme. In osteoarthritis there appears to be an excessive degradation of the matrix.
A feature of aging cartilage is the accumulation of hyaluronic acid chains that bear the old remnant head end of the aggrecan molecule, that isn't removed, and this remnant prevents the binding of fresh aggrecan molecules. This contributes to the compromise of articular cartilage with age.
In healthy articular cartilage there the extracellular matrix is slowly but continuously refreshed. Old collagen is removed and replaced by new collagen; old proteoglycans are removed and replaced by new proteoglycans. There is a balance between synthesis and degradation of the matrix.
Tissue inhibitors of metalloproteinases (TIMP) can control the activation of the MMPs and ADAMTS enzymes preventing uninhibited action of these enzymes. With reduced activity of TIMPs there may be excessive degradation for the amount of synthesis occurring.
Cytokines that have an effect on the chondroblast and promote degradation include interleukin (IL), tumour necrosis factor α (TNF), and interferon (IFN). These mediators have two sorts of effects. There is a lesser effect of stimulation of the production of degradative enzymes. The dominant effect is the inhibition of the synthesis of the proteins, collagens, and proteoglycans. Superoxide radicals and nitric oxide also promote degradation. Inflammatory effects do not explain all of the features of the genesis of osteoarthritis.
Synovial Membrane
Intima and Subintima
The term synovium refers to the soft tissue lining of diarthrodial joints, tendon sheaths, and bursae. It contains a surface layer called the intima, and underlying tissue called the subintima. Between the intimal surfaces is a small amount of fluid that is usually rich in hyaluronic acid. The synovium provides a non-adherent surface between tissue elements.[11]
The intima contains macrophages and fibroblasts and is two to three layers of cells thick. The cells aren't continuous like epithelium. Between them runs an amorphous matrix. The gaps between the cells allow easy communication through the intima.
The subintima consists of a loose network of collagen fibres; blood vessels; fat globules; and a variety of cells including mast cells, fibroblasts, and macrophages.
The blood vessels within the subintima produce most of the components by volume of synovial fluid. There is a transudate of fluid and proteins that passes into the joint space to start to produce synovial fluid..
Synovial macrophages
These are also known as macrophage-like synoviocytes (MLS), or type A synoviocytes. These are essentially macrophages. Previously they were thought to arise from bone marrow, but in reality they are derived from embryonic precursor cells and maintained by independent slow proliferation. [12]
They remove debris from the synovial fluid such as degraded aggrecans and other material that interfere with the lubricating property.
They also produce prostaglandins that can affect vasodilation or constriction of the subintimal blood vessels, thereby regulating the production of synovial fluid. For example in inflamed joints, prostaglandin production results in an effusion.
Synovial lining macrophages share certain features in common with epithelial cells. They express tight junction proteins, and provide an anti-inflammatory barrier around the joint that impairs immune cell traffic in a steady state. During arthritis this barrier "cracks" open.[13] Macrophages make up the minority of cells in normal intima, except in inflammatory arthritis where they make up 80% of the intima.[13]
These cells are also involved in the immune system as antigen presenting cells.
Synovial fibroblasts
These are also known as fibroblast-like synoviocytes (FLS), or type B synoviocytes. They are more abundant than synovial macrophages. They are thought to arise from mesenchymal stem cells. [12]
Fibroblasts produce inhibitors of phagocytic enzymes that are in turn produced by macrophages, and thereby prevent excessive activity.
Fibroblasts also secrete lubricin, the obsolete term for this was lubricating glycoprotein (LGP). It is also known as superficial zone protein. Lubricin is the cardinal component of synovial fluid and provides an anti-friction property. Hyaluronic acid and proteins on their own do not have an anti-friction property. Lubricin is also expressed by superficial zone chondrocytes and to a lesser extent intermediate zone chondrocytes.[14]
These cells also produce hyaluronan (note previously thought that this was produced by macrophages).[13]
FLS are involved in many pathological aspects of rheumatoid arthritis and promote synovitis, pannus growth, and cartilage/bone destruction.
Joint Lubrication
- See also: Cartilage Biomechanics
The ability of synovial fluid to lubricate the surface of cartilage depends on Lubricin (superficial zone protein), a glycoprotein located on the surface of the synovium and cartilage.
Hyaluronan is the main factor that is responsible for retaining a constant volume of fluid during exercise. The fluid cushions the synovial tissue and acts as a reservoir for lubricant for the cartilage. Mechanical stimulation of synovial fibroblasts is likely a key factor for stimulating the synthesis of hyaluronan. So when there is a large volume of synovial fluid, there is decreased mechanical stimulation and hence reduced synthesis, and vice versa.
Joint effusions can be created by two mechanisms, but they are not necessarily distinct. Osteoarthritis can display both mechanisms.
- Mechanical irritation: such as in osteoarthritis, there is excessive production of hyaluronan by synovial fibroblasts through frictional forces.
- Synovitis: this occurs through the accumulation of exudate, i.e. inflammatory oedema through increased vascular permeability.
List of Synovial Joint
| Synovial Joint | Joint type | Bones | Ligaments | Muscles | Innervation | Vasculature | ROM | Volume |
|---|---|---|---|---|---|---|---|---|
| Acromioclavicular Joint | Planar Joint | Clavicle Scapula | Coracoclavicular, coracoacromial, superior acromioclavicular, and inferior acromioclavicular ligaments. | No muscles directly act on this joint. | Axillary, suprascapular, and lateral pectoral nerves | Suprascapular and thoracoacromial arteries | Upward rotation: 30 degrees, external rotation:8 degrees | 2mL |
| Atlanto-axial Joint | Pivot Joint | C1 (Atlas) C2 (Axis) | C2 | Rotation ~45° each way, flexion-extension ~10° each way, and lateral flexion ~5° each way | ||||
| Atlanto-occipital Joint | Condyloid Joint | C1 (Atlas) Occiput | Two articular capsules, posterior atlanto-occipital membrane, anterior atlanto-occipital membrane | Flexion by longi capitis and recti capitis anteriores; extension by recti capitis posteriores major and minor, the obliquus capitis superior, the semispinalis capitis, splenius capitis, sternocleidomastoid, and upper fibres of the trapezius. | C1 | Anastomosis between the deep cervical, occipital and vertebral arteries. | 3.5 flexion, 21 extension, 10.9 lateral flexion each way, 6.7 rotation each way | |
| Cervical Zygapophyseal (Facet) Joint | Planar Joint | |||||||
| Distal Radioulnar Joint | Pivot Joint | Radius Ulna | Triangular, anterior distal radioulnar, and posterior distal radioulnar ligaments | Pronation: pronator quadratus, pronator teres; Supination: supinator, biceps brachii | Anterior and posterior interosseous nerves | Anterior and posterior interosseous arteries | ||
| Elbow Joint | Hinge Joint | Radius Ulna Humerus | Capsule, medial and lateral collateral ligaments, oblique cord, quadrate ligament | Radial, ulnar, median, and musculocutaneous nerves | Anastomotic arcades formed by branches of radial, ulnar, and brachial arteries. | |||
| First Carpometacarpal Joint (Trapeziometacarpal Joint) | Saddle Joint | Metacarpal Trapezium | Capsule, anterior oblique, ulnar collateral, first intermetacarpal, posterior oblique, dorsoradial ligaments. | Lateral antebrachial cutaneous nerve, palmar cutaneous branch of the median nerve, superficial radial nerve | First dorsal metacarpal branch of the radial artery | 53° of flexion/extension, 42° of abduction/adduction, and 17° of rotation | ||
| Glenohumeral Joint | Ball and Socket Joint | Humerus Scapula | Capsule, glenohumeral, coracohumeral and transverse humeral ligaments | abduction: deltoid assisted by the supraspinatus; adduction: short scapular muscles (except supraspinatus) when the deltoid relaxes. Assisted by the pectoralis major and latissimus dorsi; flexion: clavicular head of the pectoralis major and the anterior fibres of the deltoid, assisted by the coracobrachialis and biceps; extension: latissimus dorsi, posterior fibres of the deltoid and the long head of the triceps; rotation: lateral rotation: infraspinatus and teres minor, medial rotation: subscapularis and teres major | suprascapular, subscapular, axillary and lateral pectoral nerves | anterior and posterior humeral circumflex, and subscapular arteries | arm flexion, extension, adduction, abduction, and internal and external rotation | |
| Hip Joint | Ball and Socket Joint | Ilium Femur | Ischiofemoral, iliofemoral, pubofemoral, transverse acetabular, and ligamentum teres | 27 musculotendinous units are involved in hip function | Femoral, obturator and superior gluteal nerves, and nerve to quadratus femoris | Branches of the medial and lateral circumflex femoral, superior and inferior gluteal arteries and obturator arteries | Flexion 140°, extension 20°, Internal rotation 30°, external rotation 40°, abduction 50°, adduction 30° | 1-10mL |
| Interphalangeal Joints (Foot) | Hinge Joint | Proximal Phalanx (Foot) Distal Phalanx (Foot) | ||||||
| Knee Joint | Saddle Joint Hinge Joint | Tibia Femur Patella | Popliteal nerve, tibial nerve | Genicular branches of the popliteal artery | Mainly sagittal plane: 3° of hyperextension to 155° of flexion | |||
| Lumbar Zygapophyseal (Facet) Joint | Planar Joint | Vertebra | Capsular Ligament | Medial Branches of the Dorsal Rami | Branches of Lumbar Arteries | Limited Flexion, Extension, Lateral Flexion, and Rotation | ||
| Metacarpophalangeal Joint | Condyloid Joint | Metacarpal Proximal Phalanx (Hand) | Capsule, two collateral ligaments, palmar (volar) ligament | Digital nerves from the ulnar and median nerves | Deep digital arteries from the superficial palmar arch | |||
| Metatarsophalangeal Joints | Condyloid Joint | Metacarpal Proximal Phalanx (Foot) | Capsule, collateral ligamentous complexes, plantar plate. For great toe also sesamoid-phalangeal ligaments. | flexor digitorum longus, flexor digitorum brevis, extensor digitorum longus, extensor digitorum brevis, flexor digiti minimi brevis, abductor digiti minimi, dorsal and plantar Interossei, lumbricals | Digital nerves from the ulnar and median nerves | Deep digital arteries from the superficial palmar arch | ||
| Proximal Radioulnar Joint | Pivot Joint | Radius Ulna | Annular ligament | Articular branches of the musculocutaneous, median, and radial nerve | Radial portion of the peri-articular arterial anastomosis of the elbow joint | |||
| Radiocarpal Joint | Condyloid Joint | Radius Ulna Scaphoid Lunate Triquetrum | Volar: radial collateral ligament to styloid process, radioscaphocapitate, ligament radiolunate ligament, radioscapholunate ligament; Dorsal: radioscaphoid ligament, radiolunate ligament, radiotriquetral ligament | flexor digitorum superficialis, flexor digitorum profundus, palmaris longus, flexor carpi radialis and ulnaris, extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digitorum, flexor carpi ulnaris, extensor carpi ulnaris, extensor carpi radialis longus and brevis, flexor carpi radialis | anterior interosseous nerve arising from median nerve (C5-T1), posterior interosseous nerve arising from radial nerve (C7-C8) | Palmar carpal arch (from palmar carpal branches of radial and ulnar arteries, reinforced by anterior interosseous artery and penetrating deep branches of deep palmar arch), dorsal carpal arch (formed by dorsal carpal branches of radial and ulnar arteries, reinforced by anterior and posterior interosseous arteries) | ||
| Sacroiliac Joint | Ilium Sacrum | Anterior sacroiliac, interosseous sacroiliac, posterior sacroiliac, long posterior sacroiliac, sacrotuberous, sacrospinous, and iliolumbar ligaments. | Posterior joint lateral branches of the posterior rami of L5-S4. Anterior joint L4-S3 (+/- L3, sacral plexus, superior gluteal nerve) | Median sacral artery and the lateral sacral branches of the internal iliac artery | 0-2° | 1 - 1.5 mLs | ||
| Sternoclavicular Joint | Saddle Joint | Clavicle Rib 1 Manubrium | Sternoclavicular, costoclavicular, interclavicular ligs. | Medial supraclavicular (C3-4) and subclavian (C5-6) nn. | Internal thoracic and suprascapular aa. (branches of the subclavian a.) | 35° in the horizontal and coronal planes, 70° range of motion anteroposteriorly, 50° of rotation along its long axis. | ||
| Talocalcaneal Joint (Subtalar Joint) | Planar Joint | Talus Calcaneus | Multiple, interosseous talocalcaneal ligament is most important | Medial plantar, lateral plantar, and deep fibular nerves | Posterior tibial and fibular arteries | Equal components of inversion/eversion and abduction/adduction. | ||
| Tibiotalar Joint (Talocrural Joint) | Hinge Joint | Tibia Fibula Talus | Syndesmosis, medial collateral ligaments, lateral collateral ligaments | tibial nerve, deep peroneal nerve | anterior and posterior tibial arteries, peroneal artery | 10° to 20° of dorsiflexion, 40° to 55° of plantarflexion | 16-30 mL |
Resources
See Also
References
- ↑ Jaumard, Nicolas V et al. “Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions.” Journal of biomechanical engineering vol. 133,7 (2011): 071010. doi:10.1115/1.4004493
- ↑ 2.0 2.1 2.2 2.3 Eschweiler J, Horn N, Rath B, Betsch M, Baroncini A, Tingart M, Migliorini F. The Biomechanics of Cartilage-An Overview. Life (Basel). 2021 Apr 1;11(4):302. doi: 10.3390/life11040302. PMID: 33915881; PMCID: PMC8065530.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Roughley, P.J., Mort, J.S. The role of aggrecan in normal and osteoarthritic cartilage. J EXP ORTOP 1, 8 (2014). https://doi.org/10.1186/s40634-014-0008-7
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Hochberg, Marc C., et al. Rheumatology. Philadelphia, PA: Elsevier, 2019.
- ↑ Zhang, Wen et al. “Decorin is a pivotal effector in the extracellular matrix and tumour microenvironment.” Oncotarget vol. 9,4 5480-5491. 3 Jan. 2018, doi:10.18632/oncotarget.23869
- ↑ Tseng, Susan et al. “Cartilage Oligomeric Matrix Protein (COMP): A Biomarker of Arthritis.” Biomarker insights vol. 4 33-44. 17 Feb. 2009, doi:10.4137/bmi.s645
- ↑ Brandon J. Rose, David L. Kooyman, "A Tale of Two Joints: The Role of Matrix Metalloproteases in Cartilage Biology", Disease Markers, vol. 2016, Article ID 4895050, 7 pages, 2016. https://doi.org/10.1155/2016/4895050
- ↑ 8.0 8.1 8.2 Yang CY, Chanalaris A, Troeberg L. ADAMTS and ADAM metalloproteinases in osteoarthritis - looking beyond the 'usual suspects'. Osteoarthritis Cartilage. 2017 Jul;25(7):1000-1009. doi: 10.1016/j.joca.2017.02.791. Epub 2017 Feb 13. PMID: 28216310; PMCID: PMC5473942.
- ↑ Yang, C-Y et al. “ADAMTS and ADAM metalloproteinases in osteoarthritis - looking beyond the 'usual suspects'.” Osteoarthritis and cartilage vol. 25,7 (2017): 1000-1009. doi:10.1016/j.joca.2017.02.791
- ↑ Kevorkian L, Young DA, Darrah C, Donell ST, Shepstone L, Porter S, Brockbank SM, Edwards DR, Parker AE, Clark IM. Expression profiling of metalloproteinases and their inhibitors in cartilage. Arthritis Rheum. 2004 Jan;50(1):131-41. doi: 10.1002/art.11433. PMID: 14730609.
- ↑ Smith, Malcolm D. “The normal synovium.” The open rheumatology journal vol. 5 (2011): 100-6. doi:10.2174/1874312901105010100
- ↑ 12.0 12.1 Tu J, Hong W, Zhang P, Wang X, Körner H, Wei W. Ontology and Function of Fibroblast-Like and Macrophage-Like Synoviocytes: How Do They Talk to Each Other and Can They Be Targeted for Rheumatoid Arthritis Therapy? Front Immunol. 2018 Jun 26;9:1467. doi: 10.3389/fimmu.2018.01467. PMID: 29997624; PMCID: PMC6028561.
- ↑ 13.0 13.1 13.2 Collison, J. Synovial macrophages shield the joints. Nat Rev Rheumatol 15, 573 (2019). https://doi.org/10.1038/s41584-019-0295-6
- ↑ Jay GD, Waller KA. The biology of lubricin: near frictionless joint motion. Matrix Biol. 2014 Oct;39:17-24. doi: 10.1016/j.matbio.2014.08.008. Epub 2014 Aug 27. PMID: 25172828.