Thoracic Outlet Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
}} | }} | ||
'''Thoracic outlet syndrome''' (TOS) is caused by compression of the brachial plexus or subclavian vessels as they pass through the narrow passageways leading from the base of the neck to the axilla and arm. There is considerable disagreement about its diagnosis and treatment, particularly the neurogenic form. | '''Thoracic outlet syndrome''' (TOS) is caused by compression of the brachial plexus or subclavian vessels as they pass through the narrow passageways leading from the base of the neck to the axilla and arm. There is considerable disagreement about its diagnosis and treatment, particularly the neurogenic form. Practice guidelines are not currently possible due to the low level of evidence.<ref name=":0" /> | ||
== Anatomy == | == Anatomy == | ||
| Line 69: | Line 69: | ||
Thoracic outlet syndrome is divided into:<ref name=":0" /> | Thoracic outlet syndrome is divided into:<ref name=":0" /> | ||
*'''Neurogenic''' '''(ATOS)''': Caused by compression of the inferior trunk of the brachial plexus due to a cervical rib, band, or enlarged scalenus muscles. | *'''Neurogenic''' '''(ATOS)''': Caused by compression of the inferior trunk of the brachial plexus due to a cervical rib, band, or enlarged scalenus muscles. This is the most common form. | ||
**'''NPMS''': Neurogenic pectoralis minor syndrome is a subgroup with compression at the pectoralis minor space. If limited to the scalene triangle it is called NTOS. It combined then it is called '''NTOS/NPMS.''' | **'''NPMS''': Neurogenic pectoralis minor syndrome is a subgroup with compression at the pectoralis minor space. If limited to the scalene triangle it is called NTOS. It combined then it is called '''NTOS/NPMS.''' | ||
* '''Arterial Thoracic Outlet Syndrome (NTOS)''': Caused by objective compression of the subclavian artery at the interscalene triangle. | * '''Arterial Thoracic Outlet Syndrome (NTOS)''': Caused by objective compression of the subclavian artery at the interscalene triangle. | ||
| Line 87: | Line 87: | ||
=== History === | === History === | ||
''' | '''NTOS''': The patient may have pain, numbness, tingling, and weakness. Symptoms are worse when working with the arm above horizontal. | ||
The pain is dull and aching in nature and may occur in the shoulder and upper arm, chest, axilla, and neck. The pain may radiate distally to the medial arm, lateral shoulder, and dorsal forearm. Pain can occur at night. | |||
Ask about occupation and any potentially relevant aggravating factors such as sporting activities, driving, prolonged typing, etc. Ask about arm dominance. | |||
Numbness and paraesthesias of the arm usually the medial arm and hand (4th and 5th fingers). There may be weakness in the shoulders, arm, and hands. | |||
Arterial signs and symptoms can be present in patients with NTOS. However ATOS is not diagnosis unless there is proven symptomatic ischaemia. VTOS is less commonly seen in conjunction with NTOS. | |||
'''VTOS:''' Presents as acute or chronic upper extremity deep venous thrombosis (Paget-Schroetter syndrome, effort thrombosis), or positional swelling (McCleery syndrome) | '''VTOS:''' Presents as acute or chronic upper extremity deep venous thrombosis (Paget-Schroetter syndrome, effort thrombosis), or positional swelling (McCleery syndrome) | ||
| Line 99: | Line 103: | ||
===Examination=== | ===Examination=== | ||
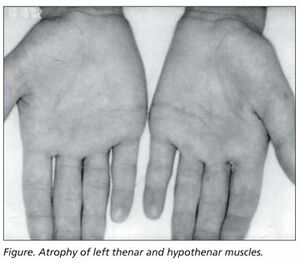
[[File:Gillat-Sumner hand.jpg|thumb|Wasting of the left thenar and hypothenar muscles]] | [[File:Gillat-Sumner hand.jpg|thumb|Wasting of the left thenar and hypothenar muscles]] | ||
There may be tenderness in the | '''NTOS:''' There may be tenderness in the scalene triangle (NTOS), pectoralis minor insertion site (NPMS), and axilla. Pressure over the scalene triangle or pectoralis minor insertion site may reproduce symptoms. | ||
Weakness and/or paraesthesias can occur with arm elevation, pallor of the palm with arm elevation and fingers pointing to the ceiling, and weakness of the 5th finger. The patient may have the Gilliat-Sumner hand in which there is severe wasting in the fleshy base of the thumb. Atrophy of abductor pollicis brevis may mimic [[Carpal Tunnel Syndrome]]. | |||
CRPS like signs can occur with stellate ganglion compression such as swelling of the extremities and fingers. | CRPS like signs can occur with stellate ganglion compression such as swelling of the extremities and fingers. | ||
| Line 109: | Line 113: | ||
There may be restricted abduction and internal rotation of the ipsilateral shoulder. | There may be restricted abduction and internal rotation of the ipsilateral shoulder. | ||
There are a variety of special tests (Table 1) | Examine for Tinel signs along the radial, ulnar, and median nerves. | ||
There are a variety of special tests (Table 1). The validity and reliability are hampered by the lack of a gold standard for diagnosis. | |||
=== Special Tests === | |||
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
|+Table 1. Thoracic Outlet Syndrome test performances<ref>{{#pmid:11707008}}</ref> {{CEBM|4}} | |+Table 1. Thoracic Outlet Syndrome test performances<ref>{{#pmid:11707008}}</ref> {{CEBM|4}} | ||
| Line 151: | Line 159: | ||
|[https://www.youtube.com/watch?v=e-6AiDPyd2Q Wright test] (sx reproduction)|| 0.90|| 0.29|| 1.3|| 0.3|| | |[https://www.youtube.com/watch?v=e-6AiDPyd2Q Wright test] (sx reproduction)|| 0.90|| 0.29|| 1.3|| 0.3|| | ||
|- | |- | ||
| Roos | | [https://www.youtube.com/watch?v=rM4fB-t_l9E Elevated Arm Stress Test/Roos (EAST)]|| 0.84|| 0.30|| 1.2|| 0.5|| | ||
|} | |} | ||
'''Elevation arm stress test (EAST)''': Also called Roos test. This test is used to assess for narrowing of the scalene triangle. The shoulders are abducted to 90 degrees and extended, and the elbows flexed to 90 degrees. The hands are rapidly opened and closed for up to three minutes. A positive test is reproduction of local or distal pain and neurologic symptoms. Record the time to onset of symptoms and what symptoms occured. | |||
'''Upper limb tension test (ULTT)''': This is comparable to the straight leg raise of the lower limbs. It can be tested with one arm at a time or both arms at the same time to allow for easier comparison. There are three sequences, each progressively increasing tension on the brachial plexus (except the last bullet point) | |||
* The arms are abducted to 90 degrees with the elbows extended and palms facing down. | |||
* The wrists are dorsiflexed. | |||
* The head is laterally flexed away from the symptomatic side. | |||
* The elbow can then be flexed. If symptoms come on at this point then cubital tunnel syndrome shoulder be considered. | |||
== Investigations == | == Investigations == | ||
'''Plain films''': Chest and cervical spine xrays should be requested to assess for cervical rib or elongated C7 transverse process. | |||
'''[[Nerve Conduction Studies|Electrophysiological]] tests:''' These are typically normal below the clavicle and are not required for diagnosis unless a specific disorder other than NTOS is suspected. However in some cases there may be the following findings in classic neurogenic TOS: | |||
* Low compound muscle action potential in the thenar and intrinsic muscles | * Low compound muscle action potential in the thenar and intrinsic muscles | ||
* Abnormal sensory nerve conduction in the ulnar nerve | * Abnormal sensory nerve conduction in the ulnar nerve | ||
| Line 162: | Line 179: | ||
* Abnormal medial antebrachial cutaneous sensory nerve conduction) | * Abnormal medial antebrachial cutaneous sensory nerve conduction) | ||
'''Other:''' Venous and arterial anatomy can be assessed by catheter angiography, doppler, or MR angiography and venography. | |||
Venous and arterial anatomy can be assessed by catheter angiography, doppler, or MR angiography and venography. | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Revision as of 06:59, 20 February 2022
Thoracic outlet syndrome (TOS) is caused by compression of the brachial plexus or subclavian vessels as they pass through the narrow passageways leading from the base of the neck to the axilla and arm. There is considerable disagreement about its diagnosis and treatment, particularly the neurogenic form. Practice guidelines are not currently possible due to the low level of evidence.[1]
Anatomy
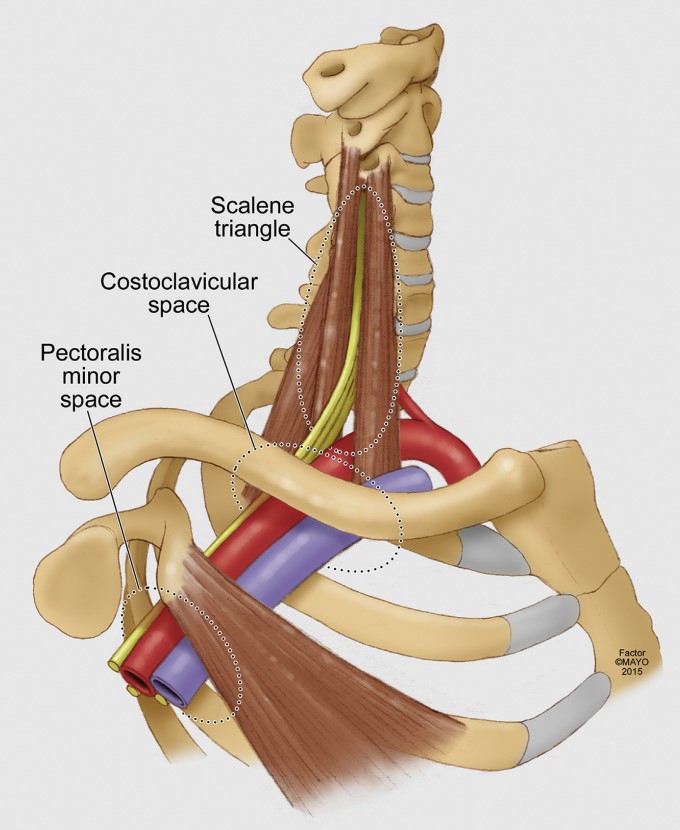
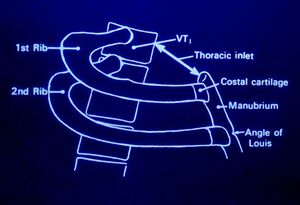
The thoracic outlet is found at the base of the neck. It consists of the first rib and adjacent structures. The upper thoracic aperture is bordered by:
- Posteriorly - spine
- Anteriorly - manubrium
- Laterally - 1st rib
The stellate ganglion sits posterior to the subclavian artery. It is anterior to the 1st rib, transverse process of C7, and the anterior primary rami of C8 and T1. It receives white rami communicantes from C8 and T1 (afferent sympathetic fibres from the brachial plexus and upper intercostal nerves). It sends grey rami communicantes to C8 and T1 (efferent sympathetic fibres to brachial plexus and intercostal nerves)
Pathophysiology
Thoracic outlet syndrome is caused by an enlargement or change of the tissues in or near the thoracic outlet leading to neurovascular compression.
Neurovascular compression can occur at three different anatomic levels
- Interscalene triangle (between the scalene muscles)
- Costoclavicular space (between the first rib and clavicle)
- Pectoralis minor space (under the pectoralis minor)
NTOS: brachial plexus compression can occur at the interscalenne triangle or the pectoralis minor space.
VTOS: Venous compression occurs most commonly at the costoclavicular space, but can occasionally occur at the pectoralis minor space.
ATOS: Arterial compression occurs most commonly at the scalene triangle typically by an anomalous bone or ligamentous structure.[1]
Various causes have been proposed including
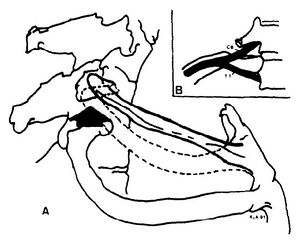
- Anomalous scalene bands. fibrous band may extend from the tip of the abnormal transverse process to the first rib.
- Anomaly or fracture of 1st rib
- Cervical rib
- Fracture clavicle
- 1st rib dysfunction. Subluxation cranially at the costotransverse joint leading to irritation of the nerve roots C8 and T1 as well as the stellate ganglion.
- Myofascial dysfunction and pain (scalenes, pectoralis minor, infraspinatus, teres minor). Restriction of internal rotation can be seen, this may be due to the fact that the axillary nerve C5/6 comes off the posterior cord (teres minor and deltoid)
- Tumour
- Repetitive trauma
- Stellate ganglion irritation causing autonomic symptoms/signs.
Often there is no direct cause.
Note that anomalies of the thoracic outlet are also common in asymptomatic individuals. In a study of 50 cadavers only 10% had a bilaterally normal anatomy.[2]
Classification
Thoracic outlet syndrome is divided into:[1]
- Neurogenic (ATOS): Caused by compression of the inferior trunk of the brachial plexus due to a cervical rib, band, or enlarged scalenus muscles. This is the most common form.
- NPMS: Neurogenic pectoralis minor syndrome is a subgroup with compression at the pectoralis minor space. If limited to the scalene triangle it is called NTOS. It combined then it is called NTOS/NPMS.
- Arterial Thoracic Outlet Syndrome (NTOS): Caused by objective compression of the subclavian artery at the interscalene triangle.
- Venous Thoracic Outlet Syndrome (VTOS): Caused by compression of the subclavian vein at the costoclavicular junction, or occasionally at the pectoralis minor space.
- Paget-Schroetter syndrome: thrombotic occlusion at the costoclavicular junction, also called effort thrombosis
- McCleeery syndrome: intermittent positional obstruction in the absence of thrombosis
- VPMS: subgroup where the compression is limited to the pectoralis minor space. If limited to the costoclavicular junction it is called VTOS. If combined it is called VTOS/VPMS.
- Persistent TOS: Of any type, means that it hasn't improved after treatment
- Recurrent TOS: Symptoms have recurred after an initial three month period of improvement.
- Secondary TOS: Symptoms of a different type have occurred after treatment of a different problem.
The following terms should not be used: True, disputed, or nonspecific NTOS, vascular TOS, mixed TOS, Roos classification.
Epidemiology
The condition is more common in women. The onset of symptoms usually occurs between 20 and 50 years of age
Clinical Features
History
NTOS: The patient may have pain, numbness, tingling, and weakness. Symptoms are worse when working with the arm above horizontal.
The pain is dull and aching in nature and may occur in the shoulder and upper arm, chest, axilla, and neck. The pain may radiate distally to the medial arm, lateral shoulder, and dorsal forearm. Pain can occur at night.
Ask about occupation and any potentially relevant aggravating factors such as sporting activities, driving, prolonged typing, etc. Ask about arm dominance.
Numbness and paraesthesias of the arm usually the medial arm and hand (4th and 5th fingers). There may be weakness in the shoulders, arm, and hands.
Arterial signs and symptoms can be present in patients with NTOS. However ATOS is not diagnosis unless there is proven symptomatic ischaemia. VTOS is less commonly seen in conjunction with NTOS.
VTOS: Presents as acute or chronic upper extremity deep venous thrombosis (Paget-Schroetter syndrome, effort thrombosis), or positional swelling (McCleery syndrome)
ATOS: Presents as either symptomatic ischaemia with arm elevation or fixed arterial injury (stenosis, occlusion, or aneurysm).
Examination
NTOS: There may be tenderness in the scalene triangle (NTOS), pectoralis minor insertion site (NPMS), and axilla. Pressure over the scalene triangle or pectoralis minor insertion site may reproduce symptoms.
Weakness and/or paraesthesias can occur with arm elevation, pallor of the palm with arm elevation and fingers pointing to the ceiling, and weakness of the 5th finger. The patient may have the Gilliat-Sumner hand in which there is severe wasting in the fleshy base of the thumb. Atrophy of abductor pollicis brevis may mimic Carpal Tunnel Syndrome.
CRPS like signs can occur with stellate ganglion compression such as swelling of the extremities and fingers.
The first rib should be examined. The patient is seated as for examination of the cervical spine. Lateral flexion is tested bilaterally. With the head in lateral flexion, the supraclavicular area on the side of flexion is palpated. The first rib is located medially in the supraclavicular area. The patient is asked to breathe in, and the first rib rises against the pressure of the examining finger. Pain may be elicited locally. Paraesthesiae in the C8 or T1 areas may be reported.
There may be restricted abduction and internal rotation of the ipsilateral shoulder.
Examine for Tinel signs along the radial, ulnar, and median nerves.
There are a variety of special tests (Table 1). The validity and reliability are hampered by the lack of a gold standard for diagnosis.
Special Tests
| Thoracic Outlet Syndrome Tests | |||||
|---|---|---|---|---|---|
| Test | Sensitivity | Specificity | +LR | -LR | Kappa |
| Cervical Rotation Lateral Flexion Test[4] | 0.92 | 0.90 | 9.2 | 0.09 | 1.0 |
| Both Adson + Wright (pulse) positive | 0.54 | 0.94 | 9.0 | 0.5 | |
| Both Adson + hyperabduction (sx) positive | 0.72 | 0.88 | 6 | 0.3 | |
| Hyperabduction (pulse abolition) | 0.52 | 0.90 | 5.2 | 0.5 | |
| Both Adson + Roos positive | 0.72 | 0.82 | 4 | 0.3 | |
| Both Adson + Wright (sx) positive | 0.79 | 0.76 | 3.3 | 0.3 | |
| Both Adson + Roos positive | 0.72 | 0.82 | 4 | 0.3 | |
| Adson test | 0.79 | 0.76 | 3.3 | 0.3 | |
| Tinel sign | 0.86 | 0.56 | 2.0 | 0.3 | |
| Both Wright (pulse) + hyperabduction (sx) positive | 0.63 | 0.69 | 2.0 | 0.5 | |
| Both Wright (sx) + hyperabduction (sx) positive | 0.83 | 0.50 | 1.7 | 0.3 | |
| Both Wright (sx) + Roos positive | 0.83 | 0.47 | 1.6 | 0.4 | |
| Wright test (pulse abolition) | 0.70 | 0.53 | 1.5 | 0.6 | |
| Hyperabduction (sx reproduction) | 0.84 | 0.40 | 1.4 | 0.4 | |
| Wright test (sx reproduction) | 0.90 | 0.29 | 1.3 | 0.3 | |
| Elevated Arm Stress Test/Roos (EAST) | 0.84 | 0.30 | 1.2 | 0.5 | |
Elevation arm stress test (EAST): Also called Roos test. This test is used to assess for narrowing of the scalene triangle. The shoulders are abducted to 90 degrees and extended, and the elbows flexed to 90 degrees. The hands are rapidly opened and closed for up to three minutes. A positive test is reproduction of local or distal pain and neurologic symptoms. Record the time to onset of symptoms and what symptoms occured.
Upper limb tension test (ULTT): This is comparable to the straight leg raise of the lower limbs. It can be tested with one arm at a time or both arms at the same time to allow for easier comparison. There are three sequences, each progressively increasing tension on the brachial plexus (except the last bullet point)
- The arms are abducted to 90 degrees with the elbows extended and palms facing down.
- The wrists are dorsiflexed.
- The head is laterally flexed away from the symptomatic side.
- The elbow can then be flexed. If symptoms come on at this point then cubital tunnel syndrome shoulder be considered.
Investigations
Plain films: Chest and cervical spine xrays should be requested to assess for cervical rib or elongated C7 transverse process.
Electrophysiological tests: These are typically normal below the clavicle and are not required for diagnosis unless a specific disorder other than NTOS is suspected. However in some cases there may be the following findings in classic neurogenic TOS:
- Low compound muscle action potential in the thenar and intrinsic muscles
- Abnormal sensory nerve conduction in the ulnar nerve
- Prolonged F-wave latency in the ulnar nerve
- Abnormal medial antebrachial cutaneous sensory nerve conduction)
Other: Venous and arterial anatomy can be assessed by catheter angiography, doppler, or MR angiography and venography.
Differential Diagnosis
- Rotator Cuff Tendinopathy
- Cervical disc disorders
- C7 or C8 nerve root compression
- Ulnar neuropathy
- Carpal Tunnel Syndrome
- Fibromyalgia
- Multiple Sclerosis
- CRPS
- Neuralgic Amyotrophy
- Syringomyelia
Diagnosis
NTOS: The diagnosis of NTOS can be made when three of the following four criteria are present:[1]
- LOCAL FINDINGS:
- History: Symptoms consistent with irritation or inflammation at the site of compression (scalene triangle for NTOS, and pectoralis insertion for NPMS), plus symptoms due to referred pain. Patients may have pain in the chest, axilla, upper back, shoulder, trapezius, neck, or head.
- Examination: Tenderness of the affected area.
- PERIPHERAL FINDINGS:
- History: Arm or hand symptoms consistent with proximal nerve compression. Symptoms include numbness, pain, paraesthesias, vasomotor changes, and weakness. Muscle wasting can occur in extreme. Symptoms are exacerbated by movements that either narrow the thoracic outlet (lifting arms overhead) or stretch the brachial plexus (dangling, driving, walking/running).
- Examination: Reproduction of peripheral symptoms with palpation of the affected area (scalene triangle or pectoralis minor insertion site). The EAST or ULTT test may provoke symptoms.
- ABSENT FINDINGS:
- Cervical disc disease, shoulder disease, carpal tunnel syndrome, chronic regional pain syndrome, brachial neuritis.
- INJECTION:
- Response to a properly performed test injection
Treatment
Nonsurgical treatment
Malfunction of the first rib: isometric contraction of scalenus anterior and medius results in elevation of the first rib anteriorly, and reduces posterior subluxation. The therapist places their hand over the lateral head with the patient in a seated position. The patient contracts against the therapists hand. Gentle mobilisations are done over 20 seconds.
Postural dysfunction: Spinal postural stability; release tight pectoralis minor (pec minor may be tight without 1st rib dysfunction with arm elevation), scalene and shoulder girdle muscles (e.g. infraspinatus and teres minor); maintain cervicothoracic mobility; strengthen scapula muscles, lower and middle trapezius, and serratus anterior; strengthen rotator cuff; address ergonomic factors; address work behaviour factors.
Injections:
See Also
Reporting standards are by Illig et al. [1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Illig et al.. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. Journal of vascular surgery 2016. 64:e23-35. PMID: 27565607. DOI.
- ↑ Juvonen T, Satta J, Laitala P, Luukkonen K, Nissinen J. Anomalies at the thoracic outlet are frequent in the general population. Am J Surg. 1995 Jul;170(1):33-7. doi: 10.1016/s0002-9610(99)80248-7. PMID: 7793491.
- ↑ Gillard et al.. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint bone spine 2001. 68:416-24. PMID: 11707008. DOI.
- ↑ Lindgren KA, Leino E, Manninen H. Cervical rotation lateral flexion test in brachialgia. Arch Phys Med Rehabil. 1992 Aug;73(8):735-7. PMID: 1642524.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,