Thoracic Outlet Syndrome
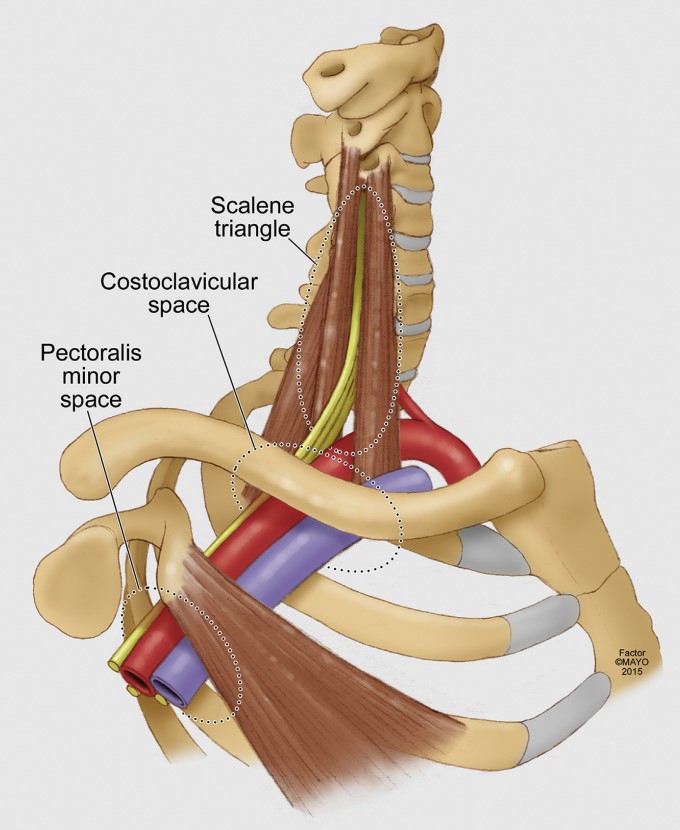
Thoracic outlet syndrome is caused by compression of the brachial plexus or subclavian vessels as they pass through the narrow passageways leading from the base of the neck to the axilla and arm. There is considerable disagreement about its diagnosis and treatment.
Anatomy
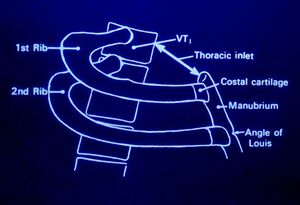
The upper thoracic aperture is bordered by
- Posteriorly - spine
- Anteriorly - manubrium
- Laterally - 1st rib
Aetiology
Thoracic outlet syndrome is caused by an enlargement or change of the tissues in or near the thoracic outlet. Various causes have been proposed including
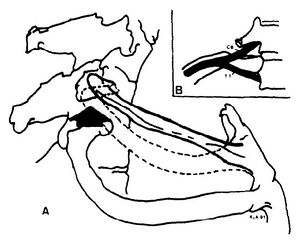
- Anomalous scalene bands. fibrous band may extend from the tip of the abnormal transverse process to the first rib.
- Anomaly or fracture of 1st rib
- Cervical rib
- Fracture clavicle
- 1st rib dysfunction. Subluxation cranially at the costotransverse joint leading to irritation of the nerve roots C8 and T1 as well as the stellate ganglion.
- Myofascial dysfunction and pain
- Tumour
- Repetitive trauma
Often there is no direct cause.
Note that anomalies of the thoracic outlet are also common in asymptomatic individuals. In a study of 50 cadavers only 10% had a bilaterally normal anatomy.[1]
Classification
Thoracic outlet syndrome is divided into
- Vascular (vTOS) : Caused by compression of the subclavian artery or vein.
- Neurogenic (nTOS): Caused by compression of the inferior trunk of the brachial plexus due to a cervical rib, band, or enlarged scalenus muscles.
- Disputed or painful form. There is no neurological deficit but the patient experiences neurological symptoms and pain.
Epidemiology
The condition is more common in women. The onset of symptoms usually occurs between 20 and 50 years of age
Clinical Features
History
Pain: Pain is dull and aching in nature and may occur in the shoulder and upper arm, chest, axilla, and neck. The pain may radiate distally to the medial arm, lateral shoulder, and dorsal forearm. Pain can occur at night.
Neurological symptoms: Numbness and paraesthesias of the arm usually the medial arm and hand (4th and 5th fingers). There may be weakness in the shoulders, arm, and hands.
Vascular: There may be swelling (tight rings), coldness and discoloration in the right arm/hand
General: Symptoms are worse when working with the arm above horizontal.
There may be restricted abduction and internal rotation of the ipsilateral shoulder.
Examination
There may be tenderness in the supraclavicular area, weakness and/or paraesthesias with arm elevation, pallor of the palm with arm elevation and fingers pointing to the ceiling, and weakness of the 5th finger.
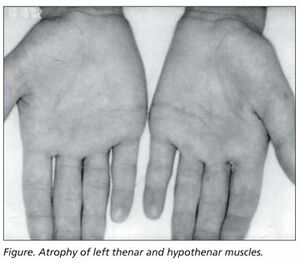
In neurogenic thoracic outlet syndrome the patient may have the Gilliat-Sumner hand in which there is severe wasting in the fleshy base of the thumb. Atrophy of abductor pollicis brevis may mimic Carpal Tunnel Syndrome.
CRPS like signs can occur with stellate ganglion compression such as swelling of the extremities and fingers.
The first rib should be examined. The patient is seated as for examination of the cervical spine. Lateral flexion is tested bilaterally. With the head in lateral flexion, the supraclavicular area on the side of flexion is palpated. The first rib is located medially in the supraclavicular area. The patient is asked to breathe in, and the first rib rises against the pressure of the examining finger. Pain may be elicited locally. Paraesthesiae in the C8 or T1 areas may be reported.
There are a variety of special tests (Table 1)
| Thoracic Outlet Syndrome Tests | |||||
|---|---|---|---|---|---|
| Test | Sensitivity | Specificity | +LR | -LR | Kappa |
| Cervical Rotation Lateral Flexion Test[3] | 0.92 | 0.90 | 9.2 | 0.09 | 1.0 |
| Both Adson + Wright (pulse) positive | 0.54 | 0.94 | 9.0 | 0.5 | |
| Both Adson + hyperabduction (sx) positive | 0.72 | 0.88 | 6 | 0.3 | |
| Hyperabduction (pulse abolition) | 0.52 | 0.90 | 5.2 | 0.5 | |
| Both Adson + Roos positive | 0.72 | 0.82 | 4 | 0.3 | |
| Both Adson + Wright (sx) positive | 0.79 | 0.76 | 3.3 | 0.3 | |
| Both Adson + Roos positive | 0.72 | 0.82 | 4 | 0.3 | |
| Adson test | 0.79 | 0.76 | 3.3 | 0.3 | |
| Tinel sign | 0.86 | 0.56 | 2.0 | 0.3 | |
| Both Wright (pulse) + hyperabduction (sx) positive | 0.63 | 0.69 | 2.0 | 0.5 | |
| Both Wright (sx) + hyperabduction (sx) positive | 0.83 | 0.50 | 1.7 | 0.3 | |
| Both Wright (sx) + Roos positive | 0.83 | 0.47 | 1.6 | 0.4 | |
| Wright test (pulse abolition) | 0.70 | 0.53 | 1.5 | 0.6 | |
| Hyperabduction (sx reproduction) | 0.84 | 0.40 | 1.4 | 0.4 | |
| Wright test (sx reproduction) | 0.90 | 0.29 | 1.3 | 0.3 | |
| Roos test | 0.84 | 0.30 | 1.2 | 0.5 | |
Investigations
Electrophysiological tests are typically normal below the clavicle. However in some cases there may be the following findings in classic neurogenic TOS:
- Low compound muscle action potential in the thenar and intrinsic muscles
- Abnormal sensory nerve conduction in the ulnar nerve
- Prolonged F-wave latency in the ulnar nerve
- Abnormal medial antebrachial cutaneous sensory nerve conduction)
Plain films can be used to assess for an extra cervical rib
Venous and arterial anatomy can be assessed by catheter angiography, doppler, or MR angiography and venography.
Differential Diagnosis
- Rotator Cuff Tendinopathy
- Cervical disc disorders
- C7 or C8 nerve root compression
- Ulnar neuropathy
- Carpal Tunnel Syndrome
- Fibromyalgia
- Multiple Sclerosis
- CRPS
- Syringomyelia
Treatment
Nonsurgical treatment
Malfunction of the first rib: isometric contraction of scalenus anterior and medius results in elevation of the first rib anteriorly, and reduces posterior subluxation. The therapist places their hand over the lateral head with the patient in a seated position. The patient contracts against the therapists hand. Gentle mobilisations are done over 20 seconds.
Postural dysfunction: Spinal postural stability; release tight pectoralis minor (pec minor may be tight without 1st rib dysfunction with arm elevation), scalene and shoulder girdle muscles (e.g. infraspinatus and teres minor); maintain cervicothoracic mobility; strengthen scapula muscles, lower and middle trapezius, and serratus anterior; strengthen rotator cuff; address ergonomic factors; address work behaviour factors.
Injections:
See Also
Reporting standards are by Illig et al. [4]
References
- ↑ Juvonen T, Satta J, Laitala P, Luukkonen K, Nissinen J. Anomalies at the thoracic outlet are frequent in the general population. Am J Surg. 1995 Jul;170(1):33-7. doi: 10.1016/s0002-9610(99)80248-7. PMID: 7793491.
- ↑ Gillard et al.. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint bone spine 2001. 68:416-24. PMID: 11707008. DOI.
- ↑ Lindgren KA, Leino E, Manninen H. Cervical rotation lateral flexion test in brachialgia. Arch Phys Med Rehabil. 1992 Aug;73(8):735-7. PMID: 1642524.
- ↑ Illig et al.. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. Journal of vascular surgery 2016. 64:e23-35. PMID: 27565607. DOI.
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,