Intersection Syndrome: Difference between revisions
| Line 29: | Line 29: | ||
==Epidemiology and Risk Factors== | ==Epidemiology and Risk Factors== | ||
The condition is considered to be rare. For example in a study of 1,131 patients referred for wrist ultrasound, intersection syndrome was only identified in 21 cases (1.9%).<ref name=":0">{{Cite journal|last=Draghi|first=Ferdinando|last2=Bortolotto|first2=Chandra|date=2014-03|title=Intersection syndrome: ultrasound imaging|url=http://link.springer.com/10.1007/s00256-013-1786-1|journal=Skeletal Radiology|language=en|volume=43|issue=3|pages=283–287|doi=10.1007/s00256-013-1786-1|issn=0364-2348}}</ref> In another study of 1,815 MRI examinations of the wrist and forearm, intersection syndrome was only identified in 3 cases (0.2%).<ref name=":1">{{Cite journal|last=Costa|first=C. Rosalia|last2=Morrison|first2=William B.|last3=Carrino|first3=John A.|date=2003-11|title=MRI features of intersection syndrome of the forearm|url=https://pubmed.ncbi.nlm.nih.gov/14573413|journal=AJR. American journal of roentgenology|volume=181|issue=5|pages=1245–1249|doi=10.2214/ajr.181.5.1811245|issn=0361-803X|pmid=14573413}}</ref> | The condition is considered to be rare. For example in a study of 1,131 patients referred for wrist ultrasound, intersection syndrome was only identified in 21 cases (1.9%).<ref name=":0">{{Cite journal|last=Draghi|first=Ferdinando|last2=Bortolotto|first2=Chandra|date=2014-03|title=Intersection syndrome: ultrasound imaging|url=http://link.springer.com/10.1007/s00256-013-1786-1|journal=Skeletal Radiology|language=en|volume=43|issue=3|pages=283–287|doi=10.1007/s00256-013-1786-1|issn=0364-2348}}</ref> In another study of 1,815 MRI examinations of the wrist and forearm, intersection syndrome was only identified in 3 cases (0.2%).<ref name=":1">{{Cite journal|last=Costa|first=C. Rosalia|last2=Morrison|first2=William B.|last3=Carrino|first3=John A.|date=2003-11|title=MRI features of intersection syndrome of the forearm|url=https://pubmed.ncbi.nlm.nih.gov/14573413|journal=AJR. American journal of roentgenology|volume=181|issue=5|pages=1245–1249|doi=10.2214/ajr.181.5.1811245|issn=0361-803X|pmid=14573413}}</ref> In a prospective study of 8080 patients with arm or hand pain in Thailand, intersection syndrome was found in 30 patients (0.37%).<ref name=":3">{{Cite journal|last=Pantukosit|first=S.|last2=Petchkrua|first2=W.|last3=Stiens|first3=S. A.|date=2001-09|title=Intersection syndrome in Buriram Hospital: a 4-yr prospective study|url=https://pubmed.ncbi.nlm.nih.gov/11523968|journal=American Journal of Physical Medicine & Rehabilitation|volume=80|issue=9|pages=656–661|doi=10.1097/00002060-200109000-00005|issn=0894-9115|pmid=11523968}}</ref> | ||
In sport-people common culprits are heavy lifting, rowing, skiing, and racket sports. The highest risk is when beginning a new sport. The dominant hand is more commonly affected. It can also occur occupationally for example in typists and carpenters. | Most patients are male,<ref name=":3" /> in contrast to de Quervains. In sport-people common culprits are heavy lifting, rowing, skiing, and racket sports. The highest risk is when beginning a new sport. The dominant hand is more commonly affected. It can also occur occupationally for example in typists and carpenters. | ||
==Clinical Features== | ==Clinical Features== | ||
===History=== | ===History=== | ||
The pain is located radially but is slightly more proximal and dorsal than [[De Quervain Tendinopathy|de Quervains]]. They will typically also report a "squeaking" sensation with wrist and thumb movement. | The pain is located radially but is slightly more proximal and dorsal than [[De Quervain Tendinopathy|de Quervains]]. They will typically also report a "squeaking" sensation with wrist and thumb movement. In the prospective study where 30 patients were identified, symptoms were swelling (73.3%), crepitus (40%), pain with radial deviation (46.7%), pain with pulling (13.3%), and pain with a combination of hand movements (40%).<ref name=":3" /> Patients tend to present acutely.<ref name=":3" /> | ||
===Examination=== | ===Examination=== | ||
| Line 61: | Line 61: | ||
* Rest - The condition is commonly self-limited. | * Rest - The condition is commonly self-limited. | ||
* Activity modification | * Activity modification | ||
* Bracing (wrist splint in | * Bracing (wrist splint in 15 degrees extension)<ref name=":3" /> | ||
* Stretching | * Stretching | ||
* NSAIDs | * NSAIDs | ||
* Injections - Corticosteroid injection into the tendon sheath of the second compartment at the area of maximal tenderness. Prolotherapy has also been described.<ref name=":2">{{Cite journal|last=Schmidt|first=Eric|last2=Kobayashi|first2=Yuka|last3=Gottschalk|first3=Andrew W.|date=2021|title=It's Not De Quervain Tenosynovitis - A Diagnosis to Consider in Persistent Wrist Pain|url=https://pubmed.ncbi.nlm.nih.gov/34239368|journal=Ochsner Journal|volume=21|issue=2|pages=120–122|doi=10.31486/toj.21.0005|issn=1524-5012|pmc=8238112|pmid=34239368}}</ref> | * Injections - Corticosteroid injection into the tendon sheath of the second compartment at the area of maximal tenderness. Prolotherapy has also been described.<ref name=":2">{{Cite journal|last=Schmidt|first=Eric|last2=Kobayashi|first2=Yuka|last3=Gottschalk|first3=Andrew W.|date=2021|title=It's Not De Quervain Tenosynovitis - A Diagnosis to Consider in Persistent Wrist Pain|url=https://pubmed.ncbi.nlm.nih.gov/34239368|journal=Ochsner Journal|volume=21|issue=2|pages=120–122|doi=10.31486/toj.21.0005|issn=1524-5012|pmc=8238112|pmid=34239368}}</ref> | ||
* Surgery. This involves release of the second extensor compartment. | * Surgery. This involves release of the second extensor compartment. This is only very rarely required. In the prospective study of 30 patients, none required surgery.<ref name=":3" /> | ||
==Follow Up and Prognosis== | ==Follow Up and Prognosis== | ||
The prognosis is generally good. | The prognosis is generally good.<ref name=":3" /> | ||
==Summary== | ==Summary== | ||
| Line 77: | Line 77: | ||
[[Category:Tendinopathies]] | [[Category:Tendinopathies]] | ||
[[Category:Hand and Wrist Conditions]] | [[Category:Hand and Wrist Conditions]] | ||
{{Reliable sources}} | {{Reliable sources}} | ||
Revision as of 09:29, 12 May 2024
| |
| Intersection Syndrome | |
|---|---|
| Synonym | peritendinitis crepitans, crossover syndrome, adventitial bursitis, subcutaneous perimyositis with abductor pollicis longus syndrome and bugaboo forearm. |
| Epidemiology | Rare |
| Classification | Proximal and distal forms. |
| Risk Factors | Sports and occupational |
| DDX | De Quervain Tendinopathy |
| Treatment | Rest, activity modification, wrist splinting, injection |
| Prognosis | Good |
Intersection syndrome is an uncommon overuse disorder of the forearm.
Aetiopathophysiology
Intersection syndrome is an overuse injury caused by repetitive wrist extension. There are two forms - the more common proximal form, and less common distal form.
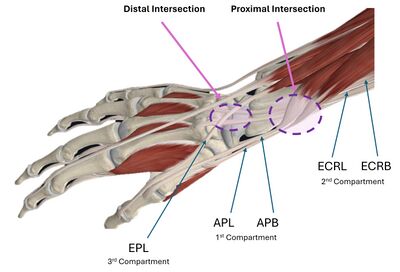
Proximal Intersection Syndrome
In the proximal form the affected location is where the musculotendinous junctions of the first compartment containing abductor pollicis longus (APL) and extensor pollicis brevis (EPB) cross over the tendons of the second compartment containing extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB). These two compartments intersect at an angle of approximately 60 degrees located 4-8cm proximal to Lister's tubercle.[2]
One theory is that the syndrome is caused by frictions between the muscle bellies of first compartment cross over the tendons of the second compartment. A second theory is that there is entrapment of muscles in the second compartment secondary to stenosis - a "stenosing tenosynovitis".
Distal Intersection Syndrome
There is a rarer distal intersection site that has been much more recently described than the proximal form. In the distal form the affected site is where the third extensor compartment tendon intersects with the second extensor compartment tendons. It is hypothesised that this form is related to the "biomechanical pulley effect" that Lister's tubercle has on the EPL tendon.[3]
Epidemiology and Risk Factors
The condition is considered to be rare. For example in a study of 1,131 patients referred for wrist ultrasound, intersection syndrome was only identified in 21 cases (1.9%).[4] In another study of 1,815 MRI examinations of the wrist and forearm, intersection syndrome was only identified in 3 cases (0.2%).[2] In a prospective study of 8080 patients with arm or hand pain in Thailand, intersection syndrome was found in 30 patients (0.37%).[5]
Most patients are male,[5] in contrast to de Quervains. In sport-people common culprits are heavy lifting, rowing, skiing, and racket sports. The highest risk is when beginning a new sport. The dominant hand is more commonly affected. It can also occur occupationally for example in typists and carpenters.
Clinical Features
History
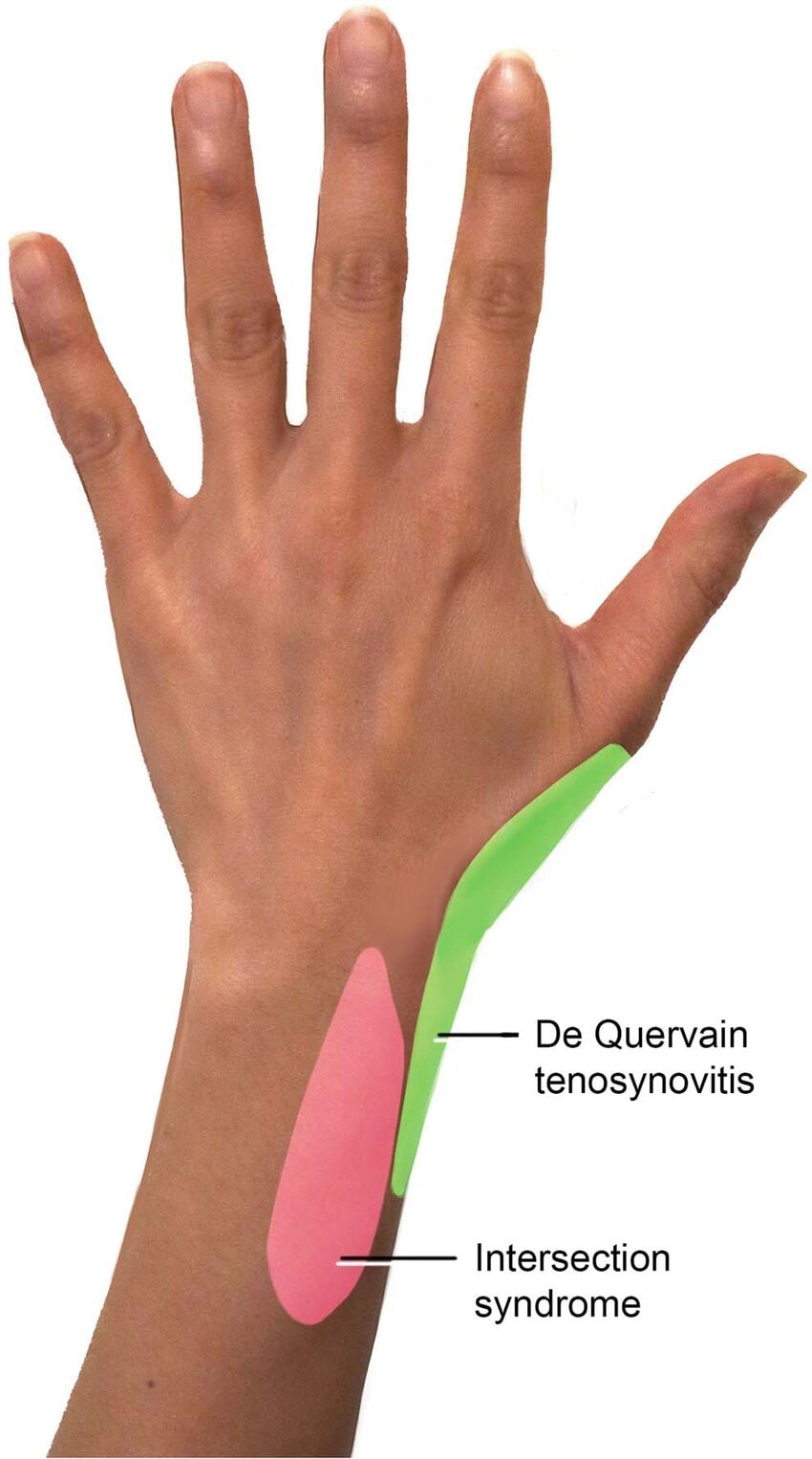
The pain is located radially but is slightly more proximal and dorsal than de Quervains. They will typically also report a "squeaking" sensation with wrist and thumb movement. In the prospective study where 30 patients were identified, symptoms were swelling (73.3%), crepitus (40%), pain with radial deviation (46.7%), pain with pulling (13.3%), and pain with a combination of hand movements (40%).[5] Patients tend to present acutely.[5]
Examination
Swelling and redness may be noted compared to the contralateral side. Pay careful attention to the location of tenderness to avoid misdiagnosis as de quervains - they should not be tender over the radial styloid. More prominent movement of the thumb is required to reproduce the pain in comparison to de quervains. Wrist extension and radial deviation may reproduce pain. Squeaking or crepitus may be noted at the site. Auscultation can be performed over the area of pain while the patient flexes and extends their wrist.
Investigations
Ultrasound and/or MRI can confirm the diagnosis.
In proximal intersection syndrome there is an effusion within the second extensor compartment tendon sheath and occasionally also within the first osseofibrous tunnel sheath. Less frequently there is oedema or a bursitis between the two tendon groups. In distal intersection syndrome common findings are tenosynovitis, soft tissue oedema, and bursitis.[4] MRI shows peritendinous oedema.[2]
Diagnosis
The diagnosis is made on clinical features, however imaging can be supportive. Some clinicians prefer confirmation on imaging due to the low prevalence.[4]
Differential Diagnosis
- De Quervain Syndrome
- Scaphoid fracture
- Osteoarthritis of the first metacarpal joint
- Ganglion cyst
- Wartenderg syndrome
- Sprain
Treatment
- Rest - The condition is commonly self-limited.
- Activity modification
- Bracing (wrist splint in 15 degrees extension)[5]
- Stretching
- NSAIDs
- Injections - Corticosteroid injection into the tendon sheath of the second compartment at the area of maximal tenderness. Prolotherapy has also been described.[1]
- Surgery. This involves release of the second extensor compartment. This is only very rarely required. In the prospective study of 30 patients, none required surgery.[5]
Follow Up and Prognosis
The prognosis is generally good.[5]
Summary
References
- ↑ 1.0 1.1 Schmidt, Eric; Kobayashi, Yuka; Gottschalk, Andrew W. (2021). "It's Not De Quervain Tenosynovitis - A Diagnosis to Consider in Persistent Wrist Pain". Ochsner Journal. 21 (2): 120–122. doi:10.31486/toj.21.0005. ISSN 1524-5012. PMC 8238112. PMID 34239368.
- ↑ 2.0 2.1 2.2 Costa, C. Rosalia; Morrison, William B.; Carrino, John A. (2003-11). "MRI features of intersection syndrome of the forearm". AJR. American journal of roentgenology. 181 (5): 1245–1249. doi:10.2214/ajr.181.5.1811245. ISSN 0361-803X. PMID 14573413. Check date values in:
|date=(help) - ↑ Parellada, Antoni J.; Gopez, Angela G.; Morrison, William B.; Sweet, Stephanie; Leinberry, Charles F.; Reiter, Sean B.; Kohn, Mark (2007-01-26). "Distal intersection tenosynovitis of the wrist: a lesser-known extensor tendinopathy with characteristic MR imaging features". Skeletal Radiology (in English). 36 (3): 203–208. doi:10.1007/s00256-006-0238-6. ISSN 0364-2348.
- ↑ 4.0 4.1 4.2 Draghi, Ferdinando; Bortolotto, Chandra (2014-03). "Intersection syndrome: ultrasound imaging". Skeletal Radiology (in English). 43 (3): 283–287. doi:10.1007/s00256-013-1786-1. ISSN 0364-2348. Check date values in:
|date=(help) - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Pantukosit, S.; Petchkrua, W.; Stiens, S. A. (2001-09). "Intersection syndrome in Buriram Hospital: a 4-yr prospective study". American Journal of Physical Medicine & Rehabilitation. 80 (9): 656–661. doi:10.1097/00002060-200109000-00005. ISSN 0894-9115. PMID 11523968. Check date values in:
|date=(help)
Literature Review
- Reviews from the last 7 years: review articles, free review articles, systematic reviews, meta-analyses, NCBI Bookshelf
- Articles from all years: PubMed search, Google Scholar search.
- TRIP Database: clinical publications about evidence-based medicine.
- Other Wikis: Radiopaedia, Wikipedia Search, Wikipedia I Feel Lucky, Orthobullets,