Acute Neck Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{stub}} | |||
==Clinical Assessment== | ==Clinical Assessment== | ||
{{Red flags| | {{Red flags| | ||
Revision as of 13:38, 24 May 2021
Clinical Assessment
- Trauma
- Constitutional: Fever, night sweats, weight loss, history of cancer, immunosuppression, pain elsewhere, illicit drug use
- Iatrogenic: Recent surgery, catheterisation, venipuncture, manipulation
- Awkward posture
- Exotic exposure or recent overseas travel
- Neurological: Symptoms/signs, vomiting
- Cardiovascular: Risk factors, anticoagulants
- Genitourinary/Reproductive: UTI, haematuria, retention, uterine, breast
- Endocrine: Corticosteroids, diabetes, hyperparathyroid
- Gastrointestinal: Dysphagia
- Integumentary: Infections, rashes
- Respiratory: Cough, haemoptysis
It is rarely possible to establish a patho-anatomic diagnosis in acute neck pain, and so the diagnostic process is one of exclusion.
The first step is evaluating whether the patient has neurological symptoms or signs. If they do then they should be assessed under a neurological disorders framework rather than an acute neck pain framework as the neurological disorder takes precedence. Neurological disorders include spinal cord injury, myelopathy, and radiculopathy.
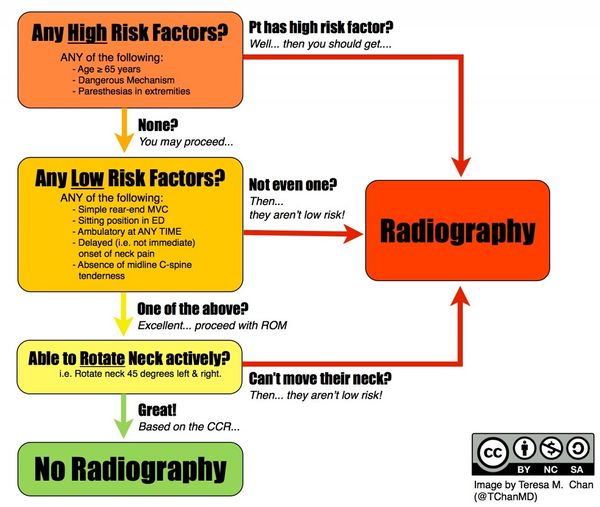
In the event of trauma, the Canadian C-spine rule should be used, and any fracture managed as appropriate.
Diagnosis
For patients with no history of injury the diagnosis used by the Australian Acute Musculoskeletal Guidelines is "idiopathic neck pain," while for those with neck pain following a motor vehicle accident the diagnosis is "whiplash-associated neck pain." For ACC medicolegal purposes the coding that should be used is normally "cervical sprain," but this is not a meaningful label in a medical sense as it lacks legitimacy as a diagnosis.
Management
Passive Treatment
Passive treatment is avoided. It is not effective, especially when compared to other methods. Passive management assumes that a specific diagnosis has been made, and that passive treatment will rectify said diagnosis. However no conventional examination or investigation can identify the pathology and no conventional treatment can target or resolve any specific cause of pain
Explanation and Reassurance
These often go together. Elicit the patient's ideas and concerns. Gently correct false beliefs and address any fears about serious causes or about the prognosis. A clinical assessment can effectively rule out sinister causes and so the clinician can provide reassurance based on sound evidence. The patient many not have any specific concerns or fears. Regardless the clinician should fully reassure the patient that serious causes of neck pain are rare and can be recognised on clinical assessment, and common causes are not threatening and have a good prognosis. The clinician should be truthful that in the majority of cases no one knows what causes the pain, that it is probably something simple like a sprain or sore muscles, but that there is no simple way to make an exact diagnosis. Explain that even without treatment most patients recover, and that the most effective treatment is a tincture of time. However offer other measures as below to help the process along.
Activation
Simple Exercises
Analgesia
Bibliography
- Bogduk, Nikolai, and Brian McGuirk. Management of acute and chronic neck pain : an evidence-based approach. Edinburgh New York: Elsevier, 2006.